A “Floating Glenoid” after a Reverse Total Shoulder Arthroplasty: A Case Report with Literature Review
A B S T R A C T
A shoulder replacement for cuff tear arthropathy was the original indication of the reverse total shoulder arthroplasty (rTSA). However, over time, this particular concept of shoulder arthroplasty has found new indications for other pathologies such as complex proximal humeral fractures and irreparable rotator cuff tears with rotator cuff arthropathy. Retensioning of the deltoid muscle is a vital step during this procedure in order to restore active elevation however, this can be potentially problematic since it results in anatomical changes and often times increases the stress forces across the acromion. We experienced a rare case of an 84-year-old female presenting with an extensive fracture resulting in a “floating glenoid” after reverse total shoulder arthroplasty via a deltopectoral approach. In our case, the patient presented with gradual onset pain in the posterior shoulder with point tenderness over the acromion, which worsened during active joint movement. The patient was definitively managed with surgical removal of the glenoid implants and conversion to a hemiarthroplasty. While there are existing strategies for preventing fractures of this nature, further research is still necessary to establish best management guidelines of these fracture complications associated with rTSA in order to achieve optimal outcomes.
Keywords
Stress fracture, reverse total shoulder arthroplasty, glenoid
Introduction
Reverse total shoulder arthroplasty (rTSA) has become the treatment of choice for patients with rotator cuff arthropathy. Complication rates after rTSA have been reported as being up to three to five times that of conventional total shoulder arthroplasty. Intraoperative and postoperative complications include neurological injury, infection, dislocation or instability, acromial or scapular spine fracture, hematoma, and scapular notching. In reverse total shoulder arthroplasty, increased tensioning of the deltoid muscle is essential for improving active elevation. However, these anatomical changes along with pre-existing factors of the underlying condition itself may potentially produce unique complications such as acromial and scapular spine fractures. We present a case of management of a rare case presentation of multiple non-traumatic fractures around the glenoid after reverse total shoulder arthroplasty via a deltopectoral approach. The management involved conversion of surgery to a hemiarthroplasty. We also present a review of the literature.
Case Report
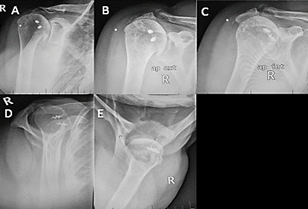
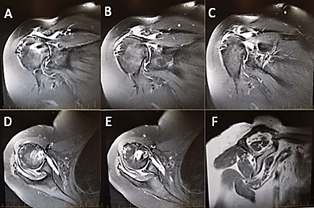
An 84-year-old, right-hand dominant female was seen in consultation with a four-month history of a painful right shoulder with gradually deteriorating function after pulling a garden hose. She had previously undergone bilateral mini-open repairs of rotator cuff tears approximately ten years prior to presentation. An acromioplasty was performed on the right side at the time of the rotator cuff repair. Three years earlier, she had undergone a left reverse total shoulder replacement for rotator cuff arthropathy. Good passive movement of the glenohumeral joint was demonstrated. However, there was a marked weakness of the supraspinatus and infraspinatus muscles with limited active movement. Plain radiographs of the right shoulder showed classic findings of glenohumeral degeneration and marked superior migration of the right humeral head in keeping with rotator cuff arthropathy (Figure 1). Magnetic resonance imaging (MRI) revealed a massive rotator cuff tear involving the supraspinatus, infraspinatus and subscapularis tendons (Figure 2). Of significance, she developed deterioration in clinical function one year after the left rTSA and was diagnosed with a stress fracture of the left acromion. This was managed conservatively with rest and immobilization in abduction. Repeat imaging showed evidence of the healed fracture.
Figure 1: Plain radiographs [A) anteroposterior, B) external rotation, C) internal rotation D) trans-scapular and E) axillary views] of right shoulder showing significant rotator cuff arthropathy with proximal migration of the humeral head. Suture anchors are noted in the lesser tuberosity in keeping with previous rotator cuff repair.
Figure 2: T2 weighted MRI scan demonstrating massive rotator cuff tear involving Supraspinatus, and Infraspinatus (A-E) with significant fatty degeneration of the supraspinatus and subscapularis muscles on the T1 weighted sagittal view (F).
