Can a Pain Neuroscience Education Lecture Alter Treatment Choices for Chronic Pain in Physician Assistant Students?
A B S T R A C T
Purpose: Pilot study assessing if pain neuroscience education (PNE) can shift treatment choices for patients with chronic pain in Physician Assistants (PA) students.
Methods: A convenience sample of PA students (n = 29) attended a 2-hour PNE lecture. Prior to and immediately after the lecture, students completed a questionnaire regarding their beliefs and choices regarding treatments and professionals best suited for patients suffering from chronic pain.
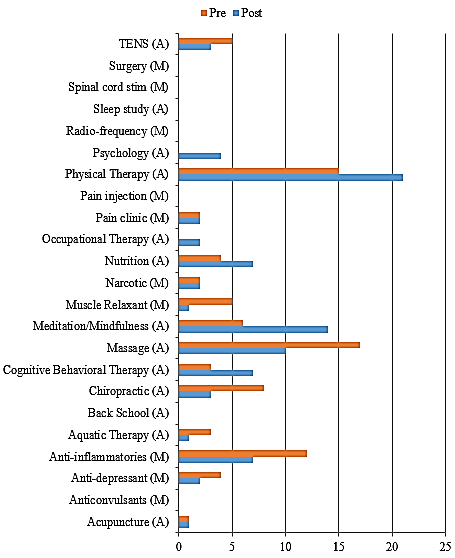
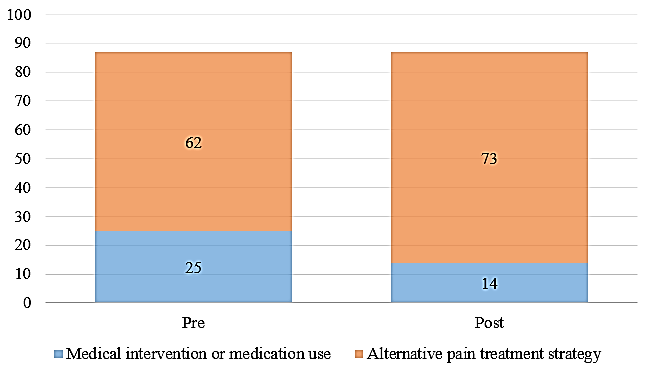
Results: Following the PNE lecture, there was a significant shift of decreasing the choice of medical interventions/pharmaceutical use and increasing alternative pain strategy interventions (p = 0.046). Further, non-pharmaceutical treatments shifted towards cognitive and active movement approaches (mindfulness, relaxation, physical therapy, psychology and cognitive behavioural medicine), away from passive treatments (massage therapy and chiropractic). After PNE, PA students were less likely to recommend an orthopedic surgeon to treat chronic pain (p = 0.015).
Conclusion: A PNE lecture to PA students is able to decrease pharmaceuticals as first choice in treatment of chronic pain and towards more active, non-pharmaceutical cognitive targeted treatments.
Keywords
Pain, neuroscience, education, physician assistant, chronic
Introduction
Rates of chronic pain and the resultant opioid use to address chronic pain is at epidemic proportions. In the United States (US) an estimated 126.1 million adults experience pain over a 3-month period, with 25.3 million suffering from daily chronic pain [1]. Americans, 5% of the world's population, consume 80% of the opioids, and 99% of the hydrocodone globally [2]. In lieu of these staggering epidemic numbers, the question arises - what can be done to address these issues? The answer is multifactorial and no one single answer will change this trajectory. One of those answers may be related to how we as society, and more specifically healthcare providers, view pain.
