A Rare Case Report of Infected Baker’s (Popliteal) Cyst
A B S T R A C T
A popliteal cyst, otherwise known as a Baker’s cyst, is a fluid-filled sac that forms behind the knee between the medial head of the gastrocnemius and the semimembranosus muscles. These cysts have a high prevalence in the adult population and are frequently associated with a variety of degenerative conditions of the knee, which complicates the diagnosis. Our patient is an elderly male initially evaluated for a deep venous thrombosis. Further evaluation revealed a baker’s cyst abscess, which was diagnosed on imaging and confirmed post-operatively. A culture growth of the abscess was obtained that grew Streptococcus anginosus. The patient presented with right leg swelling, erythema and knee pain. His physical exam showed significant effusion of the right knee, with tenderness to palpation of the right posterior knee and a limited range of motion with flexion. The venous duplex was negative for deep venous thrombosis (DVT) and the patient continued to experience significant pain with ambulation. A knee aspiration was done with purulent joint fluid sent for culture. A computed tomography (CT) scan without contrast of his right leg revealed a Baker’s cyst abscess within a collection of fluid. The patient was taken to the operating room (OR) with a diagnosis of right septic knee and popliteal cyst abscess where arthroscopic irrigation and debridement with extensive synovectomy of the right knee was performed. Aspiration cultures were positive for Streptococcus anginosus, which has a unique ability to promote abscesses formation. Patient tolerated the procedure well and was discharged from the hospital in good condition with instructions to take Rocephin IV for six weeks. The patient ambulated without difficulty and showed significant improvement after 2 months.
Keywords
Infected popliteal cyst, baker cyst abscess, septic arthritis, knee pain
Introduction
A Baker’s (popliteal) cyst is a distention of the gastrocnemius-semimembranosus bursa of the knee, which communicates with the posterior portion of the joint capsule [1]. Significant complications rarely occur but the most common is cyst rupture or infection which can be confused clinically with deep venous thrombosis, and acute thrombophlebitis, which poses a diagnostic and management dilemma [1]. The purpose of this case report is to highlight an uncommon case of an infected popliteal cyst extending into the calf, associated with septic knee with significant challenges sorting out the differential diagnoses that come with such a presentation. The case described in this report additionally demonstrates that with appropriate diagnostic studies, and prompt treatment, better patient outcomes are achieved when treating Baker cyst abscesses.
Case Presentation
An 81-year-old Caucasian male with a history of atrial fibrillation, mitral valve prolapses, and previously on Xarelto, presented to the Emergency Department (ED) with right leg swelling and mild-to-moderate pain. The patient stated that he was doing yard work around five days prior to presenting to the ED. He did not recollect any trauma but later in the day noticed constant pain inside and back of the knee. The pain gradually escalated, and he tried ice packs with minimal relief. On the day of presentation, he developed right lower leg swelling with erythema and acute worsening of right knee pain to 9 out of 10 and exacerbated with ambulation. He presented to the urgent care for initial treatment but was ultimately sent to the ED. The patient denied any fever, chills, nausea, vomiting, neurological symptoms, or any personal or family history of blood clots. His only significant history was hyperlipidemia, for which he was taking a statin and chronic atrial fibrillation, for which he was transitioned from Xarelto to aspirin 162 mg by his cardiologist, following extensive workup the week prior to his ED presentation. He was an otherwise active male who exercised 5 days a week.
Surgical history was only notable for the removal of several lipomas of his lower extremities 2 years previously. His physical exam was noteworthy for +3 effusion to the right knee and slightly tender to palpation of the right posterior knee. The range of motion was limited at the right knee due to pain, notably with flexion. His right leg was warm and swollen (>3 cm larger than left calf) and mildly firmer compared to his left leg. Distal pulses were palpable and brisk. Homan’s sign was negative. Skin showed keratosis and both toenails were deformed with onychomycosis. In the Emergency Department, he was found to be in atrial fibrillation with rapid ventricular rate, but vitals were otherwise stable. His complete blood count (CBC) was within normal limits. The patient was given 1 dose of Rocephin for possible non-purulent cellulitis. He was also started on heparin and diltiazem drip and admitted to the hospital. His Wells score was 3. The differential diagnosis for his right leg symptoms included acute DVT versus possible cellulitis versus severe meniscal injury.
