Journals
Bariatric Surgery Conversions at a Revisional Referral Center: A Subset Analysis of Clinical Outcomes from a Rural Community Hospital Accredited Program
A B S T R A C T
Introduction: Revisional bariatric surgery for complications and weight regain is associated with higher morbidity and mortality rates compared to primary bariatric surgery. The majority of procedures are done in an urban setting.
Methods: A retrospective chart review with IRB approval was conducted in a rural community hospital accredited bariatric program. A total of 53 revisions were performed by a single surgeon from February 2019 to February 2020. A subset analysis of 18 bariatric surgery conversions was performed and its outcomes are presented. Primary outcomes were 30-day morbidity and mortality. Secondary outcomes included anastomotic or staple line leak, intraabdominal abscess and need for subsequent surgery.
Results: Most patients were female (83.3%) and the median ASA class was 3. The mean age was 48.2 ± 13.3 years. Most conversions were performed laparoscopically (88.9%), with a minority done robotically (11.1%). There were no open procedures or conversions to open. The most common prior bariatric operation was a sleeve gastrectomy (SG) (44.4%) followed by vertical banded gastroplasty (VBG) (22.2%). The most common type of operation was laparoscopic SG conversion to Roux-en-Y gastric bypass (RYGB) (16.7%) followed by laparoscopic VBG conversion to RYGB (16.7%). History of tobacco use was present in 38.9% of patients. The most common preoperative comorbidity was severe gastroesophageal reflux disease (GERD) (88.9%). The 30-day morbidity was 33.3% and there was no mortality. There were no anastomotic or staple line leaks. Intraabdominal abscess developed in 11.1% of patients. The rate of marginal ulceration was 27.8%, with only one case (5.6%) requiring future gastrojejunostomy revision. The rate of subsequent surgery beyond 30 days was 22.2%.
Conclusion: With an acceptable complication rate, no anastomotic or staple line leaks, and no mortality, minimally invasive bariatric surgery conversions are feasible and safe in a rural community hospital environment, with the most common indication being complications from a prior laparoscopic SG, and with the RYGB being the most common procedure as an end product of conversion.
Keywords
Revisions, conversions, bariatric surgery, community hospital, rural, laparoscopic, robotic
Introduction
The long-term benefits of metabolic and bariatric surgery and its proven effects on obesity-related comorbidities have been established by multiple publications, which include the development of Enhanced Recovery After Surgery (ERAS) protocols to optimize patient outcomes [1, 2]. Nevertheless, there is still a considerable degree of variability in terms of reporting outcomes among centers [3]. The super-specialty of revisional bariatric surgery has typically been studied within the academic hospital environment, although a significant portion of more recent studies has been conducted in the community hospital arena [4]. The application of robotic computer-assisted surgical platforms to revisional bariatric surgery has facilitated improved outcomes based on the ergonomic advantages offered by such technology to the surgeon [5]. Bariatric surgery revisions can be classified into reconstructions, conversions, reversals, removals or explanations, staged procedures and endoscopic procedures (endoscopic bariatric therapies, interventional bariatric endoscopy or endo-bariatrics). Particularly with conversions, multiple series have studied whether it is wise to convert an adjustable gastric band (AGB) to a Roux-en-Y gastric bypass (RYGB) or to a sleeve gastrectomy (SG) and whether it should be done in one or two stages. The literature favors the RYGB with either a one or a two-stage approach [6-8].
A conversion of SG to RYGB has been extensively studied due to the common complication of severe gastroesophageal reflux disease (GERD) with or without gastric sleeve stenosis as a contributing factor, with the RYGB being an effective therapy for such complication and for weight regain [9]. On the other hand, the RYGB is also the most effective product of conversion for complications after vertical banded gastroplasty (VBG) [10]. The RYGB can itself be converted to a biliopancreatic diversion with duodenal switch (BPD-DS) with acceptable outcomes [11]. Although revisional bariatric surgery is usually performed in urban centers or community hospitals, rural community programs do not typically conduct such complex operations, or if they do, the literature does not present a high volume of publications. This subset analysis study intends to determine whether performing revisional bariatric surgery, specifically conversions is feasible and safe in the rural community hospital environment. This question has not been extensively studied and therefore represents a novel topic and contribution.
