Bilateral Post Traumatic Facial Nerve Palsy Presenting as Dysarthria: A Case Report
A B S T R A C T
Bilateral traumatic facial nerve palsy (FNP) is rare and can present with distressing features. We report a 23-year-old male final year medical student with a 10-day history of speech difficulty following a passenger motorcycle road traffic accident. Physical examination showed a fully conscious young man whose only neurological deficit was bilateral lower motor neuron facial nerve palsy (House and Brackmann grade IV) and difficulty pronouncing plosives. A high-resolution temporal bone CT showed a right longitudinal temporal bone fracture. There was no temporal bone fracture on the left side. Brain MRI was normal. He had complete recovery of facial nerve function on conservative management 6 months after the injury.
Keywords
Dysarthria, facial nerve paralysis, trauma, temporal bone fracture
Introduction
Bilateral facial nerve palsy (FNP) is rare, representing less than 2% of all cases of FNP [1]. Bilateral traumatic FNP is even rarer and can cause a diagnostic challenge due to lack of facial asymmetry as seen in unilateral FNP. Affected individuals may be devastated due to emotional and psychological distress as well as social limitations associated with it [2]. It can present with distressing features such as facial asymmetry, drooling of saliva, incomplete eye closure, exposure conjunctivitis, corneal ulceration, synkinesis, feeding difficulties and speech difficulties, which will lead to functional and aesthetic disability especially if full recovery is not achieved [3]. We report a rare case of bilateral facial nerve palsy presenting with dysarthria.
Case Report
We present a 23-year-old final year male medical student with a 10-day history of speech difficulty three days following a road traffic accident. He had transient loss of consciousness following the accident. There was no history of bleeding from any craniofacial orifice, seizures, limb weakness, hearing or swallowing difficulties, tinnitus or vertigo. There was no associated impaired lacrimation in both eyes, hyperacusis and taste disturbance in anterior two-third of tongue. However, there was a history of dryness of the tongues. He received initial care at a local hospital and was later referred to our facility for evaluation and treatment. Physical examination showed a young man with vital signs within limits of normal. He was fully conscious. He had dysarthria with difficulty in pronouncing plosives. His memory and other higher cerebral functions were preserved. He had bilateral lower motor neuron FNP (H&B grade IV) as evidenced by expressionless face and inability to close both eyelids. Hearing was grossly preserved bilaterally using Weber’s and Rhine’s tests. Pure tone audiogram was not done.
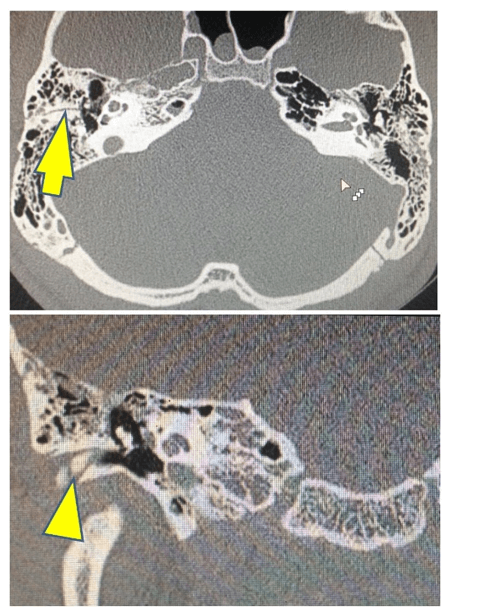
A high-resolution CT (HRCT) of the temporal bone showed a right longitudinal temporal bone fracture. There was no temporal fracture on the left side (Figure 1). Brain MRI showed no parenchymal brain injury/space occupying lesion or cerebellopontine angle lesion. Electrodiagnostic studies were not done due to unavailability. Hematological investigation results were within limits of normal. He was managed with high dose steroids and corneal protection measures. Complete improvement in FN function with significant improvement in speech has been observed 6 months after the injury (Figure 3), with the left recovering faster than the right side (Figure2).
Figure 1: High resolution petrous bone CT showing a right longitudinal fracture (Yellow arrows). There was no demonstrable fracture on the left. Preferable to place scans side to side and merge all using paint. Consider adding coronal of the left side.
Figure 2: Picture of the patient showing partial and complete resolution of facial nerve palsy on the right and left respectively 5 months after injury (Kind permission of the patient was obtained for this image).
Figure 3: Picture of the patient showing bilateral complete resolution of facial nerve palsy. 6 months after injury (Kind permission of the patient was obtained for this image).
Discussion
Bilateral FNP presenting as dysarthria has rarely been reported in literature. The etiologies of facial nerve palsy range from infections, tumors, head injuries, degenerative diseases, vascular diseases, and idiopathic [4]. Trauma is a very rare cause of bilateral FNP. Traumatic FNP is often associated with temporal bone fractures: longitudinal (70-90%) or transverse according to their orientation with respect to the long axis of the petrous pyramid [1]. However, the incidence of FN trauma is higher with transverse fractures than with the longitudinal ones, 40-50% vs 15-20% [3]. FNP without petrous temporal bone fracture may be explained by FN edema as there was no fracture seen on the left in the index case (Figure 1) [1].