The next morning, the venous duplex was negative for DVT but did show a moderate size cyst in the medial aspect of the right calf area. Antibiotics were discontinued as the patient remained afebrile with no leukocytosis. However, he was reporting worsening of his pain and swelling. There was a concern for impending compartment syndrome, so orthopedic surgery was consulted. His right knee was aspirated by orthopedics for concern of septic arthritis versus gout flare. Thirty cc’s of very cloudy purulent yellow joint fluid was aspirated from the right knee. Cytology of the fluid showed 4+ (PMNs), 100,000+ white blood cells with no crystals. Acid Fast Bacilli smear and fungal culture were negative, and cultures were pending.
A CT scan without contrast of the right lower extremity was performed showing a fluid collection at the posterior medial aspect of the knee likely representing a Baker’s cyst which extended down to the posterior mid-calf measuring 15.2 cm in length by 4.0 cm in AP and 8.0 cm in the transverse plane with small air bubbles. There was also a right knee effusion with a small amount of air. The findings were concerning for an infected fluid collection consistent with an abscess. It was located between the medial head of gastrocnemius and soleus muscles. There was subcutaneous edema extending from the mid-thigh to the ankle, likely related to cellulitis. Degenerative changes of the knee were noted. The patient was started on Cefazolin 2 gm IV q8 hours and Flagyl 500mg IV q8 hr. Right lower leg swelling remained unchanged.
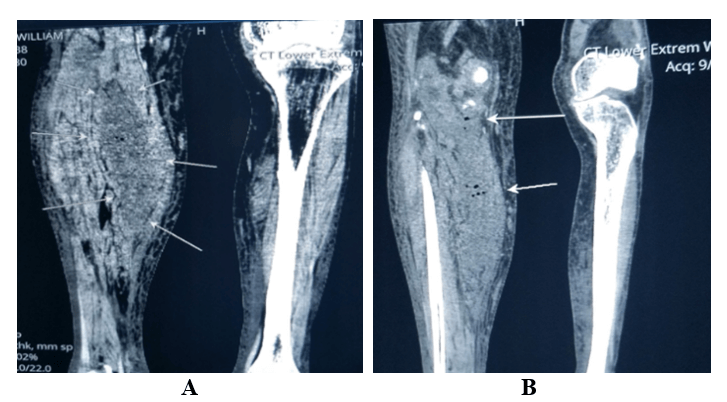
Figures 1: A) Above, Axial CT Lower Extremity. Right leg infected baker’s cyst. Note air bubbles in the cyst (white arrows); B) Above, Axial CT Lower Extremity. Right leg infected baker’s cyst. Note air bubbles in the cyst (white arrows).
Figures 2: A) Coronal image. CT Lower Extremity. Right leg infected baker’s cyst. Note air bubbles in the cyst (white arrows); B) Coronal image. CT Lower Extremity. Right leg infected baker’s cyst. Note air bubbles in the cyst (white arrows).
The next day, vancomycin was added for possible methicillin-resistant Staphylococcus aureus (MRSA) coverage. Additional blood work was ordered showing C-reactive protein (CRP) of 17.25 mg/dl (normal <4.99). ASO titers were ordered to check for post-streptococcal arthritis which were normal. A teichoic acid antibody was ordered to assess for Staphylococcus aureus, which later came back negative. The patient continued experiencing significant pain with ambulation and was subsequently taken to the operating room for his right septic knee and infected baker's cyst with extension into his lower leg. Arthroscopic irrigation and debridement with extensive synovectomy and partial lateral meniscectomy for lateral meniscus tear were performed which was discovered during the surgery of the right knee. The calf was milked to express the Baker's cyst into the joint and a large amount of purulent fluid was excavated and suctioned. Three liters of vancomycin and saline were run through the knee before closure. The patient was stable post-procedure. Additionally, aspiration cultures showed pan sensitive Streptococcus anginosus growth. The patient was discharged with Rocephin 2g daily for six weeks and aspirin 325 mg for atrial fibrillation. He was stable upon discharge with significant improvement of his symptoms.
Discussion
Baker’s cyst has a high prevalence in the adult population [1]. However, Baker’s cyst abscess, rupture and calf dissemination are uncommon, with only a small number of cases being reported in the medical literature [1]. The prevalence of these cysts increases with age, most commonly occurring in patients between ages 35 and 70 [2]. One-third of patients present with a history of trauma, or a history of coexisting joint diseases such as rheumatoid arthritis, osteoarthritis, and meniscal tears, seen in about two-thirds of patients [3].An accurate diagnosis to distinguish between a possible deep venous thrombosis versus a complicated infected Baker’s cyst is paramount as delays can result in a surgical emergency. In such a situation, the surgeon must be aware of the knee involvement and additional possible complications. Literature also showed that about 2% and 6% of deep venous thrombosis (DVTs) are actually, pseudo-thrombophlebitis as a result of a Baker’s cyst rupture. Hence, this can be worsened by the administration of heparin or anticoagulants for DVT treatment. Thus, an accurate diagnosis is of paramount importance for appropriate treatment [4].
