A Modified Reconstruction Technique of Chest Wall after Radical Resection of Chondrosarcoma Underlying the Breast
A B S T R A C T
Chest wall tumors are uncommon and include a variety of Cartilaginous, bony, and soft tissue lesions. The clinical presentation varies from asymptomatic to chest pain or ulcerating chest mass. Retro mammary chondrosarcoma of the chest wall can present as a painless breast mass and may be mistaken for a breast tumor. A careful clinical examination and relevant investigations are a cornerstone to plan an appropriate surgical procedure.
Keywords
Chondrosarcoma, breast, chest wall resection and reconstruction
Introduction
Chest wall tumors are classified into three categories: Primary, secondary and metastatic. They can also be classified as benign and malignant neoplasm, as shown in (Table 1). Primary chest wall tumors are uncommon and only represent 0.2 to 2% of all tumors [1]. The commonest neoplasm of the chest wall is chondrosarcoma and constitutes 20-30 % of primary chest wall tumors. It arises from the costochondral (80%) or costosternal (20%) junctions, respectively [2]. We report a case of retro mammary Chondrosarcoma, which presented as a breast mass. After careful critical examination and radiological diagnosis, radical resection and reconstruction of the chest wall were successfully performed.
Case Report
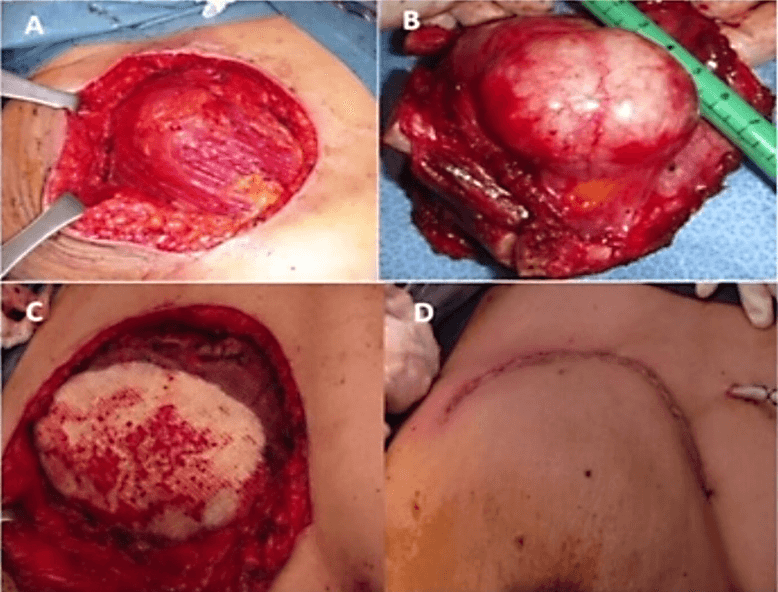
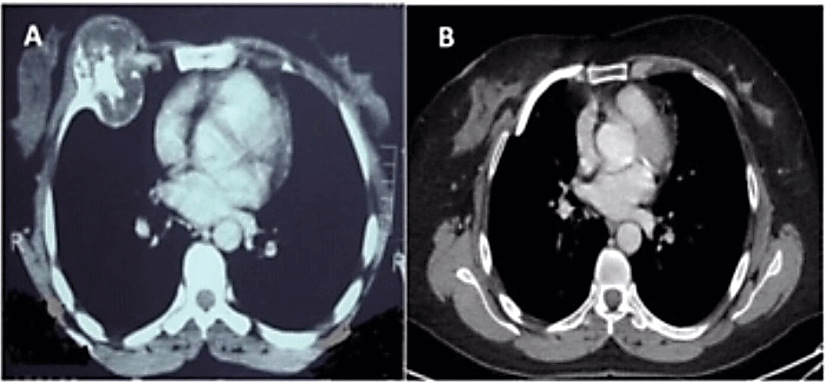
A 50-year-old female presented with a history of pain in right breast of two months duration. There was no history of cough or shortness of breath. On superficial palpation, the right breast was normal, but on deep palpation, there was a fixed palpable mass with freely mobile overlying breast tissue. There were no palpable regional lymph nodes. Hematology and biochemistry panels were normal, as was her mammogram. Chest x-ray revealed opacity, and Computed Tomography (CT) of the thorax showed a mass arising from the 4th costochondral junction in the retro mammary area. The radiological feature was consistent with the osteochondroma of the chest wall (Figure 1A). After informed consent, surgery was planned. The mass was approached by a crescent-shaped incision along the right breast crease. The breast was reflected from the bed to the lateral site along with part of the pectoralis major muscle and right side 3-6 ribs were divided latterly and reflected which revealed 4 cm x 5.5 mass, rib above and below was excised en-bloc with a 5 cm clear margin (Figures 2A & 2B).
