Journals
Application of a Bedtime Obturator Prosthesis for an Edentulous Patient with an Extensive Maxillary Defect
A B S T R A C T
One of the important objectives of prosthetic treatment is to preserve any remaining tissue. Prosthodontists generally instruct patients to remove their dentures at night, which allows the denture-supporting tissues to rest and provides an opportunity for cleaning the dentures. Removing the obturator prosthesis, however, results in open communication between the oral and nasal cavities, leading to psychological fear because of the disordered articulation. Additionally, latent pathogenic microorganisms can become highly colonized on obturator prostheses. To make it possible to remove the obturator without patient anxiety and ensure the opportunity for denture cleaning, we have advocated the application of a separate bedtime obturator that closes only the defect cavity. In this study, a newly designed, hollow bedtime obturator, which is retained by the undercut surrounding the defect and has a gingival clasp for removing it, was inserted in a 70-year-old edentulous patient with an extensive maxillary defect. Subjective and objective evaluations indicated that the bedtime obturator improved denture hygiene and nighttime quality of life of the patient. The concept of a separate bedtime obturator is a useful solution for the particular situation created by maxillectomy.
K E Y W O R D S
Hollow obturator, maxillectomy, gingival clasp, denture cleaning, quality-of-life outcome
I N T R O D U C T I O N
Obturator prostheses improve speech, mastication, and swallowing by reestablishing oronasal separation [1-4]. Wearing a stable obturator prosthesis contributes not only to functional recovery but also to improving the patient’s mood [5]. Removing the obturator prosthesis, however, results in open communication between the oral and nasal cavities, leading to psychological fear of dysfunctional speech and leakage of saliva [6, 7]. For these reasons, many obturator prosthesis wearers are uneasy about removing their dentures at night [7]. Additionally, latent pathogenic microorganisms such as Candida spp. and Staphylococcus spp. have been found to be highly colonized on the mucosal surface of obturator prostheses [8].
Thus, removing the dentures at night—alleviating anxiety and ensuring sufficient time for denture cleaning—are important for obturator prosthesis wearers to avoid the risk of systemic infection, resulting in deteriorating quality of life. To achieve this aim, it is necessary to take measures in accordance with the particular situation created by maxillectomy. This report evaluates the benefits of a newly designed, separate bedtime obturator that is retained by the undercut surrounding the defect and has a gingival clasp for removing it.
C l i n i c a l R e p o r t
A 70-year-old man living in a nursing home was referred to the Division of Denture Prosthodontics Restoration, Kagoshima University Hospital with complaints of mastication and speech disorders in June 2014. Intraoral examination revealed that his maxilla was edentulous, and there was a right maxillary defect (Fig. 1A). His mandibular dentition consisted of only the right canine and first premolar (Fig. 1B). There were no abutment teeth with which to support an obturator prosthesis (Fig. 1C, D), and the maxillary obturator prosthesis fell when he opened his mouth. Oral hygiene for the remaining teeth and dentures was poor. He had stuffed tissue paper into the areas of tooth loss and the obturator (Fig. 1B, D). We diagnosed masticatory dysfunction and articulation disorder caused by loss of the abutment teeth and defective dentures. The therapeutic strategy was as follows: (1) We planned to obtain functional recovery by developing a provisional obturator prosthesis from the old one and use it as a template for a definitive prosthesis. (2) We would provide sufficient oral hygiene instruction concerning his remaining teeth and dentures. (3) We designed a bedtime obturator that closed only a defect cavity to solve the following two problems: (a) the disordered articulation caused by removing the denture at night and (b) the negative effects on the remaining tissue caused by wearing the dentures all of the time [9-11].
To create a provisional obturator prosthesis, we refurbished the old obturator prosthesis while correcting the problems, including an additional tooth, extension of the denture base, occlusal reconstruction, and direct relining (Fig. 2A). We used the undercut areas surrounding the nostrils and soft palate to retain the obturator prosthesis [1] (Fig. 2A, arrow). After confirming functional recovery and improved oral hygiene, we began to fabricate the definitive prosthesis. To transfer information from the provisional obturator prosthesis to the definitive prosthesis, we used a dynamic impression method [12] and the matrix of the polished surface [13] using putty-type silicone rubber impression material. The hollow obturator prosthesis and a lower partial denture with cast clasps were inserted in October 2014 (Fig. 2C, D).
For fabricating a separate bedtime obturator, we made a master cast by creating an impression of the definitive obturator prostheses using type IV stone and a silicone rubber impression material to reproduce the mucosal surface of the definitive obturator prosthesis with a deep undercut. After removing the definitive obturator prosthesis from the master cast, a duplicate impression of the master cast was made. Type IV stone was poured for the duplicate cast. To make a hollow bulb obturator, we used a modification of the methods reported by Tanaka et al. [14] and Deogade et al., [15] as follows.