Methods
With Institutional Review Board (IRB) approval from the Ethics Committee of Winchester Medical Center, a 495-bed rural community hospital, a retrospective chart review was conducted. The hospital and its program accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) acts as the primary referral center for a large rural community in the Shenandoah Valley of Virginia, USA. The retrospective review was done on a total of 53 consecutive bariatric surgery revisions over a 1-year period (February 2019 to February 2020) by a single fellowship-trained metabolic and bariatric surgeon. Out of that revision population, a subset analysis of 18 conversions was performed with attention to primary outcomes (30-day morbidity and mortality) along with secondary outcomes (anastomotic or staple line leaks, readmissions, intraoperative time, length of stay, intraabdominal abscess, marginal ulcers, need for subsequent surgery, among others). All procedures were performed in a minimally invasive fashion, either with the laparoscopic or with the robotic approach (da Vinci Xi or X platforms, Intuitive Surgical, Sunnyvale, CA, USA). A Bariatric Revisions Board multi-disciplinary conference was held for each case to be approved after the preoperative workup and counseling had taken place. The cases were performed only after a consensus had been reached by the expert panel.
Results
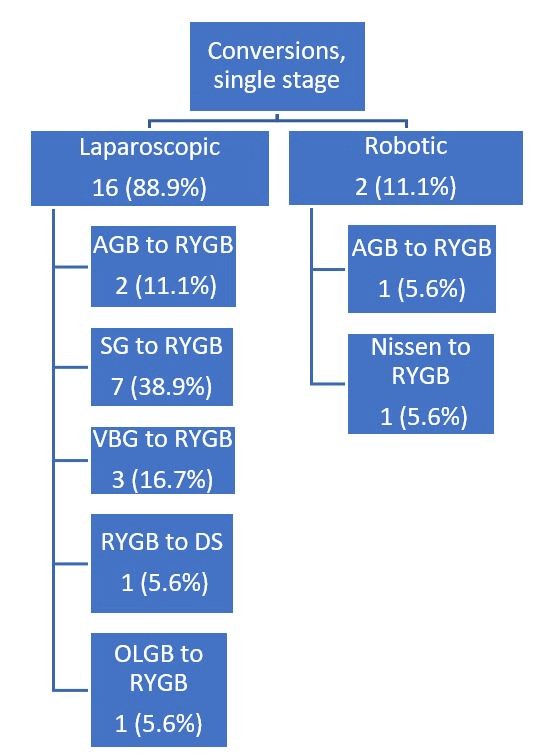
Figure 1 presents the type of procedures performed within this subset analysis of 18 patients from a total of 53 bariatric surgery revisions. Although the author’s preference is to use the robotic platform as much as possible, especially for revisions, it was not available for most of these operations. Therefore, most of the conversions were performed laparoscopically. Table 1 illustrates the patient demographics and the most important risk factors. Most patients were female (83.3%), and the median ASA class was 3. The mean age was 48.2 ± 13.3 years. The most common preoperative comorbidity was GERD (88.9%) followed by hypertension (44.4%). Tobacco use was present in 38.9% of patients.
Figure 1: Types of revisional bariatric conversions performed (n=18).
RYGB: Roux-en-Y gastric bypass; SG: Sleeve Gastrectomy; AGB: Adjustable Gastric Band; VBG: Vertical Banded Gastroplasty; DS: Duodenal Switch; OLGB: Omega-Loop Gastric Bypass.
Table 1: Patient demographics and risk factors (n=18).
|
Sex (F, M) |
15 (83.3%), 3 (16.7%) |
|
Age (mean ± SD) |
48.2 ± 13.3 years |
|
ASA class (median) |
3 |
|
Pre-op BMI (mean) |
38.9 ± 10.1 kg/m2 |
|
History of tobacco use |
7 (38.9%) |
|
Pre-op GERD |
16 (88.9%) |
|
Pre-op HTN |
8 (44.4%) |
|
Pre-op DM2 |
3 (16.7%) |
|
Pre-op OSA |
6 (33.3%) |
|
Pre-op CAD |
2 (11.1%) |
|
Pre-op CHF |
1 (5.6%) |
|
Pre-op CKD/ESRD |
2 (11.1%) |
|
Pre-op albumin (mean ± SD) |
3.8 ± 0.3 (g/dL) |
SD: Standard Deviation; ASA: American Society of Anaesthesiologists; BMI: Body Mass Index; GERD: Gastroesophageal Reflux Disease; HTN: Hypertension; DM2: Type 2 Diabetes Mellitus; OSA: Obstructive Sleep Apnea; CAD: Coronary Artery Disease; CHF: Congestive Heart Failure; CKD: Chronic Kidney Disease; ESRD: End-Stage Renal Disease.