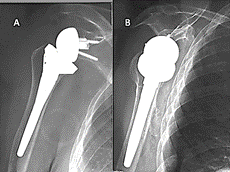
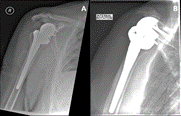
A right reverse shoulder arthroplasty was offered as the preferred treatment option. The patient subsequently underwent an uncomplicated reverse total shoulder arthroplasty two years later via a standard deltopectoral approach (Figure 3). Intraoperatively, partial attachment of the subscapularis was noted. A lesser tuberosity osteotomy was performed to mobilize the subscapularis tendon and subsequently reattached using trans-osseous non-absorbable sutures. Intraoperative range of motion demonstrated 45º of external rotation, 90º of internal rotation and 110º of abduction. She was maintained in a shoulder sling for six weeks and performed pendulum exercises three times daily. At the two-month follow-up visit, the patient comfortably demonstrated anti-gravity elevation well above shoulder level without any pain. She was maintained on a standard postoperative physiotherapy programme.
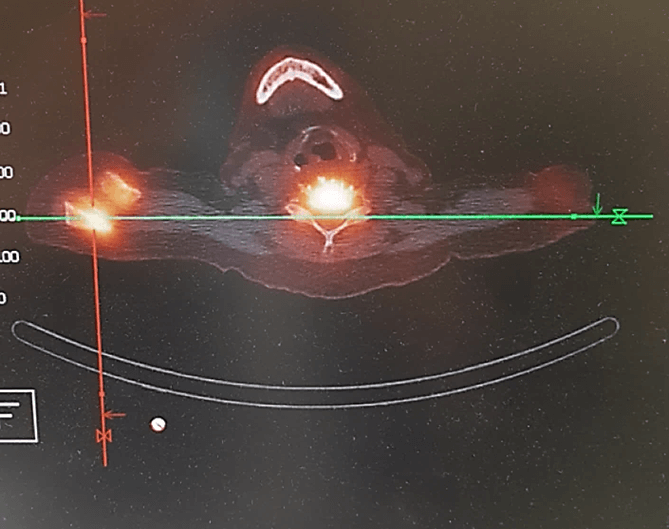
Six months after surgery, she was diagnosed with a stress reaction/fracture of the right acromion based on scintigraphic and single-photon emission computed tomography (SPECT) findings after complaining of gradual onset of right posterior shoulder pain with point tenderness over the acromion (Figures 4 & 5). She was managed conservatively with rest and an abduction pillow. Two months later, the pain had resolved and painless active elevation above shoulder level with pain-free resisted elevation was demonstrated.
Figure 3: Plain radiographs A) anteroposterior view and B) trans-scapular view showing reverse total shoulder replacement.
Figure 4: Axial single-photon emission computed tomography (SPECT) scan showing increased uptake in the right acromion, consistent with an acromial stress fracture.
Figure 5: Sagittal cuts (A & B) of SPECT CT scan showing increased uptake at glenoid believed to associated with remodeling after rTSA rather than a stress fracture.
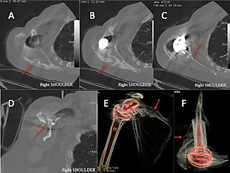
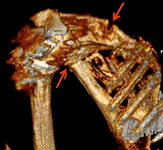
A decision was made to discontinue the abduction pillow and gradually commence regular activities. At the one-year review, the patient revealed a history of new-onset squeaking of the right shoulder with gradual declining clinical function. She denied any ongoing significant pain but admitted to pain with anti-gravity movement against resistance. Given the history of previous acromial stress fractures, clinical suspicion was raised and repeat plain radiographs and a CT scan were performed which revealed a fracture of the base of the acromion extending across the spine of the scapula and extending through the neck of the scapula resulting in a “floating” glenoid (Figures 6-8). In an effort to control her pain and prevent potential ongoing osteolysis, conversion to a hemiarthroplasty was proposed.
Figure 6: Plain radiographs (A) anteroposterior view and B) Internal rotation view) showing rTSA with glenoid component with a superolateral projected direction.
Figure 7: A-D) Axial and sagittal CT views showing fracture of scapular spine extending inferiorly involving the base of the glenoid, passing the tip of the posterior screw. E & F) 3D CT demonstrating the extent of fracture across the base of the glenoid.
Figure 8: Reconstructed CT (oblique view) showing the fracture extending from scapular spine superiorly to inferior border across the base of the glenoid.
