Journals
Bronchial atresia in an accessory lobe caused tension pneumothorax
A B S T R A C T
We report a case in which bronchial atresia in an accessory lobe caused tension pneumothorax. The atretic bronchus was found in an accessory lobe (right S6) that had been incompletely isolated from the right lower lobe during the fetal period. The accessory lobe was overinflated, leading to bullous formation due to the trapping of air. Video-assisted excision of the posterior lobe was successfully performed without any perioperative complications. The pathological findings were compatible with congenital bronchial atresia. This is the first report of bronchial atresia in an accessory lobe. We must keep this lesson in mind because such cases can suddenly develop serious complications.
K E Y W O R D S
Pneumothorax, congenital bronchial atresia posterior, pulmonary lobe, accessory fissure
Background
Bronchial atresia is a rare developmental anomaly characterized by focal obliteration of a bronchus in association with hyperinflation of the distal lung [1-4]. Bronchial atresia can involve any lobe but most commonly occurs at the apicoposterior segment of the left upper lobe, followed by the right upper lobe [1, 2]. We report a case of bronchial atresia in an accessory lobe (right S6) that had been isolated from the right lower lobe during the fetal period.
Case Presentation
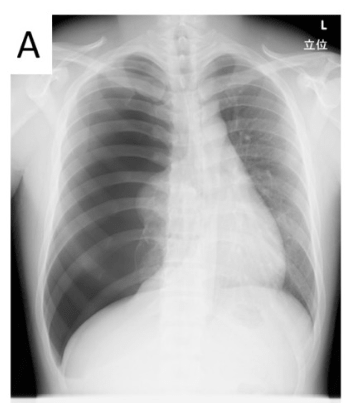
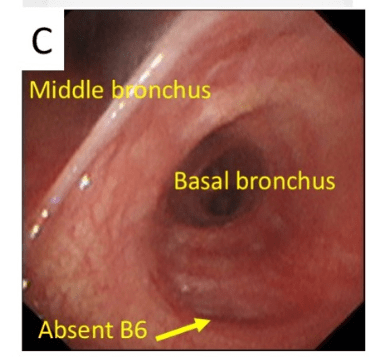
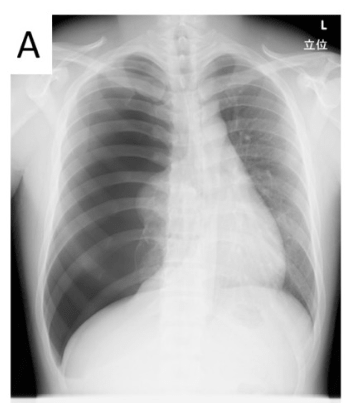
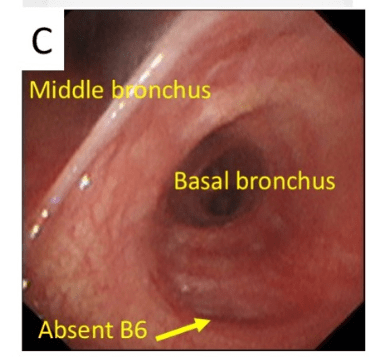
The patient was a 21-year-old man who had no remarkable medical or family history. He visited a private hospital due to sudden onset of right chest pain, cough, and dyspnea. A chest X-ray showed an almost completely collapsed right lung and mediastinal shifting to the contralateral side (Figure 1A). After chest tube drainage, the patient was referred to our hospital for further examination and surgery. Chest CT showed a hyperlucent lung area with huge bullae that were localized in the right S6 (Figure 1B). There was no B6. However, the peripheral bronchus appeared normal without mucinous impaction or bronchial dilatation. The defect of the B6, as observed by bronchoscopy (Figure 1C), was also suggestive of bronchial atresia. The S6 was almost completely isolated from the right lower lobe and was a so-called ‘posterior lobe’ [5]. Both the ventilation and perfusion scintigraphy showed a defect in the emphysematous area (Figure 1D). The patient was diagnosed with pneumothorax due to bronchial atresia in a posterior lobe.