Table 2: Primary outcomes (n=18).
|
30-day morbidity |
6 (33.3%) |
|
Mortality |
0 (0%) |
Table 2 demonstrates the primary outcomes. The 30-morbidity was 33.3%, corresponding to 6 patients who developed complications within the first 30 days. There was no mortality. Table 3 shows the primary outcomes that pertain to the hospital and office follow-up metrics, including the length of stay (LOS), intraoperative time, estimated blood loss (EBL), blood transfusions, conversions to open, post-operative body mass index (BMI), and change in BMI. As already mentioned, most conversions were performed laparoscopically (88.9%), with a minority done robotically (11.1%). There were no open procedures or conversions to open. Table 4 demonstrates the secondary outcomes that deal with complications. The most common complication was marginal ulceration (27.8%), with a 16.7% rate of endoscopic balloon dilation, and with only one patient (5.6%) requiring subsequent gastrojejunostomy reconstruction as a second revisional operation. There were no anastomotic or staple line leaks. The rate of intraabdominal abscess formation was 11.1%.
Table 3: Secondary outcomes: hospital and office follow-up metrics (n=18).
|
Intraoperative time (mean ± SD) |
174.2 ± 65.8 minutes |
|
Hospital LOS (mean ± SD) |
2.7 ± 1.9 days |
|
EBL (mean ± SD) |
106.7 ± 220.8 mL |
|
Blood transfusions |
1 (5.6%) |
|
Laparoscopic |
16 (88.9%) |
|
Robotic |
2 (11.1%) |
|
Conversions to open |
0 (0%) |
|
Follow-up duration (mean ± SD) |
6.0 ± 3.7 months |
|
Post-op BMI (mean ± SD) |
31.7 ± 7.7 kg/m2 |
|
BMI change (mean ± SD) |
-7.2 ± 4.3 BMI points |
SD: Standard Deviation; LOS: Length of Stay; EBL: Estimated Blood Loss; BMI: Body Mass Index.
Table 4: Secondary outcomes: complications and clinical events (n=18).
|
Anastomotic or staple line leak |
0 (0%) |
|
Intraabdominal abscess |
2 (11.1%) |
|
GJ marginal ulcers |
5 (27.8%) |
|
Marginal ulcers requiring balloon dilation |
3 (16.7%) |
|
Marginal ulcers requiring subsequent GJ reconstruction |
1 (5.6%) |
|
Hiatal hernia with obstruction requiring unexpected return to OR within 30 days |
1 (5.6%) |
|
Readmission within 30 days |
4 (22.2%) |
|
ED visits |
7 (38.9%) |
|
C diff colitis |
1 (5.6%) |
|
AKI |
1 (5.6%) |
|
Post-op intraabdominal bleeding |
2 (11.1%) |
|
Subsequent surgery beyond 30 days |
4 (22.2%) |
GJ: Gastrojejunostomy; OR: Operating Room; ED: Emergency Department; C diff: Clostridium difficile; AKI: Acute Kidney Injury.
Discussion
Revisional metabolic and bariatric surgery is a technically demanding super-specialty associated with higher complication rates, morbidity, and mortality compared to primary bariatric surgery. Most publications in the literature arise from academic centers or from urban community hospitals affiliated with academic institutions. However, in the rural community hospital environment, where affiliation with academic programs is less common and resources are limited, these complex procedures are not done frequently or, if they are, the outcomes have not been extensively reported. Moreover, the use of robotic technology in the rural community hospital environment and the reporting of its outcomes is another area where further clinical outcomes research is needed and where the author of this study has had extensive experience [12].