The patient thus underwent further surgery to convert the reverse total shoulder arthroplasty to a hemiarthroplasty one week later (Figure 9). Intraoperative findings revealed evidence of metallosis and gross polyethylene wear due to impingement after the fracture; however, the glenoid baseplate was still firmly affixed to the completely separated glenoid fragment. The bone was debrided once the implants were removed, and an eccentric humeral head was placed on the humeral component. The intraoperative passive movement achieved was 90º of internal rotation and 30º of external rotation. Six weeks following the conversion, she had self-assisted elevation well above shoulder level with no pain and was comfortably back to regular driving. She continues to be monitored with serial imaging for both shoulders two years after her last surgery with no further complaints.
Figure 9: Plain radiographs (internal rotation anteroposterior and trans-scapular views) showing conversion of rTSA to a hemiarthroplasty.
Discussion
Reverse total shoulder arthroplasty (rTSA) was initially designed to address rotator cuff tear arthropathy in elderly patients but has now expanded to include other indications such as complex fractures of the proximal humerus in the elderly, irreparable rotator cuff tears without osteoarthritis, post tumor resection, revision after failed hemiarthroplasty, failure after total shoulder arthroplasty and osteoarthritis with significant posterior subluxation [1-7]. The newer implant designs allow for the distalization and medialization of the center of rotation of the shoulder joint to decrease torque at the glenoid component and recruit the deltoid muscle fibers rather than rotator cuff muscles to influence upper limb function by facilitating arm abduction and elevation [8]. Despite these obvious benefits, anatomical, physiological, and biomechanical changes to the shoulder joint after rTSA may result in complications that are not only similar to anatomical total shoulder arthroplasty (TSA) but also unique complications to rTSA [9]. Complication rates after rTSA have been reported to be three to five times that of conventional total shoulder arthroplasty, with figures reaching as high as 68% for primary rTSA [7, 10, 11]. Acromial and scapular spine fractures are among the known complications associated with rTSA. Crosby et al. retrospectively analysed 400 rTSAs and reported an incidence of scapular fractures of 5.5% (22 fractures) [12]. Molé and Favard found an incidence of 3% of acromial fractures when they reviewed 527 rTSAs [13]. In a systematic review of 782 patients, Zumstein et al. found the combined incidence of acromial and scapular fractures to be 1.5% [11].
Levy et al. classified acromial fractures into three types based on CT scans: type 1 involving a portion between the anterior and medial deltoid origin, type II involving at least the entire medial deltoid origin with a portion of the posterior deltoid, and type III involving the entire middle and posterior deltoid origin [14]. Crosby et al. reported discrete patterns of these fractures and constructed a classification scheme that placed them into three types based on the anatomical location of the fracture avulsion: (Type I) fractures of the anterior acromion; (Type II) fractures of the acromion posterior to the acromioclavicular joint; and (Type III) fractures of the scapular spine. They suggested Type I fractures should be observed, Type II fractures should undergo acromioclavicular joint resection if stable but open reduction internal fixation if unstable and Type III fractures should be treated with open reduction internal fixation [12].
Rouleau et al. proposed a further descriptive subclassification for the more medial fractures that is based on the anatomy and functionality of the scapula fractures at the scapular base. The authors termed these fractures as fractures occurring at the base of the acromion and explained that this zone functionally connects the acromion to the rest of the scapula while scapular spine fractures were reserved for those that were even more medially occurring [15]. Based on these classifications, the index case was closest to a type III fracture. We believe, however that the fracture pattern seen in the index case could not be adequately accommodated by the proposed anatomical classifications. Furthermore, these classifications, while not validated, currently are not widely used by shoulder surgeons and are based on small series of fractures. It was, therefore, impractical to use any of these classifications as a guide to the management of the index patient. As research in this area increases, it is hopeful that clarity on the nomenclature of these fractures may eventually allow for optimal treatment plans based on anatomical location.
