A Case Report on Intraorbital Extraconal Dermoid Cyst
A B S T R A C T
Orbital dermoid cyst represents 3 to 4% of all primary orbital tumors. The intraorbital location is relatively rare and it commonly occurs at childhood. We reported the case of a 4-year-old male child with an intraorbital dermoid cyst, who presented with progressive left proptosis, which had noticed 6 months earlier. Visual acuity, ocular motility and fundoscopic examination were normal. Magnetic resonance Imaging (MRI) revealed an extraconal orbital mass situated on superior & mildly posterior aspect of orbit and which was iso-to-hypointense in T1, hyperintense in T2, restriction of diffusion in DWI, hyperintense signal on ADC (Shine through) and no enhancement after giving contrast. The tumor was completely excised via a left fronto-orbital access. Histopathologically, the tumor was confirmed as dermoid cyst.
Keywords
Dermoid cyst, intraorbital, MRI, surgery
Introduction
Dermoid cysts are squamous epithelium-lined sacs that result from abnormal migration of ectodermal cells. These cysts are composed of keratinized stratified squamous epithelium, have a fibrous capsule, and also have skin appendices like sweat glands, sebaceous glands and hair follicles [1]. Both dermoid and epidermoid are lined by keratinized stratified squamous epithelium and have a fibrous wall but A dermoid has dermal appendages, whereas an epidermoid has none [2]. Orbital dermoid cyst represents 3 to 4% of all primary orbital tumors. The intraorbital location is relatively rare [3]. Dermoid cysts are common orbital masses in childhood. Most cysts are present at birth or in the first 3 months of life. Patients usually present with mass lesion or proptosis [4]. Inflammatory reaction in surrounding tissues as the result of leakage of cyst content may rarely be the reason for admission. They should be surgically removed at ages 1 - 2 as they may enlarge and lead to deformation in orbital bony structures and erosion [5].
Good quality imaging (MRI) plays a major role in the etiological diagnosis, providing a precise analysis of the location of the lesion, its components, and its effects on adjacent and nearby structures, as well as in planning the surgical approach [6].
Case Report
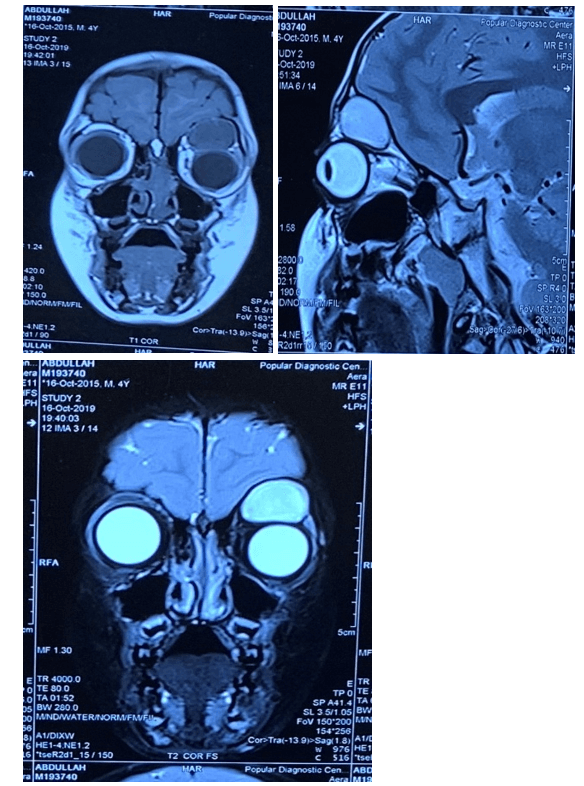
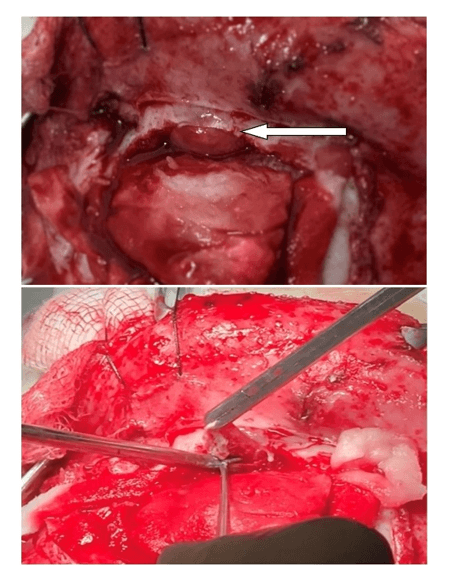
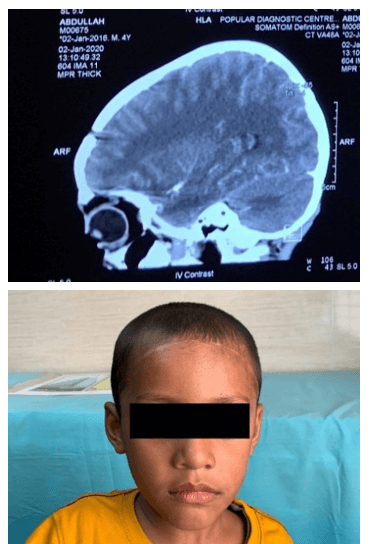
A 4-year-old male child presented with progressive left proptosis, which had noticed 6 months earlier. Visual acuity, ocular motility and funduscopic examination were normal. Magnetic Resonance Imaging (MRI) revealed an extraconal intraorbital dermoid (2.1 x 1.75 x 1.75 cm) situated on superior & mildly posterior aspect of orbit and which was iso-to-hypointense in T1, hyperintense in T2 (Figure 1), restriction of diffusion in DWI, hyperintense signal on ADC (Shine through) and no enhancement after giving contrast (Figure 2). The tumor was completely excised via a left fronto-orbital access (Figure 3). Histopathologically, the tumor was confirmed as dermoid cyst. Postoperative CT (Computerized Tomography) scan revealed no residual dermoid cyst (Figure 4).