This study presents the results from a subset analysis of 18 minimally invasive conversions within a total population of 53 bariatric surgery revisions that were performed over a 1-year period by a single surgeon. The valuable experience from those 53 revisions in the rural community hospital setting will be published later and compared to 61 bariatric emergencies at the same institution by the author. From the same revisional population, a different subset analysis of 18 minimally invasive gastrojejunostomy reconstructions has been previously conducted and published. The results showed that marginal ulcer recurrence is common, but in most cases, it resolves with medical and endoscopic therapy after revisional surgery without the need for RYGB reversal. However, this rate of resolution comes at the expense of higher complication rates compared to primary surgery [13].
With respect to this subset analysis and study of bariatric surgery conversions, 100% of conversions were performed in one stage. The most common reason to undergo a conversion was the presence of complications from a prior SG, with severe GERD (27.8%) and an SG stricture (16.7%) being the main factor to consider conversion to RYGB. On the other hand, a prior VBG with obstruction from a proximal gastric stricture (11.1%), or with erosion into the gastric lumen (11.1%) was another common source of complications requiring conversion to RYGB. It can be seen from this study that although these procedures are complex, the rate of conversion to open was 0% and the rate of blood transfusion during hospitalization was low (5.6%). Although the RYGB was the most common product of conversions, there were no anastomotic or staple line leaks, and there was no mortality.
The third most common type of procedure performed was the conversion of an adjustable gastric band (AGB) to RYGB (11.1% laparoscopic, 5.6% robotic). There were less frequent conversion procedures such as omega-loop gastric bypass (OLGB) to classic RYGB (5.6%) and Nissen fundoplication to RYGB (5.6%). It is important to mention that, although weight regain was not the main reason to perform conversions in this patient population, there was a -7.2 ± 4.3 BMI point decrease corresponding to a mean follow-up of 6.0 ± 3.7 months. As can be seen, bariatric revisional surgery is still an effective therapy that promotes weight loss when performed for medical necessity, i.e., for complications after a prior primary bariatric operation rather than simple weight regain.
The rate of marginal ulceration at the gastrojejunostomy after an SG conversion to RYGB was high (27.8%), with 16.7% of patients requiring medical therapy with a proton pump inhibitor (PPI) and Carafate for cytoprotection with or without one to three endoscopic balloon dilations over a 3-month observation period. Only one patient (5.6%) failed this type of therapy, with refractory marginal ulcers that required a subsequent laparoscopic gastrojejunostomy revision a few months later and eventually with resolution, without requiring an RYGB reversal. It is important to be patient and try to avoid making a premature decision to return to the operating room since most marginal ulcers after revisional surgery will heal without the need for a second revision. The rate of intraabdominal abscess after conversions is not negligible (11.1%), but in both cases where this occurred, a percutaneous drainage with image-guidance by the interventional radiologist facilitated a faster recovery without the need for surgical intervention. This was accompanied by intravenous antibiotic therapy at home coordinated by the Infectious Diseases specialist in both instances.
Finally, the rate of subsequent surgery beyond 30 days is 22.2%, but only in one case (5.6%). This was directly related to the revisional procedure that was performed (SG to RYGB) due to marginal ulcers that did not heal with medical and endoscopic therapy. The other three cases corresponded to subsequent laparoscopic cholecystectomy, laparoscopic gastrostomy tube insertion to decompress an atonic gastric remnant in the patient with prior OLGB, and a diagnostic laparoscopy with closure of internal hernia. All these patients recovered from their surgeries without complications. There were several limitations associated with this study, such as its retrospective, single-center, single-surgeon nature, as well as its relatively short follow-up period (6.0 ± 3.7 months). Furthermore, the number of patients in this subset analysis (n=18) was modest, but at least it was enough to draw some helpful conclusions from this valuable experience. In the future, after the 53 bariatric surgery revisions are compared with the 61 bariatric surgery emergencies, more important conclusions will be drawn by analysing the morbidity and mortality from these two different types of bariatric procedures that are typically performed at experienced referral centers. The novelty of such as future publication will lie in the fact that it will be based on a rural environment experience, such as this subset analysis.