Different explanations have been proposed for the occurrence of acromial and scapular spine fractures following rTSA. In the more common indication for rTSA, rotator cuff arthropathy, the acromion is commonly eroded from the underlying proximally migrated head secondary to a deficient rotator cuff. This can lead to insufficiency of the acromion, making it brittle or potentially already fractured. If the subscapularis muscle is intact, the erosion is posterior and may involve the scapular spine [16]. Conversely, a deficient subscapularis may influence anterior erosion. Though proximal migration of the humeral head was present in the index case, there was neither apparent preoperative radiographic evidence of acetabularization of the acromial arch, nor there were any radiographic indicators of congenital modifications of the acromion perceived to have influenced the outcome. The index patient, however, did undergo an acromioplasty some twelve years earlier and partial attachment of the subscapularis seen at surgery may have influenced subtle posterior stress on the acromion and spine, respectively, placing the index patient at a possible slightly increased risk of a stress fracture. Walch et al. however, found a 9% incidence of acromial insufficiency in 457 reverse total shoulder arthroplasties. Seventeen patients had a fracture of the acromion, 23 had os acromiale and one had a pseudarthrosis of the scapular spine. The authors showed that neither subjective nor functional results were affected by preoperative acromial pathology when compared to patients without acromial pathology [17]. Mottier et al. reported no significant difference in outcome even with a history of preoperative os acromiale or acromion stress fracture. The authors found that the Constant score was comparable to that obtained in cases with no acromial injury with the same review [18].
On the background of a commonly elderly population requiring rTSA and decreased use of a chronically dysfunctional shoulder, bone health can be seen as a significant risk factor for stress fractures after rTSA. Otto et al. assessed several clinical risk factors for scapular fractures after reverse total shoulder arthroplasty. The authors matched 53 patients with scapular fractures after rTSA with 212 control patients and found osteoporosis to be the only statistically significant risk factor for scapular fractures after rTSA (odds ratio, 1.97; 95% confidence interval, 1.00-3.91) [19]. There was no historical evidence of osteoporosis and preoperative screening for osteoporosis was not performed for the index case. Given the gender and age of the index patient, coupled with anticipated disuse osteopenia, screening for osteoporosis and possible intervention before and after rTSA may have been prudent in the management of this case. Other potential risk factors for acromial and scapular spinal fractures include the surgical approach, the deltopectoral approach in particular and previous post rTSA stress fractures of the ipsilateral shoulder [13, 19, 20]. Mayne et al. found that having had an acromial or scapular spine fracture of the ipsilateral shoulder girdle after rTSA increased the risk for other stress fractures in that patient. The authors proposed that this may be due to the increased stress on the surrounding bony and ligamentous anatomy during fracture healing and/or in the presence of a mal- or non-union of these fractures [20]. This suggests that the risk of the subsequent scapular spine fracture in the case presented increased with the history of the previous acromial stress fracture on the ipsilateral side.
The type, size, length and trajectory of screws in rTSA have all been evaluated for improvement in fixation and micromotion of the glenoid baseplate. The use of variable‐angle locking screws has been advocated so that the trajectory can be aimed toward the denser bony regions such as the scapular spine and the coracoid base [15]. Screw fixation has since come under scrutiny as a possible contributing factor to the development of acromial and scapular fractures after rTSA. Crosby et al. recommended avoiding the superior screw in the metaglene for baseplate fixation after three-dimensional CT scans revealed that the superior screw was a potential stress riser [12]. Similarly, Mayne et al. suggested that this superior screw is a potential risk for creating a stress riser in the scapular spine and has the potential for breaching the spinoglenoid notch, placing the suprascapular nerve/artery at risk. The authors recommended avoiding placing this screw into the scapular spine by using a posterior screw that was ≤20mm [20]. These recommendations, however, are not validated and were based solely on the authors’ observations and vast surgical experience. Otto et al. reported a similar finding of fourteen of sixteen scapular spine fractures occurring from a screw tip. However, no correlation was identified between the occurrence of these fractures and the orientation and length of screws [19]. There is no evidence currently to support the theory that these fractures are caused by the actual presence of a screw but rather suggest that the fracture pattern, when they do occur, may be influenced by screw position [12]. Further studies are necessary to adequately assess any correlation between the occurrence of scapular spine fractures post rTSA and baseplate screws.
Acromial fractures, in particular, may be related to the lengthening of the arm and subsequent increased tension in the deltoid muscle resulting in a stress fracture. The medialization of the center of rotation affords a significantly longer lever arm and hence the mechanical advantage of the deltoid function. In a review of the different radiographic assessments of upper extremity lengthening following rTSA, Lädermann et al. reported changes in humeral length varying from -5mm to 5mm, and changes in upper-extremity length varying from 15 mm to 27 mm [21]. These values were derived from different methods based on subjective surgical experience that was used to measure the length, as there are no standard criteria for measuring this parameter. However, deltoid muscle tension being a transmitted force is far more challenging intraoperative measurement and may be influenced by other factors such as preoperative deltoid muscle function, intraoperative relaxation and soft tissue handling.