The patient in our case report had the risk factors of having a popliteal cyst, knee pathology, as well as DVT. Risk factors for the popliteal cyst were age, having degenerative joint disease, and a recent meniscal injury to the knee. The patient was recently switched off Xarelto for atrial fibrillation to aspirin by his cardiologist. He initially presented to the ED with vague symptoms of leg swelling and pain without any fever or abnormal white blood cells. DVT was eventually ruled out with an ultrasound of the lower extremity. Subsequently, he had increased pain and the patient noted worsening of swelling while hospitalized. Given the worsening of symptoms and the possibility of an associated septic knee, a CT scan was performed, and an orthopedic surgeon was consulted promptly. He was subsequently started on broad-spectrum antibiotics and was taken for surgery within 24 hours.
The patient had arthroscopic irrigation and debridement done with extensive synovectomy of the knee and partial meniscectomy. The aspiration cultures were positive for pan sensitive Streptococcus anginosus and patient was discharged with Rocephin for 6 weeks. For an accurate diagnosis, an MRI is the gold-standard imaging study to confirm the presence and complications of a Baker’s cyst [1]. If not available, an ultrasound can help with the diagnosis and fluid sampling [1]. Computerized axial tomography and MRI can also outline the cyst more accurately and allows assessment for rupture of the cyst, hemorrhagic transformation, and accompanying pyomyositis or osteomyelitis [1].
In our case, treatment included arthroscopic surgical irrigation of the knee and open debridement of the calf was performed. The literature is inconclusive regarding whether the cyst resection should be performed. Cystectomy is usually avoided, except when primary cysts are extremely symptomatic [5]. One study recommended treatment of the primary disease, e.g., meniscal tear with partial meniscectomy, which in our case also included partial meniscectomy to avoid cyst recurrence. The cyst disappears once the primary disease is treated [5]. In another case report from the Cleveland clinic, Drees et al. reported a case of an injection drug user with multiple soft-tissue abscesses, severe swelling and pain in the right lower leg [6].
An MRI confirmed the presence of a Baker’s cyst with increased signal on T1 & T2 weighted images indicating a hemorrhagic or possibly infected cyst. Changes in the adjacent bones were suggestive of osteomyelitis. The incision and drainage of the cyst were performed, and cyst fluid culture yielded penicillin-susceptible Staphylococcus aureus. The most commonly noted causative pathogens per literature review are Staphylococcus aureus, Mycobacterium tuberculosis, Aspergillus fumigatus, Escherichia coli, and Bacteroides Fragilis [6]. Interestingly, in our case, the culture of the aspirate grew Streptococcus anginosus which is not commonly reported in the literature. In terms of antibiotic choices, if gram stain and bacterial culture of the aspirate are negative, specimens should be sent for acid-fast and fungal staining and culture [7, 8]. Fluid analysis and identification of the infectious agent are necessary to initiate tailored antibiotic treatment [9].
Of note, cases of Baker’s cyst caused by the Streptococcus anginosus group, are not seen commonly in the medical literature. It is a subgroup of Viridans streptococci that consists of three distinct streptococcal species: S. anginosus, S. intermedius, and S. constellatus. The organisms are a constituent of normal human flora (oral cavity, throat, stool, and vagina) with the unique ability to cause abscesses and systemic infections [10, 11]. The precise virulence factors responsible for the formation of the abscess are not fully understood; polysaccharide capsules, pyrogenic exotoxins, and hydrolytic enzymes are thought to play important roles. Interaction between the S. anginosus group and polymorphonuclear granulocytes may play a role in abscess formation [12].
Moreover, these organisms can enter the circulation even in the absence of a clinically obvious site of trauma or infection as in our case [10, 11]. Treatment requires a lengthy course of antibiotic therapy, along with adequate drainage or surgery. Ceftriaxone is the preferred antimicrobial agent due to excellent activity and tissue penetration with once-daily dosing. Our patient received six weeks of Rocephin and responded well to the treatment. If allergy or resistance precludes the use of beta-lactam agents, vancomycin is an appropriate alternative agent (MICs 0.0125 to 1.0 mcg/mL). This case is a lesson highlighting the importance of investigating vague symptoms in the inpatient setting if a patient has the risk factors for a popliteal cyst infection. An accurate diagnosis of a complication of Baker’s cyst is paramount as delays can result in a surgical emergency and worse patient outcomes.