The excised specimen was removed and sent for histopathology which was reported chondrosarcoma. The defect in the chest wall was measured and we reconstructed with methyl methacrylate (MMA) plate of appropriate size. Holes were drilled in surrounding bones and also correspondingly in MMA plate. MMA plate was placed in double layer of marlex mesh and plate was anchored to all bones with 2/0 prolene suture, then marlex mesh was sutured to the surrounding tissues. The right breast was sutured back to its anatomical position, and subcuticular stiches were applied to skin (Figures 1C & 1D). the patient was extubated on the table. Her post-operative recovery was uneventful. Ten-year post-surgery CT scan showed no recurrence (Figure 1B).
Figure 1: A) Circular incision around the breast. B) Tumor excised specimen en-bloc with the adjacent part of the ribs. C) Chest wall defect reconstructed with modified (MMS) Cement & Marlex mesh sandwich technique. D) Skin closure preserving the breast contours.
Figure 2: A) Pre-operative CT scan of the thorax showing retro mammary chondrosarcoma of the ribs. B) CT scan of the Thorax 10 years post-operative follow-up, showing the MMS plate in place.
Table 1: Classification of chest wall tumors.
|
Type |
Soft Tissue |
Bone and Cartilage |
|
Malignant |
Soft tissue sarcoma |
Chondrosarcoma |
|
|
Desmoid tumor |
Osteosarcoma |
|
|
Squamous cell carcinoma |
Ewing's sarcoma |
|
|
Basal cell carcinoma |
Plasmacytoma |
|
|
Melanoma |
|
|
|
Neuroectodermal tumors |
|
|
|
|
|
|
Benign |
Fibroma |
Chondroma |
|
|
Lipoma |
Fibrous dysplasia |
|
|
Rhabdomyoma |
Osteochondroma |
|
|
Neurofibroma |
Osteoblastoma |
|
|
Haemangioma |
Giant cell tumor |
|
|
Lymphangioma |
Aneurysmal bone cyst |
Discussion
The common benign primary neoplasm of the chest is, fibrous dysplasia, chondral, and osteochondroma. Fibrous dysplasia comprises 30% of benign chest wall tumors. Chondromas are slow-growing tumors and are common in the 2nd and 3rd decades of life. They are asymptomatic and should be distinguished from chondrosarcoma [2]. Osteochondromas that arise from the bony cortex of the rib are uncommon. Complete resection of these tumors should be performed because they can transform into Chondrosarcoma. Malignant primary chest wall tumors are Bony sarcomas [3]. Ewing sarcoma, cartilaginous tumors (Chondrosarcoma), and soft tissue sarcoma. Sometimes multiple myeloma presents with local bony lesions (solitary plasmacytoma).
Incomplete resection, metastasis, and age above 50 are poor prognostic factors. The main goal of surgery is complete en-bloc resection to prevent local recurrence and overall prolong survival [4]. Pre-operative evaluation of the patient is very important, including a complete history, physical examination, and appropriate imaging. Patients with malignant chest wall lesions commonly present with chest pain which is due to periosteal invasion and is a poor prognostic sign. Soft tissue sarcomas have a better prognosis, and they mostly present as a painless mass. The 5-year survival in these cases is 60%, the five-year. Survival of Erving sarcoma, Osteosarcoma, and plasmacytoma is 47%, 15% and 20%, respectively [5, 6]. In patients with chondrosarcoma of the anterior chest wall, the reported 5-year survival after complete resection is 70%. The outcome is poor in patients who have incomplete resection or who developed metastasis (approximately 20% of cases).