Subsequently, Lädermann et al. devised a standardized technique to objectively measured the length of the humerus and arm preoperatively and postoperatively of 58 patients. The average postoperative lengthening of the humerus was 2mm +/- 7mm and the arm was lengthened 23mm +/- 12mm. In this study, they found no correlation between lengthening and acromial fractures. However, in cases of postoperative instability, lengthening was statistically lower. The authors recommended that subjective intraoperative criteria to evaluate deltoid tension should be replaced by objective measures to prevent insufficient or excessive deltoid tension [22]. The length of the arm in the index case was not objectively measured but was deemed adequate based on the surgeon’s extensive surgical experience and the intraoperative evaluation of range of motion and implant stability. The ideal lengthening of the arm for implant stability and function after rTSA, however, is not yet known. Furthermore, with the current paucity of standards of reporting adverse events and proper outcome studies of their management, it is extremely difficult to appreciate exactly how much tension to put in the deltoid when performing rTSA. While acknowledging that reduction in length may be beneficial in the avoidance of scapular fractures, this must be finely balanced with joint stability, another concern that always requires keen intraoperative evaluation.
The clinical presentation of acromial and scapular fractures varies in the literature. Zhou et al. suggested a typical history of sudden onset lateral shoulder pain with an associated decline in function seen in patients with acromial fractures [9]. Crosby et al., while classifying scapular fractures, indicated that patients presenting with type III fractures all have a minor traumatic event that precipitated their fractures. This presentation differed from patients with type II fractures, where the pain developed after the patients regained their shoulder movement and was not necessarily associated with a specific traumatic event [12]. Walch et al. on the other hand, while confirming a sudden deterioration in clinical function and subjective satisfaction, reported that these patients generally exhibit little pain [17]. Although the index patient gave no history of a traumatic event or significant pain, the clinical symptoms of new-onset squeaking and deteriorating function were enough indication to raise suspicion. A possible explanation for the deteriorating clinical function is the large length of the defunctioned deltoid muscle that results from the displaced fracture since the deltoid muscle is essential to the functioning of the reverse prosthesis. Therefore, surgeons should consider the possibility of acromial or scapular spine fractures in patients presenting with declining function even in the absence of pain.
There is no consensus in the literature regarding the ideal management of acromial or scapular spine fractures. Levy et al. used non-operative treatment to manage sixteen acromial fractures and found that all of them resulted in functional limitations of varying extent. Hattrup et al. on the other hand, reported improved functional outcome results with conservative management of nine acromial and scapular spine fractures with greater than 1 year of follow-up. Though improvement was seen, the functional outcome among these patients was relatively inferior to shoulders that had undergone rTSA without the development of a fracture. Mayne et al. suggested that the bony pathogenesis of these fractures comprised of a spectrum of events, with the earliest presentation being a stress reaction. This reaction then progresses to an undisplaced fracture and eventually results in a displaced fracture. Therefore, the authors recommended early diagnosis and non-operative intervention of a stress reaction or undisplaced fracture in order to prevent further displacement and potential disability [20]. Studies have shown that good outcomes may be achieved with conservative management of acromial fractures. However, more medial scapular spine fractures show a worse prognosis with non-operative treatment [12, 17, 23-25].
Based on the classification proposed by Crosby et al., surgical fixation was reserved for unstable type II fractures and all type III fractures [12]. Open reduction and internal fixation, however, is not without its challenges. Stable internal fixation around this particular location can be demanding for the orthopaedic surgeon and may result in failure of fixation, mal-unions or non-unions with varying outcomes [24, 26]. General consensus suggests conservative management for stress reactions, undisplaced or stable fractures in the region of the acromion or scapular spine region after rTSA [12, 14, 23, 26, 27]. Surgical intervention is usually employed in cases of significant displacement, instability and loosening of the glenoid component [12, 17, 25]. The use of plate and screw fixation of varying designs has been described for the treatment of unstable scapular spine fractures with reasonably good healing and functional outcomes [15]. In the index case, there was radiological evidence of healing of the initial acromial fracture with conservative management. The subsequent fracture seen was of a distinctly different origin. It can therefore be postulated that the subsequent fracture pattern seen was a result of the propagation of a stress fracture that started in the scapular spine. However, no information was found on the management of combined ipsilateral acromial and scapular spine fractures following rTSA.
