A Step-By-Step Approach of the In Situ Thin Split-Thickness Toe-Nail Bed-Graft for the Treatment of Subungual Exostosis
A B S T R A C T
Subungual exostosis (SE) is a rather uncommon benign bony outgrowth of the distal phalanx of the toes, affecting mainly adolescents and young adults. While inherently painless, it grows progressively and leads to nail deformity which eventually produces pain and has negative impact on the quality of life of the affected individual. The present paper presents a step-by-step guide to the in situ split-thickness toenail bed graft technique. The outcome of our case was in line with the current literature, the preservation of the nail led to a highly satisfactory cosmetic result, while no recurrence of the lesion was reported.
Keywords
Subungual exostosis, surgical excision, surgical technique
Introduction
Subungual exostosis (SE), first described by Dupuytren as early as in 1847, is a rather uncommon benign bony outgrowth of the distal phalanx of the toes, affecting mainly adolescents and young adults [1, 2]. SE is commonly located at the hallux, while other toes and fingers can rarely be affected [2, 3]. It is usually an isolated lesion but can also be a manifestation of inherited disorders. While inherently painless, it grows progressively and applies pressure on the nail plate, leading to onychodystrophy and toe deformity which eventually produces pain and has negative impact on the quality of life of the affected individuals.
The exact aetiology of the disease remains obscure with repetitive trauma and chronic infection to represent the main associated factors. Some studies suggest that these factors lead to reactive metaplasia, but the identification of a chromosomal translocation involving collagen genes suggests a neoplastic aetiology [2, 4]. There is still controversy regarding the association of SE with osteochondroma. Histologically, the cartilage found in the SE is fibrocartilage, whereas osteochondroma is made of hyaline cartilage. These differences indicate that SE is possibly a distinct clinical entity and not a variation of osteochondoma [2]. The differential diagnosis includes infectious diseases, mainly fungal infections and both benign and malignant neoplasms. Definitive diagnosis can be quite challenging and therefore high clinical suspicion is required. Detailed history, clinical examination, radiologic examination, and histopathologic examination are all important parts of the diagnosis.
The mainstay of treatment of SE is surgical excision, usually with either total or partial excision of the nail [2, 5, 6]. Complete excision of the lesion is essential in order to avoid recurrence. Several techniques have been described over the years in an effort to produce successful results in combination with a satisfactory cosmetic appearance. The aim of the present paper is to present a step-by-step guide to the in situ split-thickness toenail bed graft technique, while preserving the nail.
Case Presentation
I History
Our patient is a young female, who at the time of her first visit was 21 years old. Her main complaint was a progressive, over the last 6 months, nail deformation of the hallux, which by that time caused her discomfort when wearing closed shoes. She did not report any trauma or infection, fungal or otherwise, of her big toe. The patient had already seen other surgeons who have suggested the removal of the lesion along with the nail, which was unacceptable for her.
II Clinical Examination
On clinical examination, almost two thirds of the nail were elevated, and a large mass was protruding centrally and medially (Figure 1).
III Radiological Imaging
On radiological examination, a big exostosis was sprouting from the distal medial part of the second phalanx of the hallux (Figure 2).
Figure 1: Clinical appearance of the elevated nail and the protruding mass.
Figure 2: Radiological appearance of the exostosis.
IV Surgical Technique
After surgical preparation of the site, a digital block with 1% lidocaine was performed and a finger tourniquet using a tight elastic ligature at the base of the thumb was applied, to control the bleeding. The nail was elevated from the medial and most of the proximal nail folds by means of a small periosteal elevator beneath the nail, while the rest of the proximal and lateral nail folds were kept intact. The protruding bony exostoses along with the pathologic nail bed were removed (Figure 3), a fine rongeur was used to remove any residual osteochondral tissue up to the normal bone tissue border and to smoothen the surface, leaving medially a big area of uncovered phalangeal bone (Figure 4). With a number 15 blade (Figure 4) a thin split-thickness layer of the healthy nail bed of the same toe, of similar size as the defect, was obtained (Figure 5). The nail bed graft was placed over the defect and sutured in place with 4-0 vicryl. (Figure 6).
Finally, the elevated nail was replaced under the proximal and medial nail folds onto the nail bed and kept in place by two sutures (Figure 7) to protect the graft and the donor-site area. The excised tissue was sent for biopsy which confirmed the diagnosis of subungual exostosis. A written consent was taken from the patient to report the results of her treatment.
