Journals
Abdominal Aortic Aneurysm and Pheochromocytoma
A B S T R A C T
Simultaneous presentation of pheochromocytoma and abdominal aortic aneurysm (AAA) is uncommon and poses unique challenges. Based on the rare case reports, there may be an association with AAA development and rupture. The approach to these separate lesions requires medical management to prevent hypertensive crisis and cardiovascular collapse, decision whether to approach the pheochromocytoma laparoscopically or by open approaches, the decision to approach the AAA by open or endovascular repair (EVAR) and the sequence and timing of repair. We present a case of a female who had a biochemically active but clinical benign pheochromocytoma in conjunction with an AAA that was repaired simultaneously by an open approach
Keywords
Pheochromocytoma, abdominal aortic aneurysm, endovascular repair, open surgical repair
Introduction
Abdominal aortic aneurysm (AAA), typically defined as a transverse diameter of the infra-renal portion of the abdominal aorta > 3cm, is most commonly a consequence of degenerative atherosclerotic disease. Other risk factors include hypertension, nicotine abuse, hyperlipidemia and family history. The incidence increases after age 50, is 4-6 times more common in males with an incidence on screening of 2.2 – 5.5% of males [1]. Because of the risk of rupture, repair is recommended in men when > 5.5 cm and women > 5.0 cm [2]. However, females appear to have an increased risk of rupture, and the risk is increased in the setting of chronic lung disease, prompting many centers to adopt a more aggressive approach using a diameter of > 4.5 cm as an indication in females [1, 2]. Additional indications for intervention include “fast growth” which has included diameter increase > 0.5 cm/year [1]. Endovascular repair has become the standard approach, as it is generally associated with less complications and shorter length of stay, however the benefit is less clear in women. Women have more technically challenging anatomy, are more likely to require open repair, and have increased incidence of endoleaks and limb occlusion due to smaller length and diameter of the proximal landing zone (“neck”) [1]. Pheochromocytoma, a tumor of chromaffin cells, is present in < 1% of patients with hypertension [3]. Biochemically active tumors secrete catecholamines, which can be determined by documenting elevated plasma free metanephrines or 24-hour urinary metanephrines, require alpha-blockade prior to any surgical intervention to avoid hypertensive crisis and risk of cardiovascular collapse. However, even biochemically inert tumors can develop hypertensive crisis [4]. When resection is indicated, current reports support laparoscopic approaches when possible, including “large” (>5 cm) tumors [5, 6]. We present a case of a patient who presented with both AAA and biochemically active pheochromocytoma.
Case Report
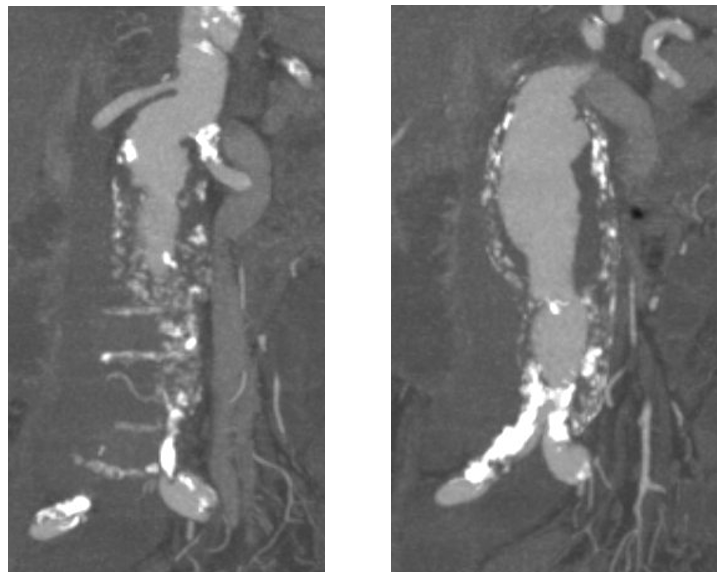
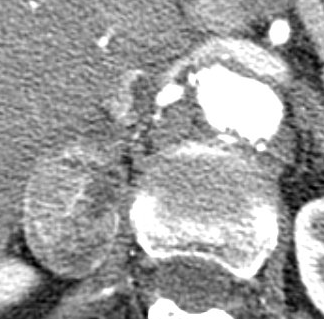
A 74-year-old female presented for routine follow up of an infra-renal abdominal aortic aneurysm. She had a history of smoking with moderate COPD, pulmonary fibrosis and hypertension controlled with two drugs. She did not require supplemental oxygen. She had mild claudication, no history of cardiac disease and had never undergone a surgical procedure. One year earlier an abdominal duplex had described her aneurysm as 5.0 cm in maximal diameter while CT described it as 4.7 cm. An incidental 3 x 3.6 x 4.0 cm right adrenal mass was also noted. On follow up CT angiography the maximal diameter of the infra-renal aorta was 5.0 cm (Figure 1). The adrenal mass was described as now being 4.9 x 2.9 cm in diameter and was hyper vascular (Figure 2). Subsequent CT PET scan showed localized uptake in the adrenal mass alone (SUV 5.9) and serum normetanephrines were 1683 pg/ml (normal less than 148).