No previous reports were found in the literature addressing a “floating glenoid” fracture following reverse total shoulder arthroplasty. It is our opinion that prevention rather than treatment should always be desirable for complications such as the one presented. Important preventative factors identified in the literature include the appropriate indication and proper patient selection; identification of possible risk factors such as osteoporosis and actively optimizing bone health before and after surgery; intraoperative detailing such as meticulous soft-tissue handling, proper screw placement, avoidance of levering on the acromion and over-tensioning of the deltoid.
The initial conservative management of the acromial stress fracture was in keeping with the literature and had good clinical and radiologic evidence of a favourable outcome. Risking a potentially poor outcome, we felt that the best option of management of the extensive scapular fracture was a surgical one. Adequate internal fixation of the fracture as suggested for type III fractures would have been virtually impossible. The desire to achieve pain relief influenced our decision to remove the glenosphere and baseplate. In addition, we felt that the abnormal wear pattern of the displaced glenoid component would have generated large amounts of metal and polyethylene particles with continued movement resulting in potentially devastating osteolysis in the future. Evidence of metallosis and gross polyethylene wear was seen at the time of conversion surgery, supporting our concerns.
Conclusion
Expanding surgical indications have led to the increasing use of rTSA and therefore, further research is necessary to establish best management practices of these fracture complications associated with rTSA in order to achieve optimal outcomes. To the best of our knowledge, this is the first documented case of this fracture pattern. Currently, no evidence exists to recommend routine or widespread screening for osteoporosis before routine primary rTSA. The best treatment option for acromial and scapular spine fractures after rTSA remains uncertain. Available data comprised of several small retrospective, single surgeon, single-institution case reports and series, lacked standardized definitions of complications and proper protocols for the reporting of adverse events. We, however, believe that early diagnosis and prompt treatment are necessary to halt ongoing clinical problems and to prevent further deterioration. We are of the opinion that for a fracture of this nature, resulting in a small compromised glenoid fragment on the background of osteopenia/osteoporosis, surgical removal of the glenoid implants and conversion to a hemiarthroplasty is a viable salvage procedure with a reasonably good outcome in the surgically fit patient.
Ethics Approval Body
Monash University Human Research Ethics Committee.
Study Approval ID
Study approval ID is 27656.
Disclaimer
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Wed 02, Jun 2021Accepted: Wed 16, Jun 2021
Published: Tue 29, Jun 2021
Copyright
© 2023 Simon N Bell. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2021.01.02
Author Info
Simon N Bell Maxim U.S.I. Christmas Jennifer A. Coghlan
Corresponding Author
Simon N BellDepartment of Surgery, School of Clinical Sciences, Monash Health, Monash University, Clayton, Victoria, Australia
Figures & Tables

References
1.
Abdel
MP, Hattrup SJ, Sperling JW, Cofield RH, Kreofsky CR et al. (2013) Revision of
an unstable hemiarthroplasty or anatomical total shoulder replacement using a
reverse design prosthesis. Bone Joint J 95-B: 668-672. [Crossref]
2. Baulot E, Garron E, Grammont PM
(1999) [Grammont prosthesis in humeral head osteonecrosis.
Indications—results]. Acta Orthop Belg 65: 109-115. [Crossref]
3.
Baulot
E, Sirveaux F, Boileau P (2011) Grammont's idea: The story of Paul Grammont's
functional surgery concept and the development of the reverse principle. Clin
Orthop Relat Res 469: 2425-2431. [Crossref]
4.
De
Wilde LF, Plasschaert FS, Audenaert EA, Verdonk RC (2005) Functional recovery
after a reverse prosthesis for reconstruction of the proximal humerus in tumor
surgery. Clin Orthop Relat Res 156-162. [Crossref]
5.
Laudicina
L, D'Ambrosia R (2005) Management of irreparable rotator cuff tears and
glenohumeral arthritis. Orthopedics 28: 382-388. [Crossref]
6.
Rockwood
CA, Jr (2007) The reverse total shoulder prosthesis. The new kid on the block. J
Bone Joint Surg Am 89: 233-235. [Crossref]
7.