- A sheet of paraffin wax was attached to the defect area as a spacer (Fig. 3A). Four perforations of 3.5 mm diameter were made through the wax in the region of the defect. Four plastic rods (Plastic casting bar; Ishifuku Metal Co., Tokyo, Japan) were placed in the perforation and allowed to project approximately 7 mm to act as the retainer of the core index (Fig. 3A arrow).
- A core index was fabricated by pouring an equal amount of type II stone and cristobalite investment within the waxed defect area. After the core index hardened, wax forms of the palatal portion and gingival clasp were made (Fig. 3B).
- After the wax obturator was cured, the plastic rods were removed. The core index material was removed from the escape holes where the plastic rod had been removed. The escape holes were closed with auto polymerizing resin.
The hollow bedtime obturator was polished and inserted in December 2014 (Fig. 3C, D). It was retained by the undercuts of the defect cavity and had a gingival clasp made of resin in the anterior region for removing it (arrow in Fig. 3C, D). The patient was instructed to wear this prosthesis only at night. No clinical problems were observed for either the definitive obturator prosthesis or the bedtime obturator at the 3-year follow-up.
Figure 4 shows the results of the objective and subjective evaluations for the definitive obturator prosthesis and bedtime obturator. The blowing ratio, used to evaluate oronasal separation, was determined by dividing the blowing time with the nose open by the blowing time with the nose closed [16]. The bedtime obturator had the same value as that of the definitive obturator prosthesis. The hygiene index [17] was used to evaluate biofilm distribution over the mucosal surface of the definitive obturator prosthesis before and after application of the bedtime obturator. The hygiene index after application of the bedtime obturator was improved from fair to excellent. A 100-mm visual analog scale was used to assess his ability to speak, the aesthetics, general satisfaction, anxiety associated with removing the denture at night, and denture cleaning at night. The original faces scale was used to assess patient mood [5]. The results showed that the bedtime obturator had improved nighttime quality of life and mood (Figure 4).
Figures
Figure 1A,B: Intraoral views at the first examination. C. Intraoral views with old obturator prosthesis. D. Old obturator prosthesis. The soft relining material around the obturator had deteriorated. The patient had stuffed tissue paper into the areas of tooth loss and the obturator
Fig. 2 A Provisional obturator prosthesis. We used the undercut of the defect to retain the provisional obturator prosthesis (arrows). B. Dynamic impression method and the matrix of the polished surface using putty-type silicone rubber impression material were used to transfer information to the definitive prosthesis. C. Intraoral views with the definitive obturator prosthesis. D. Definitive obturator prosthesis.
Fig. 3 A 3.5 mm diameter plastic rods were placed into the perforation to act as the retainer of the core index. B. Wax bedtime obturator. After a core index was fabricated, a wax form of the palatal part and gingival clasp were made. C. Occlusal and mucosal surfaces of the hollow obturator for bedtime use. The obturator had a gingival clasp made of resin in the anterior region for removing the device. (arrows) D. Intraoral view. The obturator was retained by the undercuts of the defect cavity
Fig. 4 Results of all objective and subjective evaluations
D i s c u s s i o n
Removing the obturator prosthesis at night results in open communication between the oral and nasal cavities, leading to psychological fears [6, 7]. Although we had instructed our patient to remove his dentures at night [9-11], he wanted to wear them all of the time for smooth conversation because he was often awakened at night for routine care of the facility’s residents. The continuous wearing of dentures may have a negative effect on residual tissues [9-11]. Removing dentures at night ensures an opportunity for denture cleaning to avoid the risk of systemic infection [8]. To solve the articulation disorder caused by removing the dentures and the negative effects on the remaining tissue caused by wearing them, we designed a bedtime obturator that closed only the defect cavity.
To the best of our knowledge, this case report was the first study to examine the effect of a bedtime obturator. That the blowing ratio for the bedtime obturator was the same as that for the definitive obturator indicates that sufficient oronasal separation was obtained. To fabricate the bedtime obturator, we made a master cast using the definitive obturator prosthesis. Avoiding the need to making an additional impression of an extensive maxillary defect reduces the burden on both the prosthodontist and the patient. Because the bedtime obturator is the same form as the definitive obturator prosthesis, adjustment after insertion is slight. Also, compared with wearing the definitive obturator prosthesis all night, it is less harmful to the remaining tissue because it is covers only a small area of the maxilla.
Because the bedtime obturator is retained by the undercut area surrounding the defect cavity, the time after surgery should be considered. In the present case, the patient had undergone maxillectomy 15 years earlier and the wound had healed completely.