Figure 1A: CT Coronal views demonstrating Abdominal Aortic Aneurysm proximal neck with tortuosity
Figure 1B: CT Coronal view demonstrating severe common iliac artery plaque and stenosis
Figure 2: CT Image of Right Adrenal Mass
The patient was a candidate for both adrenalectomy and repair of AAA. Our general surgeons felt uncomfortable performing laparoscopic adrenalectomy prior to repair of AAA. The patient had several issues that made an endovascular approach difficult. The left renal artery originated at the origin of the aneurysm, and she had bilateral critical iliac stenosis. She was not a candidate for commercially available fenestrated grafts, and the alignment of the renal arteries suggested that a snorkel approach (“parallel chimney graft”) had a high risk of endoleaks. She may have been a candidate for a “back table fenestrated graft” but we were concerned about her access vessels. As she was a candidate for open repair, we combined the two procedures after pre-operative alpha blockade with docosahexanic acid. We were prepared to perform a bypass to the left renal artery, but in the event were able to clamp just below the right renal and incorporate the left renal artery into the anastomosis, and post procedure she had excellent renal flow by doppler examination. We performed an aorto-bi-iliac bypass, but then had to add a jump graft to the right common femoral artery as her external iliac system was more severely diseased than we had anticipated. We performed the aortic repair first, as she had no hemodynamic lability and we were able to isolate the adrenal vessels and then the adrenal mass was resected. Postoperatively, she had transient hypotension responsive to low dose vasopressors, and made an uneventful recovery. The pathology of the mass was consistent with a 4 cm diameter pheochromocytoma.
Conclusion
The concomitant presentation of AAA and pheochromocytoma is unusual. In one relatively selected review of 50 patients with pheochromocytoma, one had concurrent AAA which did not require intervention [7]. It has been theorized that the presence of pheochromocytoma increases the risk of AAA development and rupture [3, 8]. Concurrent presentation has included in an asymptomatic fashion, as in our case, with rupture, and with “occult” pheochromocytoma which required post AAA repair study and resection [7-10]. When possible, ideally the adrenal tumor should be resected prior to AAA repair, with alpha-blockade, as even biochemically “inert” tumors can prompt hypertensive crisis [4, 10]. However, sometimes the sequence is reversed [8, 9].
There has been a trend towards favoring laparoscopic resection of pheochromocytoma and adrenal tumors in general [5, 6]. One contraindication would be need for open surgical exploration for another reason. Similarly, endovascular repair of AAA has become the predominant choice, largely replacing open repair. However, women have increased incidence of anatomic issues that make endovascular repair problematic, including disadvantaged necks and small iliac arteries as in this case [1]. It would be reasonable to have performed adrenalectomy first, but in this case, she was stable throughout, we had controlled the renal vein, and the general surgeons had a clear unobstructed view of the tumor.
The combine presence of AAA and pheochromocytoma is unusual. Staging and managing these lesions depend on determining whether the AAA is amenable to endovascular repair or not and requires an individualized approach. Our experience, and that reported in the literature, suggests that alpha-blockade should be considered in all patients, whether there is evidence of biochemical activity or not.
Conflicts of Interest
None of the authors have any financial or other conflict; this paper is not in consideration by other publications
Author’s Contributions
Riyad Karmy-Jones MD
GROUP 1: Conception of the work AND/OR Design of the work AND/OR Acquisition of data AND/OR Analysis of data AND/OR Interpretation of data.
GROUP 2: Drafting the work AND/OR Revising the work critically for important intellectual content.
GROUP 3: Final approval of the version to be published.
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Article Info
Article Type
Case ReportPublication history
Received: Fri 17, May 2019Accepted: Sat 01, Jun 2019
Published: Wed 12, Jun 2019
Copyright
© 2023 R. Karmy-Jones . This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2019.01.02
Author Info
Stephen Reese Beejay Feliciano R. Karmy-Jones Steven Matous
Corresponding Author
R. Karmy-JonesDivisions of Vascular Surgery, PeaceHealth Southwest Washington Medical Center, Vancouver WA
Figures & Tables
References
- Stoberock K, Kolbel T, Atihan G, Debus ES, Tsilimparis N et al. (2018) Gender differences in abdominal aortic aneurysm therapy - a systemic review. Vasa 47: 267-271. [Crossref]
- Davis FM, Jerzal E, Albright J, Kazmers A, Monsour A et al. (2019) Variation in the elective management of small abdominal aortic aneurysms and physician practice patterns. J Vasc Surg. [Crossref]
- SK Kota, LK Meher, S Jammula, S Mohapatra, KD Modi et al. (2013) Coexistence of pheochromocytoma with abdominal aortic aneurysm: An untold association. Ann Med Health Sci Res 3: 258-261. [Crossref]
- Gupta N, Brau K, Sasson A, Goldner W (2016) Biochemically silent pheochromocytoma presenting with hypertensive crisis during surgery. AACE clinical case Rep 2: e333-e336.
- Bai S, Yao Z, Zhu X, Li Z, Jiang Y et al. (2019) Comparison of transperitoneal laprascopic versus open adrenalectomy for large pheochromocytoma: A retrospective propensity score-matched cohort study. Int J Surg 61: 26-32. [Crossref]
- Feo CV, Maestroni U, Del Rio P, Severi S, Viani L, et al. (2016) Applicability of laparoscopic approach to the resection of large adrenal tumors: a retrospective cohort study on 200 patients. Surg Endosc 30: 3532-3540. [Crossref]
- Kota SK, Meher LK, Jammula S, Panda S, Modi KD et al. (2012) Coexistence of pheochromocytoma with uncommon vascular lesions. Indian J Endocrinol Metab 16: 962-971. [Crossref]
- Ehata T, Karasawa F, Watanabe K, Satoh T (1999) Unsuspected pheochromocytoma with abdominal aortic aneurysm--a case report. Acta Anaesthesiol Sin 37: 27-28. [Crossref]
- Arikan AA (2018) Ruptured abdominal aortic aneurysm with a suprarenal tumor. Braz J Cardiovas Surg 33: 522-524. [Crossref]
- Matadial C, Giquel J, Martinez-Ruiz R (2013) Concomitant elective resection of pheochromocytoma and repair of aortic abdominal aneurysm. J R Med Cardiovasc Dis 2: 2048004013493403. [Crossref]
