A Novel Approach to Managing Giant Duodenal Ulcer Perforations: Minimizing Ostomies, Maximizing Decompression. A Case Report
A B S T R A C T
Background: Peptic ulcer perforation is a deadly complication of duodenal ulcers. The literature is still sparse in terms of giant duodenal perforations. There exist a variety of techniques to decompress the duodenum after repair which leave the patient with multiple ostomies that require extensive postoperative care.
Case presentation: In this case we present a patient with AIDS who was found to have a large duodenal ulcer perforation. Intraoperatively the fragility of the patient’s duodenum warranted a method of decompression that would keep the integrity of the duodenal tissue. The common method of lateral duodenostomy was not the best option and instead a gastro-jejunal feeding tube was altered into a gastro-duodenal tube to avoid creating another ostomy. Postoperatively she did not show signs of leak, but eventually died from sepsis secondary to fulminant AIDS.
Conclusions: We propose this technique as a novel method of decompressing the duodenum. This new method eliminates the need for excessive ostomies and has the possibility to make the postoperative transition simpler.
Keywords
Duodenal perforation, duodenal ulcer, duodenal compression, peptic ulcer, ostomy, GJ tube
Background
Peptic ulcer perforation occurs in 2-10% of ulcers and can become a life-threatening disease, with a mortality of 10-40% [1]. Literature largely refers to “large” ulcers as those between 1 and 2 cm and “giant” as those that exceed 2-3cm, although there is no well-defined classification, nor a described incidence of large vs. small. In a 2005 study by Gupta et al, giant duodenal ulcers were found to have significantly higher leak rates than ulcers less than 1cm (13% and 2.5% respectively). Patients with large ulcers stayed in the hospital twice as long and had a mortality of 15.79% compared to patients with small ulcer patients who had a mortality of 5.74% [2]. These ulcers clearly pose a greater surgical dilemma in terms of the optimal surgical approach to minimize leak rate. Frequently a large perforation is surrounded by inflamed tissues and can be too friable to allow for a safe primary suture.
Traditionally, duodenal perforations are repaired with an omental patch or Graham patch [3-5]. However, in cases of large and giant ulcers, other surgical techniques such as a jejunal serosal patch, jejunal pedicled graft, free omental plug, suturing the omentum to the nasogastric tube, and pyloric exclusion with gastrojejunostomy, may be deemed necessary to ensure adequate closure [6]. In the past, 10% of perforated peptic ulcers underwent gastrectomy for repair. However, a 2017 study by Seow et al. indicated that gastrectomy should be avoided as there was no benefit in morbidity or mortality [7].
Decompression of the repaired duodenum is an important step to help minimize leaks. Consideration of enteral feeding access is a reasonable option in anticipation of complications and leaks. Decompression of the duodenum can also be achieved by lateral duodenostomy or retrograde duodenostomy. A lateral duodenostomy allows for internal drainage, decreasing quantity of leak, and is favored in the surgical setting where a specialist is not available to perform the repair [8]. However, this drainage technique is not feasible when the duodenal tissue is friable or if there is extensive fibrosis of the duodenum limiting its mobilization as seen in Agarwal’s 2017 study [9]. Another option is the Triple-Tube-Ostomy technique in which a tube gastrostomy, a retrograde tube duodenostomy, and a feeding jejunostomy are created to protect the fragile duodenal repair from pancreaticobiliary and gastric secretions, while providing enteral nutrition [10, 11]. This technique has shown promising results for reducing hospital stay and mortality. However, the technique was also noted to have a surgical site infection rate of 45%.
Furthermore, each tube ostomy is a source of complications including infection, leakage, and internal herniation. Therefore, developing techniques which allow for maximal decompression of the duodenum and stomach with a minimal number of tube ostomies is advantageous. In this paper, a new technique for duodenal decompression for a large/giant duodenal ulcer is described in which a single GJ feeding tube was modified to allow for decompression of the stomach and duodenal repair, thus allowing for the avoidance of a lateral or retrograde duodenostomy.
Case Presentation
This technique was used during surgery at a level 1 trauma center on a 50-year-old female with two large anterior duodenal perforations.