It has been reported that the open, hollow obturator has advantages, such as ease of fabrication and adjustment [1, 18, 19]. The open, hollow obturator, however, also has disadvantages, such as difficulty with polishing and cleaning, leading to accumulation of food or debris inside the hollow portion [1, 18, 19]. Therefore, we fabricated a closed, hollow obturator for use as both the definitive obturator and the bedtime obturator.
Numerous methods have been reported for fabricating hollow bulb obturators [14, 15, 18-20]. A major method of fabricating a closed, hollow obturator is processing the obturator in separate segments and then luting them with auto polymerizing resin [20]. This method creates a broad sealed area, which is a potential site of leakage [19]. A one-step polymerization technique has been reported that uses a thermoforming unit [18, 19] or a polyurethane form [14] as the core index. This method, however, requires complex and multiple laboratory procedures. Additionally, to prevent deformation of a small, hollow index, the polymerizing pressure was set at a lower pressure than the manufacturer’s recommendation [18]. In the present case, with the help of a plastic rod to support the core index [14], we set the polymerizing pressure according to the manufacturer’s recommendation.
C o n c l u s i o n
Within the limitation of the short-term follow-up in this case, our findings suggest that application of a newly designed bedtime obturator for a post-maxillectomy patient was a useful solution for the particular situation created by maxillectomy.
Article Info
Article Type
Clinical ReportPublication history
Received: Mon 12, Mar 2018Accepted: Fri 23, Mar 2018
Published: Mon 02, Apr 2018
Copyright
© 2023 Mamoru Murakami. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOCR.2018.10.003
Author Info
Mamoru Murakami Masahiro Nishimura Takaharu Shimizu Yasuhiro Nishi Yoshihisa Takenouchi
Corresponding Author
Mamoru MurakamiDenture Prosthodontics Restoration, Advanced Dentistry Center, Kagoshima University Hospital, 8-35-1 Sakuragaoka, Kagoshima 890-8544, Japan
Figures
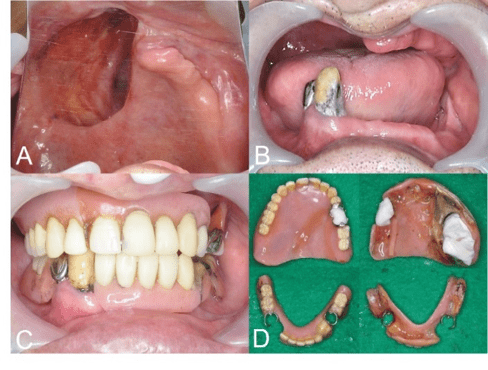
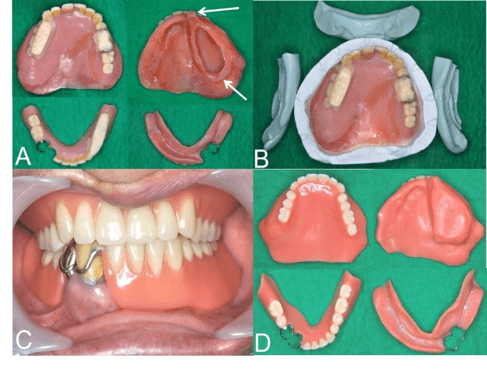
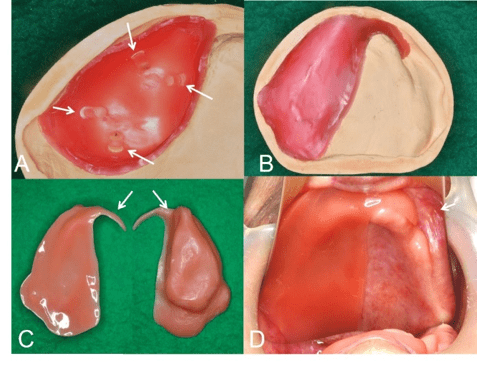
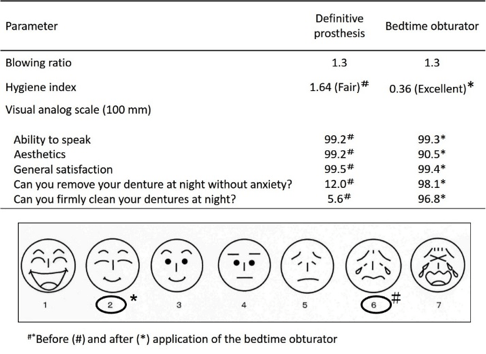
Figure legends
Fig. 1 A, B Intraoral views at the first examination. C. Intraoral views with old obturator prosthesis. D. Old obturator prosthesis. The soft relining material around the obturator had deteriorated. The patient had stuffed tissue paper into the areas of tooth loss and the obturator
Fig. 2 A Provisional obturator prosthesis. We used the undercut of the defect to retain the provisional obturator prosthesis (arrows). B. Dynamic impression method and the matrix of the polished surface using putty-type silicone rubber impression material were used to transfer information to the definitive prosthesis. C. Intraoral views with the definitive obturator prosthesis. D. Definitive obturator prosthesis.