Under general anesthesia, video-assisted excision of the right posterior lobe was performed with 4-cm window thoracotomy. Because the posterior lobe was incompletely separated from the basal segment, the posterior lobe had trapped air that was delivered from the basal segment via the incomplete accessory fissure (Figure 2A). There was no abnormality in the vascular branching of the posterior lobe. After dissecting the A6 and V6, we identified a band-like structure that seemed to be a regressed B6 (Figure 2B-D). The posterior lobe was resected with the regressed B6. The patient was discharged hospital without any complications on postoperative day 5 after the removal of the chest tube on postoperative day 2. A pathological examination revealed bullous changes in the resected posterior lobe. The regressed B6 tissue consisted of fibroblastic tissue and had no continuity with the bronchus or alveolus (Figure 2C D). At the time of writing this report, the patient is doing well without bullous reformation.






Discussion
Congenital bronchial atresia is a rare disease that was first reported by Ramsay in 1953 [1]. Obstruction at the bronchial origin causes enlargement of the peripheral bronchus, mucous accumulation, and/or emphysematous changes in the peripheral lung. The obstructed lung field traps air thorough the pores of Kohn and bronchiolar-alveolar channels of Lambert. The collateral airway works as a check valve, resulting in hyperinflation and pneumothorax in some cases.
Jederlinic reviewed 86 cases of bronchial atresia. Bronchial atresia most commonly occurs in young patients (mean age, 17 years [range, 0–44 years]) [2]. Bronchial atresia tends to occur in males more frequently than in females (64 vs 36%). Fifty percent of bronchial atresia cases occurred in the left superior lobe and 49–51% of the patients were asymptomatic at the time of evaluation [2, 3]. According to the reports of Kanzaki and Ishiwata in Japan, the etiology is almost the same as above [3, 4].
A PubMed search using the key words, ‘bronchial atresia AND pneumothorax’ revealed 7 case reports (Table 1). Chest tube drainage alone was performed in two cases, while surgical excision of the affected lung was performed in the remaining five cases (lobectomy, n=1; segmentectomy, n=4). Preservation of the lung parenchyma by segmentectomy is reasonable in cases of benign disease, particularly in the current case in which the patient had a prominent accessory fissure between the resected lung and the preserved lung. We believe that surgical therapy was also reasonable because the posterior lobe had neither perfusion nor ventilation, and because the patient had a considerable risk of death from tension pneumothorax.
|
Authors |
Age/sex |
Year |
Location |
Treatment |
Bulla |
|
Beckman et al. |
20/M |
1996 |
Left B6 |
Drainage |
Unknown |
|
Okamoto and Okubo |
25/M |
2002 |
Left superior |
Drainage |
Unknown |
|
Yoon et al. |
36/F |
2004 |
Right B2 |
Upper lobectomy |
Present |
|
Kameyama et al |
36/F |
2006 |
Left superior |
Superior segmentectomy |
Present |
|
Niimi and Gotoh |
25/F |
2010 |
Right B4 |
S4 segmentectomy |
Present |
|
Igai et al. |
18/F |
2012 |
Right B2 |
S2 segmentectomy |
Present |
|
Tanaka et al. |
26/M |
2013 |
Left superior |
Superior segmentectomy |
Present |
|
Maeda (current case) |
21/M |
2016 |
Right B6 |
S6 segmentectomy |
Present |
The pathological mechanism of the bronchial obstruction remains unknown. There are several possible theories. Bronchial atresia was caused by a disturbance in the bronchial branching during the 5th week of the fetal period when the central airways were being formed [6]. However, a normal bronchial structure is generally observed in the peripheral field of occluded bronchi, as was observed in our case. Thus, other investigators have suggested that bronchial atresia is caused after the 16th week of the fetal period, at the completion of bronchial branching. The present case showed emphysematous change without mucoid impaction in the occluded S6 area. Alveolar glands mature during weeks 20-24 of the fetal period. Furthermore, development of collateral ventilation is accomplished by 8 years of age. If bronchial atresia is caused before the sufficient development of mucous production by the alveolar glands, mucous collection is not observed: the high pressure of the occluded bronchioles prevents mucous collection [7]. Thus, in the present case, bronchial atresia might have appeared at around week 20 of the fetal period.