Patient Perspective
“On a Friday, while cutting my grass, I injured my knee without my knowledge. This turned out to be some damage to my right meniscus. I made arrangements to see a surgeon early the following week. Next week, on Monday, after showering I noticed tremendous swelling in my right leg along with the knee and leg pain. I immediately visited an urgent care facility. The doctor there was worried about a blood clot and suggested I immediately go to the hospital. I would say the pain was average and made it difficult to drive. Not sure how much of these symptoms was the meniscal injury and how much was caused from the baker’s cyst.
However, throughout this time, my main concern also was the possibility of a clot in the leg. I was admitted to the hospital for almost a week. It took 2-3 days to eliminate the clot concern. After a bit more time and some more imaging, it was determined that it was an infected Baker’s Cyst. I was taken for surgery, where they fixed my meniscus and flushed out my knee. After a couple of days, I was released to go home on IV antibiotics. After my hospital discharge, I followed with my family doctor. My family doctor arranged for an infusion company to treat me with antibiotics. I did this every day for six weeks. However, I am very thankful for the antibiotics to eliminate the infection and improve my pain. I am doing very well now. A week ago, I finished therapy sessions on my knee. I feel like I am back to normal.”
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 17, Apr 2020Accepted: Fri 01, May 2020
Published: Fri 08, May 2020
Copyright
© 2023 Salieha Zaheer. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.05.02
Author Info
Elizabeth Towner Hassan Baiz Pierre Morris Rehana Siddique Salieha Zaheer
Corresponding Author
Salieha ZaheerAscension Providence Rochester Hospital, Michigan, USA
Figures & Tables

References
- Verbner JM, Pereira Duarte M, Zicaro JP, Yacuzzi C, Costa Paz M (2018) Infected Baker’s Cyst: A New Classification, Diagnosis and Treatment Recommendations. J Orthop Case Rep 8: 16-23. [Crossref]
- Gristina AG, Wilson PD (1964) Popliteal cysts in adults and children. A review of 90 cases. Arch Surg 88: 357-363. [Crossref]
- Miller TT, Staron RB, Koenigsberg T, Levin TL, Feldman F (1996) MR imaging of Baker cysts: association with internal derangement, effusion, and degenerative arthropathy. Radiology 201: 247-250. [Crossref]
- Herman AM, Marzo JM (2014) Popliteal cysts: a current review. Orthopedics 37: e678-e684. [Crossref]
- Fritschy D, Fasel J, Imbert JC, Bianchi S, Verdonk R et al. (2006) The popliteal cyst. Knee Surg Sports Traumatol Arthrosc 14: 623-628. [Crossref]
- Drees C, Lewis T, Mossad S (1999) Baker's cyst infection: case report and review. Clin Infect Dis 29: 276-278. [Crossref]
- Austin KS, Testa NN, Luntz RK, Greene JB, Smiles S (1992) Aspergillus infection of total knee arthroplasty presenting as a popliteal cyst: Case report and review of the literature. J Arthroplasty 7: 311-314. [Crossref]
- Krawzak HW, Scherf FG, Bong J, Hohlbach G (1994) Baker’s cyst in osteoarticular tuberculosis of the knee joint. Dtsch Med Wochenschr 119: 1579-1582. [Crossref]
- Mannino M, Marino C, Chawla K (1988) Ruptured pyogenic Baker’s cyst. J Natl Med Assoc 80: 1018-1019. [Crossref]
- Bert F, Bariou Lancelin M, Lambert Zechovsky N (1998) Clinical significance of bacteremia involving the "Streptococcus milleri" group: 51 cases and review. Clin Infect Dis 27: 385-387. [Crossref]
- Stelzmueller I, Pfausler B, Fille M, Dossett LA, Bonatti H (2009) Streptococcus milleri group isolates from blood cultures: consider surgical sepsis. Surg Infect (Larchmt) 10: 259-263. [Crossref]
- Wanahita A, Goldsmith EA, Musher DM, Clarridge JE 3rd, Rubio J et al. (2002) Interaction between human polymorphonuclear leukocytes and Streptococcus milleri group bacteria. J Infect Dis 185: 85-90. [Crossref]