Fig. 3 A 3.5 mm diameter plastic rods were placed into the perforation to act as the retainer of the core index. B. Wax bedtime obturator. After a core index was fabricated, a wax form of the palatal part and gingival clasp were made. C. Occlusal and mucosal surfaces of the hollow obturator for bedtime use. The obturator had a gingival clasp made of resin in the anterior region for removing the device. (arrows) D. Intraoral view. The obturator was retained by the undercuts of the defect cavity
Fig. 4 Results of all objective and subjective evaluations
References
1. Keyf F (2001) Obturator prostheses for hemimaxillectomy patients. J Oral Rehabil 28: 821-829. [Crossref]
2. Koyama S, Sasaki K, Inai T, Watanabe M (2005) Effects of defect configuration, size, and remaining teeth on masticatory function in post-maxillectomy patients. J Oral Rehabil 32: 635-641. [Crossref]
3. Matsuyama M, Tsukiyama Y, Tomioka M, Koyano K (2007) Subjective assessment of chewing function of obturator prosthesis wearers. Int J Prosthodont 20: 46-50. [Crossref]
4. Rieger J, Wolfaardt J, Seikaly H, Jha N (2002) Speech outcomes in patients rehabilitated with maxillary obturator prostheses after maxillectomy: a prospective study. Int J Prosthodont 15: 139-144. [Crossref]
5. Murakami M, Nishi Y, Umezono M, Kamashita Y, Nishimura M (2015) Fabrication of a movable obturator following maxillary reconstruction with slit-shaped fenestration. J Prosthodont 24: 254-259. [Crossref]
6. Beumer J III, Curtis TA, Firtell DN (1979) Maxillofacial Rehabilitation–Prosthodontic and Surgical Considerations. St. Louis, Mosby 188-243.
7. Toki S, Sugisaki H, Seto J, et al. (2006) Oral care for patients with maxillary defects by a dental hygienist. Maxillofac Prosthetics 29: 35-40.
8. Murakami M, Nishi Y, Seto K, Kamashita Y, Nagaoka E (2015) Dry mouth and denture plaque microflora in complete denture and palatal obturator prosthesis wearers. Gerodontology 32: 188-194. [Crossref]
9. Zarb GA, Bolender CL, Carlsson GE (1997) Boucher’s Prosthodontic Treatment for Edentulous Patients (ed 11). St. Louis, Mosby 30-45, 358-389.
10. Osborne J, Alexander G (1981) Partial Dentures (ed 4). Osney Mead, Oxford, UK, Blackwell Scientific, 387-401.
11. McGivney GP, Carr AB (2000) Removable Partial Prosthodontics (ed 10). St. Louis, Mosby 437-449.
12. Tryde G, Olsson K, Jensen SA, et al. (1965) Dynamic impression methods. J Prosthet Dent 15: 1023-1034.
13. Lott F, Levin B (1966) Flange technique: an anatomic and physiologic approach to increased retention, function, comfort, and appearance of dentures. J Prosthet Dent 16: 394-413. [Crossref]
14. Tanaka Y, Gold HO, Pruzansky S (1977) A simplified technique for fabricating a lightweight obturator. J Prosthet Dent 38: 638-642. [Crossref]
15. Deogade SC, Mantri SS, Naitam D, et al. (2013) A direct investment method of closed two-piece hollow bulb obturator. Case Rep Dent 2013: 326530
16. Katoh C, Saitoh M, Tsuneyuki M, Tanimoto H, Hashikawa K, et al. (2010) Blowing ratio as an evaluation tool for velopharyngeal function after oral and oropharyngeal cancer resection. Head Neck 32: 1012-1018. [Crossref]
17. Paranhos Hde F, da Silva CH, Venezian GC, Macedo LD, de Souza RF (2007) Distribution of biofilm on internal and external surfaces of upper complete dentures: the effect of hygiene instruction. Gerodontology 24: 162-168. [Crossref]
18. Hori K, Miyamoto T, Ono T, Yamamoto M, Shiroshita N, et al. (2013) One step polymerizing technique for fabricating a hollow obturator. J Prosthodont Res 57: 294-297. [Crossref]
19. Buzayan MM, Ariffin YT, Yunus N (2013) Closed hollow bulb obturator—one-step fabrication: a clinical report. J Prosthodont 22: 591-595. [Crossref]
20. McAndrew KS, Rothenberger S, Minsley GE (1998) 1997 Judson C. Hickey Scientific Writing Awards. An innovative investment method for the fabrication of a closed hollow obturator prosthesis. J Prosthet Dent 80: 129-132. [Crossref]