Pre-operative pulmonary function tests should be performed in major chest wall resection to evaluate the patient respiratory physiology and post-operative recovery because surgery alters the chest wall dynamics and respiratory physiology [7, 8]. The mayo clinic has reported a 5-year survival of 96% incomplete resection in chondrosarcoma and 70% for those who have incomplete resection [9, 10]. There is still considerable controversy about save resection margins. Mayo clinic reported that with a 4 cm or greater tumor resection margin, recurrence at 5 years is only 29% as compared to those who have a 2 cm margin. However, Memorial-Sloan-Kettering experience shows a 2-5 cm margin, and a rib above and below is adequate, but a lateral margin of 4-5cm on the rib is advised because most malignant tumors tend to spread along the bone [11, 12]. The aim of chest wall reconstruction during surgery is threefold, providing chest wall stability, soft tissue coverage, good cosmoses and maintenance of pulmonary functions. Skeletal reconstruction can be achieved with synthetic materials such as silicone elastomers, acrylics, marlex, prolene meshes, and Gortex patch (polytetrafluoroethylene) [13-15]. Chest wall defected less than 5 cm and located at the apex and in the scapular area usually don’t require reconstruction [5, 16].
We preferred a methyl methacrylate (bone cement) sandwiched between the marlex mesh because of its lightweight and adherence to the bones, which allows tissue ingrowth. Another advantage is its radiolucency which is very helpful to evaluate the lung field in the follow-up radiological investigations [17]. Soft tissue coverage can be provided by myocutaneous flaps, including pectoralis major, Lattismus dorsii, rectus abdominus, serratus anterior, and trapezius muscle. The Lattisimus dorsii flap was first used in 1950 by Campbell [18]. Omental flaps can be useful for poorly healing infected and radiated wounds, as described by Kirticuta [19]. The reported post-operative mortality for chest wall resection and reconstruction is 3.8-4.5%. Post-operative complications are mostly pulmonary, including chest wall instability, respiratory insufficiency, hemothorax, and infection, and post-operative atelectasis [20, 21]. Cardiac arrhythmias and thromboembolism have also been reported. Almost 10-15% of post-operative patients develop respiratory insufficiency. Infection of reconstruction material and subsequent infection of myocutaneous flap is a real challenge to deal with. When resection is incomplete or substandard, recurrence rate is high.
Conclusion
In conclusion, the tumor of chest wall resection and reconstruction is a real surgical challenge that needs a multi-disciplinary approach, including the thoracic surgeon, oncologist, pulmonologist, plastic surgeon, intensivist, and Physiotherapist. In conclusion our Modified reconstruction technique has several advantages, it provides excellent chest wall stability, and there is no chance of MMS plate displacement or excursion. Breast anatomical geometry is preserved with excellent cosmoses. Radical excision with 5cm tumor free margins is essentially a major factor for overall long-term survival. Ten years follow-up CT-Scan of the thorax in our patient showed no recurrence, and the patient is enjoying everyday life.
Article Info
Article Type
Case ReportPublication history
Received: Mon 24, May 2021Accepted: Tue 08, Jun 2021
Published: Wed 30, Jun 2021
Copyright
© 2023 Chaudhry Aqeel. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2021.01.01
Author Info
Chaudhry Aqeel Ahsan Cheema Fahad G. Alradei Thabet Alghazal Ahmed Al Shaer Yousif A Al Qahtani Burair Al Jassas Benish Razaq Ikram ul Haq Chaudhry
Corresponding Author
Chaudhry AqeelDepartment of Thoracic Surgery, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Figures & Tables
Table 1: Classification of chest wall tumors.
|
Type |
Soft Tissue |
Bone and Cartilage |
|
Malignant |
Soft tissue sarcoma |
Chondrosarcoma |
|
|
Desmoid tumor |
Osteosarcoma |
|
|
Squamous cell carcinoma |
Ewing's sarcoma |
|
|
Basal cell carcinoma |
Plasmacytoma |
|
|
Melanoma |
|
|
|
Neuroectodermal tumors |
|
|
|
|
|
|
Benign |
Fibroma |
Chondroma |
|
|
Lipoma |
Fibrous dysplasia |
|
|
Rhabdomyoma |
Osteochondroma |
|
|
Neurofibroma |
Osteoblastoma |
|
|
Haemangioma |
Giant cell tumor |
|
|
Lymphangioma |
Aneurysmal bone cyst |
References
1.