Figure 3: Removed exostosis covered with nail bed.
Figure 4: A large area of uncovered bone is left medially. With a number 15 blade a thin split-thickness layer of healthy nail bed of the same toe, of similar size as the defect, is obtained.
Figure 5: The thin split-thickness layer of healthy nail bed.
Figure 6: Placement of the nail bed graft over the defect and suture application.
Figure 7: Replacement of the nail on to the nail bed, held with two sutures.
V Postoperative Follow-Up
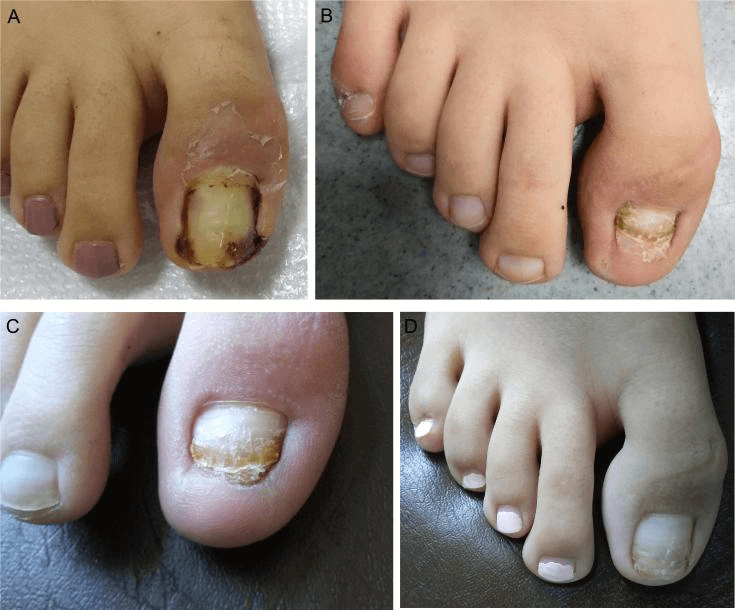
The sutures were removed at 3 weeks postoperatively (Figure 8A). The nail fell off at about 6 weeks leaving a well incorporated graft. At 3 months we could see that the graft area was almost indistinguishable to the healthy nail bed and there was no damage to the donor-site area (Figure 8B). At 6 months the nail had covered two thirds of the nail bed without lifting off or deformation (Figure 8C). At 11 months the nail has completely covered the nail bed (Figure 8D). The patient has reached the second year following the operation and has no signs of recurrence of the lesion.
Figure 8: A) At 3 weeks. B) At 3 months. C) At 6 months. D) At 11 months.
Discussion
Knowledge and understanding of nail anatomy is of utmost importance before attempting surgical procedures involving the nail. As already known, cell proliferation is derived from the nail matrix, especially the proximal half of the matrix. As a result, any trauma or surgical procedure involving the proximal matrix is more likely to cause scarring and subsequently onychodystrophy and poor cosmetic results [7, 8]. Trauma to the nail bed can cause onycholysis (non-adherence) to the nail or ingrowing of the nail [6, 9]. A nail requires three or four growth periods to improve its shape, volume and appearance.
Traditionally in the literature, nail excision, either complete or partial, is the most common treatment, leaving the toe without appropriate nail coverage during a period of 4-6 months until a new one grows in. Lokiec et al. described a partial onychectomy combined with relocation and suturing to the nail back over the raw bone surface, offering a natural coverage, with good cosmetic results [10]. A similar technique but with a mentioned, but somewhat obscure, repair of the damaged nail bed and refixation of the excised nail onto its bed was reported by Malkoc et al. [11]. Suga suggested that in the cases where the lesion was small a fish-mouth type incision of the nail-bed could be used with good cosmetic results but with a higher rate of recurrence, probably due to limited excision so as to be able to close the defect [6].
In the cases with a larger lesion, coverage of the defect has been attempted with artificial skin graft but with onycholysis or ingrown nail in all of the cases [6]. DaCambra et al. recently reported satisfactory outcomes with the use of VAC (vacuum Assisted Closure) in cases of large nail defects after excision [12].