I The Patient
This patient had several comorbidities including AIDS with a CD4 count of 44, COPD with chronic steroid dependence, and lung cancer status post resection. She had undergone an exploratory laparotomy for small bowel obstruction due to immune reconstitution inflammatory syndrome. The patient’s postoperative course was initially uncomplicated with return of bowel function and tolerance of diet by POD #3. On postoperative day 10 the patient required intubation and vasopressors and was found to have enteric contents draining from her midline wound. Viscus perforation was suspected, and she was brought to the operating room. In the operating room, a large post-pyloric duodenal ulcer (1.5cm) was found on the anterior wall and a second giant (2.5cm) perforated duodenal ulcer was found along the antimesenteric border of the duodenum at D1 with extension to D2. The base of the ulcer extended to the posterior wall at the level of the ampulla of Vater. The two ulcers were separated by ischemic serosa (approximately 0.3cm). This ischemic bridge was resected. The duodenal defect compromised 2/3 of the circumference of the duodenum.
To repair the ulcer, we primarily repaired the defect using a running Connell stitch which was then reinforced with falciform ligament and a well vascularized tongue of omentum. A bubble leak test was performed, with insufflation of the stomach and duodenum submerged in a saline filled surgical field; no leak was noted.
II The Technique
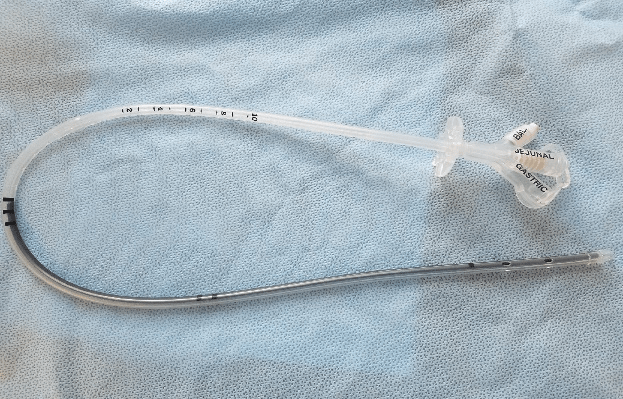
We used a GJ tube from Halyard™ (Figure 1), modifying it into a GD tube to aid in internal decompression of duodenum. A GJ 22F tube was trimmed and additional openings were created along the jejunal channel of the drain (Figure 2). Figure 3 (copyright Halyard™) depicts the decompression technique with annotations showing our modifications. A purse string stitch was placed around the gastrotomy site, and after passing the tube through the abdominal and gastric wall, the stomach was tacked to abdominal wall. This tube was therefore used to drain the proximal jejunum, the duodenum, and the stomach. The jejunal and gastric openings were placed on suction to gravity and low suction, respectively. We then thoroughly irrigated the abdomen and performed a Witzel jejunostomy using a 20-French red rubber catheter. We placed two 18-French Blakes, one in the posterolateral portion of our mobilized duodenum and one overlying the Graham patch repair in order to drain the repair site.
Results
The patient was then transferred back to the critical care unit on vasopressors. POD 2-3 the duodenal repair did not demonstrate any signs of leak, with minimal drain output. Following the surgery, the patient remained septic, and expired on postoperative day five due to overwhelming AIDS/pulmonary sepsis with signs of pneumonia on chest x-ray and increasing ventilatory and pressor requirements.
Figure 1: Original GJ tube from Halyard™. Image courtesy of V.Roudnitsky
Figure 2: Modified GJ Tube from Halyard. Arrows show newly created holes in tubing. Dashed line shows cut at the end of the tube. Image courtesy of D.J.Gross.
Figure 3: GJ Tube in place. Original drawing from Halyard ™ with our modifications. Solid arrows are where original gastric openings are. Dotted arrows show where the new openings were created. Solid lines show where the end of the tube was transected.