Figure 1: T1 weighted coronal & T2 weighted sagital & coronal MRI showed left Intraorbital extraconal dermoid.
Figure 2: MRI contrast sagital & DWI & ADC showed left intraorbital dermoid.
Figure 3: Per-operative view of dermoid tumor.
Figure 4: Postoperative CT scan showed no residual dermoid cyst & present status of the patient.
Discussion
Dermoid cysts are abnormally located masses arising from abnormal involution of superficial ectoderm during closure of sutures between bones [1]. This cyst is the commonly used clinical term for benign cystic teratoma, derived from sequestration of surface ectoderm into underlying mesenchyme along embryonic lines of closure [2].
Dermoid cysts occur predominantly in children, with few reported cases in the literature in adults [7]. They are presented in more superficial or periorbital forms with precocious clinical presentation and diagnosis, as well as in deeper or intraorbital forms, which usually progress for a long period until clinical manifestations arise and the diagnosis is established [8]. When found in the intraorbital region, they mainly occupy the upper lateral quadrant of the orbit, and its clinical presentation depends on the exact location and size of the tumor [9]. They are usually slow-growing lesions, but they can progress more rapidly if they affect people during adulthood. The deepest forms of the dermoid cyst commonly manifested with a progressive proptosis [8]. In some cases, the cyst may compress the optic nerve, impairing the visual acuity of the affected side, or manifest itself also associated with inflammatory complications or hemorrhagic complications [10].
Image exams such as CT (Computed Tomography) and Magnetic Resonance (MRI) help in the diagnosis of dermoid cysts. Computed tomography (CT) usually performed preoperatively in order to determine the presence of intracranial extension of cysts and orbital bone defect. Magnetic resonance imaging (MRI) is beneficial for detection of cyst content and differential diagnosis. CT images usually present the cyst as hypodense lesions and not highlighted by contrast, and may present calcifications; in MRI, it commonly presents hyposignal in T1 and hypersignal in T2, restriction of diffusion in DWI & hypersignal in ADC, characteristics that were observed in the reported case; in both exams, it may show evidence of the presence of oily contents [11]. Diagnostic confirmation occurs through histopathological examination of the lesion, that characterizes a laminated pavement epithelial wall and a heterogeneous content with dermal appendages that also observed in our case [12].