The split-thickness nail-bed graft technique has been described mainly in the setting of large nail defects due to injury [13, 14]. The thin in situ split-thickness technique, described by Choi et al. in one case, uses a thin split-thickness graft from the adjacent non-injured nail-bed, thus decreasing the donor-site complications, with excellent result [15]. In the present paper we attempted to give a detailed step-by-step description of the surgical technique and the postoperative follow-up period. It is a very effective technique, especially in cases like ours where large excisions are needed in order to completely remove the lesion, as it enables tension-free wound healing. The preservation of the nail offers protection to the donor-site and the graft and leads to an excellent cosmetic result.
Conclusion
The outcome of our case was in line with the current literature, which supports the retention of the nail and the thin in situ split-thickness toe-nail bed-graft technique in large nail defects following SE excision. Our technique led to a highly satisfactory cosmetic result, while no recurrence of the lesion was reported.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Thu 04, Jun 2020Accepted: Mon 22, Jun 2020
Published: Fri 03, Jul 2020
Copyright
© 2023 Panagiotis G. Tsailas. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.07.03
Author Info
Chrysoula Argyrou Panagiotis G. Tsailas
Corresponding Author
Panagiotis G. Tsailas4th department of Orthopedic Surgery, KAT Hospital, Athens, Greece
Figures & Tables







References
- Dupuytren G LGCF (1847) On the Injuries and Diseases of Bones: Being Selections from the Collected Edition of the Clinical Lectures of Baron Dupuytren London: Sydenham Society.
- Mark P DaCambra, Sumit K Gupta, Fabio Ferri de Barros (2014) Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res 472: 1251-1259. [Crossref]
- Christina M Ward, Alison Dittmer (2013) Subungual exotosis of the finger: case report and review of the literature. Iowa orthop J 33: 228-231. [Crossref]
- Clelia Tiziana Storlazzi, Agnieszka Wozniak, Ioannis Panagopoulos, Raf Sciot, Nils Mandahl et al. (2006) Rearrangement of the COL12A1 and COL4A5 genes in subungual exostosis: molecular cytogenetic delineation of the tumor-specific translocation t(X;6)(q13-14;q22). Int J Cancer 118: 1972-1976. [Crossref]
- L de Palma, A Gigante, N Specchia (1996) Subungual exostosis of the foot. Foot Ankle int 17: 758-763. [Crossref]
- Hirotaka Suga, Masashi Mukouda (2005) Subungual exostosis: a review of 16 cases focusing on postoperative deformity of the nail. Ann Plast surg 55: 272-275. [Crossref]
- David de Berker (2013) Nail anatomy. Clin Dermatol 31: 509-515. [Crossref]
- D de Berker, B Angus (1996) Proliferative compartments in the normal nail unit. Br J Dermatol 135: 555-559. [Crossref]
- R Ravindra Bharathi, Babu Bajantri (2011) Nail bed injuries and deformities of nail. Indian J Plast Surg 44: 197‐202. [Crossref]
- F Lokiec, E Ezra, E Krasin, D Keret, S Wientroub (2001) A simple and efficient surgical technique for subungual exostosis. J Pediatr orthop 21: 76-79. [Crossref]
- Melih Malkoc, Ozgur Korkmaz, Mert Keskinbora, Ali Seker, Ismail Oltulu et al. (2016) Surgical treatment of nail bed subungual exostosis. Singapore M J 57: 630-633. [Crossref]
- Mark P DaCambra, Sumit K Gupta, Fabio Ferri de Barros (2013) A novel management strategy for subungual exostosis. BMJ Case Rep 30: 2013. [Crossref]
- Jianyun Yang, Tao Wang, Cong Yu, Yudong Gu, Xiaotian Jia (2017) Reconstruction of large area defect of the nail bed by cross finger fascial flap combined with split-thickness toe nail bed graft: A new surgical method. Medicine 96: e6048. [Crossref]
- Shang Chin Hsieh, Shao Liang Chen, Tim Mo Chen, Tiang Yeu Cheng, Hsian Jenn Wang (2004) Thin split-thickness toenail bed grafts for avulsed nail bed defects. Ann Plast Surg 52: 375-379. [Crossref]
- Chang Min Choi, Hee Ryung Cho, Bark Lynn Lew, Woo Young Sim (2011) Subungual exostosis treated with an in situ thin split-thickness toenail bed graft. Dermatol Ther 24: 452-254. [Crossref]