Wall
B, Walch G (2007) Reverse shoulder arthroplasty for the treatment of proximal
humeral fractures. Hand Clin 23: 425-430. [Crossref]
8. Boileau P, Watkinson DJ, Hatzidakis
AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and
biomechanics. J Shoulder Elbow Surg 14: 147S-161S. [Crossref]
9.
Zhou
HS, Chung JS, Yi PH, Li X, Price MD (2015) Management of complications after
reverse shoulder arthroplasty. Curr Rev Musculoskelet Med 8: 92-97. [Crossref]
10. Wall B, Nove Josserand L, O'Connor
DP, Edwards TB, Walch G (2007) Reverse total shoulder arthroplasty: a review of
results according to etiology. J Bone Joint Surg Am 89: 1476-1485. [Crossref]
11.
Zumstein
MA, Pinedo M, Old J, Boileau P (2011) Problems, complications, reoperations,
and revisions in reverse total shoulder arthroplasty: a systematic review. J
Shoulder Elbow Surg 20: 146-157. [Crossref]
12. Crosby LA, Hamilton A, Twiss T (2011)
Scapula fractures after reverse total shoulder arthroplasty: classification and
treatment. Clin Orthop Relat Res 469: 2544-2549. [Crossref]
13.
Molé
D, Favard L (2007) [Excentered scapulohumeral osteoarthritis]. Rev Chir
Orthop Reparatrice Appar Mot 93: 37-94. [Crossref]
14.
Levy
JC, Anderson C, Samson A (2013) Classification of postoperative acromial
fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am
95: e104. [Crossref]
15.
Rouleau
DM, Gaudelli C (2013) Successful treatment of fractures of the base of the
acromion after reverse shoulder arthroplasty: Case report and review of the
literature. Int J Shoulder Surg 7: 149-152. [Crossref]
16. Farshad M, Gerber C (2010) Reverse
total shoulder arthroplasty-from the most to the least common complication. Int
Orthop 34: 1075-1082. [Crossref]
17.
Walch
G, Mottier F, Wall B, Boileau P, Mole D et al. (2009) Acromial insufficiency in
reverse shoulder arthroplasties. J Shoulder Elbow Surg 18: 495-502. [Crossref]
18. Mottier F, Wall B, Nove Josserand L,
Galoisy Guibal L, Walch G (2007) [Reverse prosthesis and os acromiale or
acromion stress fracture]. Rev Chir Orthop Reparatrice Appar Mot 93:
133-141. [Crossref]
19. Otto RJ,
Virani NA, Levy JC, Nigro PT, Cuff DJ et al. (2013) Scapular
fractures after reverse shoulder arthroplasty: evaluation of risk factors and
the reliability of a proposed classification. J Shoulder Elbow Surg 22:
1514-1521. [Crossref]
20.
Mayne
IP, Bell SN, Wright W, Coghlan JA (2016) Acromial and scapular spine fractures
after reverse total shoulder arthroplasty. Shoulder Elbow 8: 90-100. [Crossref]
21.
Lädermann A, Edwards TB, Walch G
(2014) Arm lengthening after reverse shoulder arthroplasty: a review. Int
Orthopaed 38: 991-1000. [Crossref]
22.
Lädermann
A, Williams MD, Melis B, Hoffmeyer P, Walch G (2009) Objective evaluation of
lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg 18:
588-595. [Crossref]
23.
Hattrup
SJ (2010) The influence of postoperative acromial and scapular spine fractures
on the results of reverse shoulder arthroplasty. Orthopedics 33. [Crossref]
24. Lópiz Y, Rodríguez González A, García
Fernández C, Marco F (2015) Scapula insufficiency fractures after reverse total
shoulder arthroplasty in rotator cuff arthropathy: What is their functional
impact? Rev Esp Cir Ortop Traumatol 59: 318-325. [Crossref]
25.
Wahlquist
TC, Hunt AF, Braman JP (2011) Acromial base fractures after reverse total
shoulder arthroplasty: report of five cases. J Shoulder Elbow Surg 20:
1178-1183. [Crossref]
26. Hamid N, Connor PM, Fleischli JF, D'Alessandro DF (2011) Acromial fracture after reverse shoulder arthroplasty. Am J Orthop (Belle Mead NJ) 40: E125- E129. [Crossref]
27. Teusink MJ, Otto RJ, Cottrell BJ, Frankle MA (2014) What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J Shoulder Elbow Surg 23: 782-790. [Crossref]