Summary
A superior accessory fissure that divides the lower lobe into the basal segment and superior segment, is present in approximately 5% of individuals examined by CT [8, 9]. However, the incidence of such a prominent accessory fissure as was observed in the current case may be less than 1%. This report showed that bronchial atresia in the isolated accessory lobe may induce tension pneumothorax. This should be a grave warning for physicians involved in therapeutic decision-making in similar cases.
Article Info
Article Type
Case ReportArticle History
Received: 6 December, 2018Accepted: 19 December, 2018
Published: 28 December, 2018
Copyright
© 2018 Kazuhiro Ueda. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.03.027
Author Info
Corresponding author
Kazuhiro UedaDepartment of General Thoracic Surgery, Graduate School of Medical and Dental Sciences, Kagoshima University, 8-35-1 Sakuragaoka, Kagoshima, 890-8520, Japan
Figures & Tables






|
Authors |
Age/sex |
Year |
Location |
Treatment |
Bulla |
|
Beckman et al. |
20/M |
1996 |
Left B6 |
Drainage |
Unknown |
|
Okamoto and Okubo |
25/M |
2002 |
Left superior |
Drainage |
Unknown |
|
Yoon et al. |
36/F |
2004 |
Right B2 |
Upper lobectomy |
Present |
|
Kameyama et al |
36/F |
2006 |
Left superior |
Superior segmentectomy |
Present |
|
Niimi and Gotoh |
25/F |
2010 |
Right B4 |
S4 segmentectomy |
Present |
|
Igai et al. |
18/F |
2012 |
Right B2 |
S2 segmentectomy |
Present |
|
Tanaka et al. |
26/M |
2013 |
Left superior |
Superior segmentectomy |
Present |
|
Maeda (current case) |
21/M |
2016 |
Right B6 |
S6 segmentectomy |
Present |
References
1. Ramsay BH (1953) Mucocele of the lung due to congenital obstruction of a segmental bronchus; a case report; relationship to congenital cystic disease of the lung and to congenital bronchiectasis. Dis Chest 24: 96-103. [Crossref]
2. Jederlinic PJ, Sicilian LS, Baigelman W, Gaensler EA (1987) Congenital Bronchial Atresia: A report of 4 cases and a review of the literature. Medicine (Baltimore) 66: 73-83. [Crossref]
3. Kanzaki M, Otsuka T, Yamamoto H (2000) J Jpn Soc Respir Endoscopy 22: 534-537.
4. Ishiwata T, Suda A, Abe M, Shimizu A (2014) J Jpn Soc Respir Endoscopy 36: 197-202.
5. Mawatari T, Murakami G, Koshino T, Morishita K, Abe T (2000) Posterior pulmonary lobe: segmental and vascular anatomy in human specimens. Clin Anat 13: 257-262. [Crossref]
6. Lacquet LK, Fornhoff M, Dierickx R, Buyssens N (1971) Bronchial atresia with corresponding segmental pulmonary emphysema. Thorax 26: 68-73. [Crossref]
7. Takumi Ichihashi, Tetsuo Sakai (1998) Four Cases of Bronchial Atresia. J Jpn Soc Respir Endoscopy 20: 472-480.
8. Godwin JD, Tarver RD (1985) Accessory fissures of the lung. AJR Am J Roentgenol 144: 39-47. [Crossref]
9. Yildiz A, Gölpinar F, Calikoğlu M, Duce MN, Ozer C, et al. (2004) HRCT evaluation of the accessory fissures of the lung. Eur J Radiol 49: 245-249. [Crossref]