The principle of treatment in dermoid cyst reported in the literature is the complete removal of the mass [3, 6]. Traditional treatment is excision of the mass with an incision over the mass. After this incision, long-standing erythema and sometimes a bad looking sunk scar may remain due to thickness of the skin in this area. Scarring occurs more in children as the skin is tight in children. Incisions through, below or above the brow are used to remove these cysts. Although the scar incision is hidden in the brow in this incision, alopecia and deformity may develop [13]. The best option for deep intraorbital dermoid cyst, the cyst extending into frontal sinus or cranium is bicoronal. When the lesion is intraorbital, the procedure involves complex techniques, due to the distinct anatomy and fragility of the orbital structures and depends, among other aspects, on the location and extent of the lesion, as well as the experience of the surgeon who performs the procedure [12]. In the case reported, the chosen access was left fronto-orbital access followed by osteotomies on the orbital roof. Similar access was used in the approach reported by Taha et al. [3].
Cyst rupture is a complication that should be avoided mostly. Cyst content should be removed from wound site by washing with abundant saline solution [8].
Conclusion
Intra-orbital dermoid cysts are rare lesions, which results in a few case reports regarding the approaches of these lesions. Thus, it is essential to add multicenter knowledge and to establish more holistic approaches for these neoplasms and satisfying the surgical demands to guarantee the cure.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Tue 26, May 2020Accepted: Tue 09, Jun 2020
Published: Wed 17, Jun 2020
Copyright
© 2023 Saumitra Sarkar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.06.15
Author Info
Dey A Hasan SMS Hossen MK Rashid HU Sarkar S Saumitra Sarkar
Corresponding Author
Saumitra SarkarDepartment of Neurosurgery, Shaheed Suhrawardy Medical College, Dhaka, Bangladesh
Figures & Tables

References
- Shepherd G Pryor, Jean E Lewis, Amy L Weaver, Laura J Orvidas (2005) Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg 132: 938-942. [Crossref]
- T Civit, A Joud, O Klein (2010) Congenital orbital tumors in adults (dermoid cysts). Neurochirurgie 56: 183-186. [Crossref]
- Taha S, Doe K, Compeyre S, Nogues L, Lopes M et al. (2009) Intraorbital Dermoid Cyst: Case Report. Neurochirurgie 55: 577-580.
- Jerry A Shields, Carol L Shields (2004) Orbital cysts of childhood--classification, clinical features, and management. Surv Ophthalmol 49: 281-299. [Crossref]
- Cavazza S, Laffi GL, Lodi L, Gasparrini E, Tassinari G (2011) Orbital dermoid cyst of childhood: clinical pathologic findings, classification and management. Int Ophthalmol 31: 93-97.
- Kose R (2017) Excision of Orbital Dermoid Cysts via Upper Eyelid Incision: A Review of 24 Cases. Natl J Maxillofac Surg 8: 167-169.
- Nguyen Si Pham, Arthur Brooks Dublin, Edward Bradley Strong (2010) Dermoid cyst of the orbit and frontal sinus: a case report. Skull Base 20: 275-278. [Crossref]
- Meenakshi Yeola, S R Joharapurkar, A M Bhole, Manisha Chawla, Sumit Chopra et al. (2009) Orbital floor dermoid: an unusual presentation. Indian J Ophthalmol 57: 51-52. [Crossref]
- Ellen M Chung, Mark D Murphey, Charles S Specht, Regino Cube, James G Smirniotopoulos (2008) From the archives of the AFIP pediatric orbit tumors and tumorlike lesions: osseous lesions of the orbit. Radiographics 28: 1193-1214. [Crossref]
- Imtiaz A. Chaudhry (2008) Management of deep orbital dermoid cysts. Middle East Afr J Ophthalmol 15: 43-45. [Crossref]
- Won Sang Jung, Kook Jin Ahn, Mi Ra Park, Ji Young Kim, Jae Jeong Choi et al. (2007) The radiological spectrum of orbital pathologies that involve the lacrimal gland and the lacrimal fossa. Korean J Radiol 8: 336-342. [Crossref]
- H Zaghouani Ben Alaya, M Gaha, Y Limem, W Karmani, Z Mziou et al. (2013) Intraorbital Dermoid Cyst. Case Report and Review of the Literature. J Fr Ophtalmol 36: 172-177. [Crossref]
- Park AH, Siddiqi F (2006) An approach to pediatric brow dermoids: an upper eyelid crease incision. Int J Pediatr Otorhinolaryngol 70: 349-351.