Conclusion
Duodenal perforation continues to be a significant and deadly complication of peptic ulcer disease; especially in the setting of severe comorbidities [12]. Leakage at the site of repair remains a common complication. The postoperative care of these patients is important to prevent peritonitis. In this paper we have described a novel method of decompressing the duodenum following large duodenal repair to prevent the need for lateral duodenostomy. The benefit of this new technique lies in its simplification of postsurgical drainage and reduction of postoperative complications. In contrast to the triple tube ostomy, a third tube does not have to be managed in this technique. The elimination of one of the ostomies and tubes could decrease postoperative infection rates. The gastrojejunostomy tube can eventually be exchanged for a simple gastrostomy tube, which can then be removed at the bedside to close without intervention. The jejunostomy tube can be removed once enteral feeds are no longer necessary. By eliminating the need for lateral duodenostomy, postoperative management and transition to rehab care will be easier.
Ethics approval and consent to participate
No identifying human information was used.
Consent for Publication
Not applicable.
Availability of data and materials
Not applicable.
Competing Interests
None.
Funding
No funding was provided.
Authors’ contributions
D.G developed the method and edited the article. A.L drafted the initial article, collected images and incorporated co-author revisions. A.E. assisted in manuscript creation and revision. V.R. assisted in editing and vision.
Acknowledgements
None.
List of abbreviations
GJ: gastro-jejunal
GD: gastro-duodenal
POD: post-operative day
COPD: chronic obstructive pulmonary disease
AIDS: acquired immunodeficiency syndrome
Article Info
Article Type
Case ReportPublication history
Received: Sun 06, Oct 2019Accepted: Thu 24, Oct 2019
Published: Tue 05, Nov 2019
Copyright
© 2023 Daniel Gross. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.05.114
Author Info
Daniel Gross Egelko Aron Levi Amelia Roudnitsky Valery
Corresponding Author
Daniel GrossSUNY Downstate Health Sciences University, 450 Clarkson Ave, Brooklyn, NY 11203
Figures & Tables


References
- Chung K, Shelat V (2017) Perforated peptic ulcer - an update. World J Gastrointest Surg 9: 1-12. [Crossref]
- Gupta S, Kaushik R, Sharma R, Attri A (2005) The Management of large perforations of duodenal ulcers. BMC Surg. 2005 5:15. [Crossref]
- Bertleff MJ, Lange JF (2010) Perforated Peptic Ulcer Disease: A Review of History and Treatment. Dig Surg 27: 161-169. [Crossref]
- Cellan-Jones CJ (1929) A Rapid Method of Treatment in Perforated Duodenal ulcer. Br Med J 1: 1076-1077. [Crossref]
- Graham R (1937) The Treatment of Perforated Duodenal Ulcers. Surgery Gynecology Obstetric 64: 235-238.
- Fraga GP Biazotto G, Bortoto JB, Andreollo NA, Mantovani M (2008) The Use of Pyloric Exclusion for Treating Duodenal Trauma: Case Series. Sao Paulo Med J 126: 337-341. [Crossref]
- Seow JG, Lim YR, Shelat VG (2017) Low serum albumin may predict the need for gastric resection in patients with perforated peptic ulcer. Eur J Trauma Emerg Surg 43: 293-298. [Crossref]
- Kutlu OC, Garcia S, Dissanaike S (2013) The successful use of simple tube duodenostomy in large duodenal perforations from varied etiologies. Int J Surg Case Rep 4: 279-282. [Crossref]
- Agarwal N, Malviya NK, Gupta N, Singh I, Gupta S (2017) Triple Tube drainage for difficult gastroduodenal perforations: A prospective study. World J Gastrointest Surg 9: 19-24. [Crossref]
- Fujikuni N, Tanabe K, Yamamoto H, Suzuki T, Tokumoto N et al. (2011) Triple-Tube-Ostomy: A Novel Technique for the Surgical Treatment of Iatrogenic Duodenal Perforation. Case Rep Gastroenterol 5: 672-679. [Crossref]
- Brown CVR, Inaba K, Martin MJ, Salim A (2019) Emergency General Surgery: A Practical Approach - 1st Ed. Springer International Publishing.
- Gross DJ, Chung PJ, Smith MC, Roudnitsky V, Alfonso AE et al. (2018) End Stage Renal Disease Is Associated with Increased Mortality in Perforated Gastroduodenal Ulcers. Am Surg 84: 1466-1469. [Crossref]