The most important lesson learned from this retrospective review is the observation that it is possible to perform complex revisional bariatric surgery in a rural community hospital setting as long as the surgeon’s experience and the team’s level of expertise are matched by the hospital’s resources and commitment from its administrators. After all, revisional bariatric surgery is a professional line of work that serves the community. Of course, the most important resource is not the type of minimally invasive platform, but the human component of the equation, which is irreplaceable when experience is considered the most valuable asset. Therefore, it is feasible and safe to perform bariatric surgery revisions (including conversions) with relatively low morbidity and no mortality in this setting regardless of geographic location or lack of academic affiliation, as long as all of the necessary elements are in place to deal with future complications.
Conclusion
With relatively low morbidity and no associated mortality, it is feasible to perform minimally invasive revisional bariatric surgery conversions in a rural community hospital setting. The most common indication is severe GERD with complications from a prior SG, and the most common product of conversion is the RYGB.
Conflicts of Interest
None.
Disclosure
Dr. Oviedo does not have any financial ties to disclose.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 06, Jul 2020Accepted: Wed 15, Jul 2020
Published: Sat 25, Jul 2020
Copyright
© 2023 Rodolfo J. Oviedo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.03.04
Author Info
Corresponding Author
Rodolfo J. OviedoTexas Bariatric Specialists, San Antonio, Texas, USA
Figures & Tables
Table 1: Patient demographics and risk factors (n=18).
|
Sex (F, M) |
15 (83.3%), 3 (16.7%) |
|
Age (mean ± SD) |
48.2 ± 13.3 years |
|
ASA class (median) |
3 |
|
Pre-op BMI (mean) |
38.9 ± 10.1 kg/m2 |
|
History of tobacco use |
7 (38.9%) |
|
Pre-op GERD |
16 (88.9%) |
|
Pre-op HTN |
8 (44.4%) |
|
Pre-op DM2 |
3 (16.7%) |
|
Pre-op OSA |
6 (33.3%) |
|
Pre-op CAD |
2 (11.1%) |
|
Pre-op CHF |
1 (5.6%) |
|
Pre-op CKD/ESRD |
2 (11.1%) |
|
Pre-op albumin (mean ± SD) |
3.8 ± 0.3 (g/dL) |
SD: Standard Deviation; ASA: American Society of Anaesthesiologists; BMI: Body Mass Index; GERD: Gastroesophageal Reflux Disease; HTN: Hypertension; DM2: Type 2 Diabetes Mellitus; OSA: Obstructive Sleep Apnea; CAD: Coronary Artery Disease; CHF: Congestive Heart Failure; CKD: Chronic Kidney Disease; ESRD: End-Stage Renal Disease.
Table 2: Primary outcomes (n=18).
|
30-day morbidity |
6 (33.3%) |
|
Mortality |
0 (0%) |
Table 2 demonstrates the primary outcomes. The 30-morbidity was 33.3%, corresponding to 6 patients who developed complications within the first 30 days. There was no mortality. Table 3 shows the primary outcomes that pertain to the hospital and office follow-up metrics, including the length of stay (LOS), intraoperative time, estimated blood loss (EBL), blood transfusions, conversions to open, post-operative body mass index (BMI), and change in BMI. As already mentioned, most conversions were performed laparoscopically (88.9%), with a minority done robotically (11.1%). There were no open procedures or conversions to open. Table 4 demonstrates the secondary outcomes that deal with complications. The most common complication was marginal ulceration (27.8%), with a 16.7% rate of endoscopic balloon dilation, and with only one patient (5.6%) requiring subsequent gastrojejunostomy reconstruction as a second revisional operation. There were no anastomotic or staple line leaks. The rate of intraabdominal abscess formation was 11.1%.
Table 3: Secondary outcomes: hospital and office follow-up metrics (n=18).
|
Intraoperative time (mean ± SD) |
174.2 ± 65.8 minutes |
|
Hospital LOS (mean ± SD) |
2.7 ± 1.9 days |
|
EBL (mean ± SD) |
106.7 ± 220.8 mL |
|
Blood transfusions |
1 (5.6%) |
|
Laparoscopic |
16 (88.9%) |
|
Robotic |
2 (11.1%) |
|
Conversions to open |
0 (0%) |
|
Follow-up duration (mean ± SD) |
6.0 ± 3.7 months |
|
Post-op BMI (mean ± SD) |
31.7 ± 7.7 kg/m2 |
|
BMI change (mean ± SD) |
-7.2 ± 4.3 BMI points |
SD: Standard Deviation; LOS: Length of Stay; EBL: Estimated Blood Loss; BMI: Body Mass Index.