Anderson BO, Burt
ME (1994) Chest wall neoplasms and their management. Ann Thoracic Surg
58: 1774-1781. [Crossref]
2.
Martini N,
McCormack P, McCaughan BE (1985) Tumors of the chest wall. International
practice in cardiothoracic surgery. Science Press 1985: 27990.
3.
Robbins SL,
Cotran RS (1979) Chondromatous tumors. In: Pathologic basis of disease, 2nd ed.
Saunders 1505.
4.
Burt M (1994)
Primary malignant tumors of the chest wall. The Memorial Sloan-Kettering Cancer
Center experience. Chest Surg Clin N Am 4: 137-154. [Crossref]
5.
Albright F,
Butler AM, Hampton AO, Smith P (1937) Syndrome Characterized by Osteitis
Fibrosa Disseminata, Areas of Pigmentation and Endocrine Dysfunction, with
Precocious Puberty in Females-Report of Five Cases. N Engl J Med 216:
727-746.
6.
Robbins SL,
Cotran RS (1979) Multiple osteocartilaginous exostoses. Pathologic basis of
disease, 2nd ed. Saunders 1979: 1482-1483.
7.
Pairolero PC,
Arnold PG (1985) Chest wall tumors. Experience with 100 consecutive patients.
J Thorac Cardiovasc Surg 90: 367-372. [Crossref]
8.
Larson DL,
McMurtrey MJ (1984) Musculocutaneous flap reconstruction of chest-wall defects:
an experience with 50 patients. Plast Reconstr Surg 73: 734-740. [Crossref]
9.
Boyd A (1986)
Chest wall resection. Surgical diseases of the pleura and chest wall. Saunders
1986: 251-261.
10.
11.
McCormack PM,
Bains MS, Burt ME, Martini N, Chaglassian T et al. (1989) Local recurrent
mammary carcinoma failing multimodality therapy. A solution. Arch Surg
124: 158-161. [Crossref]
12.
King RM,
Pairolero PC, Trastek VF, Piehler JM, Payne WS et al. (1986) Primary chest wall
tumors: factors affecting survival. Ann Thorac Surg 41: 597-601. [Crossref]
13.
Abbes M, Mateu J,
Giordano P, Bourgeon Y (1991) Chest wall reconstruction after full thickness
resection: an experience with 22 patients. Eur J Surg Oncol 17: 342-349.
[Crossref]
14.
Arnold PG,
Pairolero PC (1984) Chest wall reconstruction. Experience with 100 consecutive
patients. Ann Surg 199: 725-732. [Crossref]
15.
Cotton BH,
Paulsen GA, Dykes J (1956) Prosthesis following excision of chest wall tumors. J
Thorac Surg 31: 45-59. [Crossref]
16.
Robbins SL,
Cotran RS (1979) Chondromatous tumors. Pathologic basis of disease, 2nd ed.
Philadelphia: Saunders 1979: 1505.
17.
McCormack P,
Bains MS, Beattie EJ, Martini N (1981) New trends in skeletal reconstruction
after resection of chest wall tumors. Ann Thorac Surg 31: 45-52. [Crossref]
18.
Campbell DA
(1950) Reconstruction of the anterior thoracic wall. J Thorac Surg 19:
456-561. [Crossref]
19.
Jacobs EW,
Hoffman S, Kirschner P, Danese C (1978) Reconstruction of a large chest wall
defect using greater omentum. Arch Surg 113: 886-887. [Crossref]
20. McCaughan BC, Martini N, Bains MS, McCormack PM (1985) Chest wall invasion in carcinoma of the lung. Therapeutic and prognostic implications. J Thorac Cardiovasc Surg 89: 836-841. [Crossref]
21. Allen MS, Mathisen DJ, Grillo HC, Wain JC, Moncure AC et al. (1991) Bronchogenic carcinoma with chest wall invasion. Ann Thorac Surg 51: 948-951. [Crossref]