There are several factors contributing to FN nerve susceptibility to trauma including its length, course and vascular supply [5]. The FN emerges from the brainstem and enters the internal auditory canal to follow a long route through the petrous bone, traversing the narrow fallopian canal. The FN is subdivided into three segments within the fallopian canal: labyrinthine, tympanic and mastoid. The labyrinthine segment is the narrowest and shortest portion of fallopian canal, where the FN is highly vulnerable to trauma. Also, this portion is a transition watershed zone between blood supply from the vertebral and carotid artery systems. In addition, the FN occupies more than 80% of the available space in the labyrinthine location, where it is most likely that edema can compromise facial nerve function [3].
Traumatic FNP can be immediate or delayed (> 48h). It has been widely accepted that immediate FNP results commonly from a direct nerve impingement or transection from temporal bone fracture, and surgical exploration appears to be the treatment of choice in such instance. Delayed FNP is usually due to the pressure effect from edema within the fallopian canal and is best managed medically [6]. A HRCT of the temporal bone, which was done in the index case (Figure 1), is a useful diagnostic tool for traumatic facial nerve palsy, as it can visualize the fracture line and its relationship to the fallopian canal. The role of MRI should no longer be considered merely complementary in the management strategy. MRI is useful for direct visualization of the injured FN, enabling the detection of neural ischaemia or edema or an intraneural hematoma [7, 8]. MRI may also be useful to detect neoplasms compressing the seventh cranial nerve or cerebellopontine angle tumors. MRI in this case did not detect any lesion to explain the FNP other than direct trauma from the fractured bone and facial nerve edema. Electrodiagnostic studies may be used in FNP to assess prognosis [9]. However, this was not used in the index due to unavailability.
Although the management of post-traumatic facial nerve palsy is still controversial, it is widely accepted that surgical intervention is indicated for patients with acute onset and complete palsy. However, patients with delayed onset or incomplete palsy are usually treated with systemic steroids. Steroid, which was used in the management of the index case, has also been reported to have the potential of hastening the facial nerve recovery in the traumatic cases. Many researchers advocate no exploration for non-penetrating trauma for intra-temporal facial nerve palsy. However, late surgery has been advocated by some authors in cases of non-recovery within six months after trauma [10]. However, there is still lack of a high-level, evidence-based study to back-up this recommendation. Important prognostic factors are the severity of FNP and timing of onset, with the degree of palsy having a greater influence on recovery of function than the time of onset. Pre-intervention H&B’s grade more than IV, though backed by low-level evidence, has been shown to have worse prognosis [6]. The index case had a H&B of IV and was still able to achieve complete recovery of FN function with medical management. (Figure 3).
Conclusion
Bilateral FNP can be trauma-induced and may rarely present with disabling dysarthria even in the absence of extensive skull base fractures. Conservative management with steroids can result in return of complete facial nerve function.
Article Info
Article Type
Case ReportPublication history
Received: Tue 23, Jun 2020Accepted: Tue 14, Jul 2020
Published: Sat 18, Jul 2020
Copyright
© 2023 Ekuma ME. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.01.07
Author Info
Ekuma ME Ndubuisi CA Mezue W Ohaegbulam SC Ndafia MN
Corresponding Author
Ekuma MEMemfys Hospital for Neurosurgery, Enugu, Nigeria
Figures & Tables


References
- Pothiawala S, Lateef F (2012) Bilateral facial nerve palsy: a diagnostic dilemma. Case Rep Emerg Med 2012: 458371. [Crossref]
- Habib SS, Al Rouq F, Meo I (2015) Post-traumatic bilateral facial paralysis associated with temporal bone fracture. J Coll Physicians Surg Pak 2: S132-S133. [Crossref]
- Lee P, Liang C, Huang S, Liao H (2018) The outcome analysis of traumatic facial nerve palsy treated with systemic steroid therapy. J Craniofac Surg 29: 1842-1847. [Crossref]
- Teller DC, Murphy TP (1992) Bilateral facial paralysis: a case presentation and literature review. J Otolaryngol 21: 44-47. [Crossref]
- Chang CY, Cass SP (1999) Management of facial nerve injury due to temporal bone trauma. Am J Otol 20: 96-114. [Crossref]
- Melvin TN, Limb CJ (2008) Overview of facial paralysis: current concepts. Facial Plast Surg 24: 155-163. [Crossref]
- Jager L, Reiser M (2001) CT and MR imaging of the normal and pathologic conditions of the facial nerve. Eur J Radiol 40: 133-146. [Crossref]
- Rotondo M, D’Avanzo R, Natale M, Comforti R, Pascale M et al. (2010) Post-traumatic peripheral facial nerve palsy: surgical and neuroradiological consideration in five cases of delayed onset. Acta Neurochir (Wien) 152: 1705-1709. [Crossref]
- Guerrissi JO (1997) Facial nerve paralysis after intratemporal and extratemporal blunt trauma. J Craniofac Surg 8: 431-437. [Crossref]
- Darrouzet V, Duclos JY, Liguoro D, Truilhe Y, De Bonfils C et al. (2001) Management of facial paralysis resulting from temporal bone fractures: our experience in 115 cases. Otolaryngol Head Neck Surg 125: 77-84. [Crossref]