Table 4: Secondary outcomes: complications and clinical events (n=18).
|
Anastomotic or staple line leak |
0 (0%) |
|
Intraabdominal abscess |
2 (11.1%) |
|
GJ marginal ulcers |
5 (27.8%) |
|
Marginal ulcers requiring balloon dilation |
3 (16.7%) |
|
Marginal ulcers requiring subsequent GJ reconstruction |
1 (5.6%) |
|
Hiatal hernia with obstruction requiring unexpected return to OR within 30 days |
1 (5.6%) |
|
Readmission within 30 days |
4 (22.2%) |
|
ED visits |
7 (38.9%) |
|
C diff colitis |
1 (5.6%) |
|
AKI |
1 (5.6%) |
|
Post-op intraabdominal bleeding |
2 (11.1%) |
|
Subsequent surgery beyond 30 days |
4 (22.2%) |
GJ: Gastrojejunostomy; OR: Operating Room; ED: Emergency Department; C diff: Clostridium difficile; AKI: Acute Kidney Injury.
RYGB: Roux-en-Y gastric bypass; SG: Sleeve Gastrectomy; AGB: Adjustable Gastric Band; VBG: Vertical Banded Gastroplasty; DS: Duodenal Switch; OLGB: Omega-Loop Gastric Bypass.
References
- Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ et al. (2014) Bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg 149: 275-287. [Crossref]
- Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D et al. (2016) Guidelines for perioperative care in bariatric surgery: Enhance Recovery After Surgery (ERAS) Society recommendations. World J Surg 40: 2065-2083. [Crossref]
- Ibrahim AM, Ghaferi AA, Thumma JR, Dimick JB (2017) Variation in outcomes at Bariatric Centers of Excellence. JAMA Surg 152: 629-636. [Crossref]
- Fourman MM, Saber AA (2012) Robotic bariatric surgery: a systematic review. Surg Obes Relat Dis 8: 483-488. [Crossref]
- Buchs NC, Pugin F, Azagury DE, Huber O, Chassot G et al. (2014) Robotic revisional bariatric surgery: a comparative study with laparoscopic and open surgery. Int J Med Robot 10: 213-217. [Crossref]
- Dang JT, Switzer NJ, Wu J, Gill RS, Shi X et al. (2016) Gastric band removal in revisional bariatric surgery, one-step versus two-step: a systematic review and meta-analysis. Obes Surg 26: 866-873. [Crossref]
- Creange C, Jenkins M, Pergamo M, Fielding G, Ren Fielding G et al. (2018) Gastric band conversion to Roux-en-Y gastric bypass shows greater weight loss than conversion to sleeve gastrectomy: 5-year outcomes. Surg Obes Relat Dis 14: 1531-1536. [Crossref]
- Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Sioka E et al. (2017) Roux-en-Y gastric bypass versus sleeve gastrectomy as revisional procedure after adjustable gastric band: a systematic review and meta-analysis. Obes Surg 27: 1365-1373. [Crossref]
- Landreneau JP, Strong AT, Rodriguez JH, Aleassa EM, Aminian A et al. (2018) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg 28: 3843-3850. [Crossref]
- Zakaria M, Elhoofy A (2018) Laparoscopic Roux-en-Y gastric bypass for failed vertical banded gastroplasty. Obes Surg 28: 3505-3510. [Crossref]
- Halawani HM, Bonanni F, Betancourt A, Antanavicius G (2017) Conversion of failed Roux-en-Y gastric bypass to biliopancreatic diversion with duodenal switch: outcomes of 9 case series. Surg Obes Relat Dis 13: 1272-1277. [Crossref]
- Oviedo RJ, Brownstein NC, Smith SL, Robertson JC, Nair Collins S (2018) First 200 robotic general surgery cases in a community hospital: a retrospective cohort study. World J Surg Surgical Res 1: 1034.
- Oviedo RJ (2020) Laparoscopic and robotic gastrojejunostomy revision for complications after Roux en Y gastric bypass: results from a high-volume referral center. Br J Gastroenterol 2: 145-149.