Historically pain has been tied to the health of a person’s tissues: Injury and disease significance are associated with pain levels and vice versa, pain levels are associated with amount of injury or diseased tissues. This model, known as the biomedical model, would then assume treatment for pain be directed at the affected tissues [3]. By reducing acute inflammation and allowing healing (i.e., ankle sprain), pain will ease. Pain, especially chronic pain, is far more complex. It is now well established that complex biological processes such as central sensitization, functional and structural changes in the brain; inhibition and facilitation via central pathways of the central nervous system, etc., all play a significant role in pain [3]. Furthermore, it has been shown that many people in pain present with healthy tissues on imaging and medical tests and conversely many healthy, pain-free people demonstrate age changes (disc degeneration), various anomalies (stenosis, spurs, etc.) on imaging. A modern view of pain has led to a biopsychosocial approach to pain management in medicine, which aims to explore a deeper biological, physiological, and social understanding of the pain experience [3]. One clinical application of this model is referred to as pain neuroscience education (PNE), whereby this knowledge of pain is shared with patients to help them reconceptualize their pain. Strong evidence exists for PNE to positively influence pain ratings, dysfunction, fear-avoidance behaviour, pain catastrophization, movement dysfunction, pain knowledge, and healthcare utilization [4, 5].
Even though there are various opinions on what it will take to curb the pain and opioid epidemic, it is generally agreed upon that interventions must begin earlier as the proverbial “upstream” approach [6]. To truly affect the current state of affairs, providers at the initial contact must shift from the mindset that pain should be treated exclusively by means of pharmacological interventions, especially narcotics [6]. Current US data shows that much of the opioid epidemic from the medical side can be traced to early contact points, i.e., emergency departments and urgent care [6]. Within this model alongside the growth of the physician assistant (PA) programs in the US, it is argued that PA’s must be a primary target for this new approach [7]. In a recent PNE PA study it was shown than PA students after a 1 or 2-hour lecture of PNE not only increased their knowledge of pain but was able to positively change their attitudes and beliefs regarding pain, especially chronic pain [7]. This follow-up study aimed to determine if a 2-hour PNE lecture to PA students could change their thoughts about treatment options for people in pain, without explicitly addressing treatment and only focusing on the neurobiology and neurophysiology of pain.
Methods
I Participants and Procedure
Participants consisted of a convenience sample of PA students in a 24-month Master’s program - 2nd semester of their 1st year. The PNE lecture was a part of their neuro unit to provide education on the neuro-pathophysiology of pain mechanisms. The program is accredited through the Accreditation Review Commission on Education for Physician Assistants. Institutional review board (IRB) approval was obtained at St. Ambrose University for the study.
II Educational Protocol
The content of the lecture has been used in a previous PNE PA study described elsewhere [7]. In short, the PA lecture was a 2-hour lecture using PowerPoint™ to teach PA students about the neurophysiology and neurobiology of pain. The lecture covered content regarding challenges with current biomedical approaches to treating chronic pain and updated neuroscience of pain information (ion channels, nociceptive input, dorsal horn wind-up, neuronal facilitation/inhibition, pain matrix, environmental and stress effects on pain perception) [3, 7]. The content focused on pain neuroscience and did not cover any content specific to the pre- and post-education questionnaire. The 2-hour lecture was chosen due to its ability to positively change pain knowledge, attitudes and beliefs regarding pain and fit into class schedules [7]. The lecture was delivered by one of the authors (AL), who has taught PNE in both graduate and post-graduate level for 20 years.
III Instrument
A questionnaire was developed in order to address the aims of the study. The questionnaire consisted of three parts. Part one focused on demographics including age, gender, personal and family experiences with pain as well as their own comfort with treating chronic pain. Part two focused on their beliefs in terms of which healthcare providers were ideal to assess and treat chronic pain (Likert scale anchored at 0 [not recommended] and 10 [highly recommended]). Part three focused on various current treatments offered in pain management for chronic pain, asking PA students to identify top three preferred treatments. To assess face and content validity, the original questionnaire was sent to an expert panel (n = 12) consisting of experts in PNE, PA education and questionnaire design. Per questionnaire design protocols, if a 70% agreement was obtained, the questionnaire was deemed ready for the next step. Step one revealed a few grammar issues and small clarifications on questions, which was addresses to develop a version 2. The questionnaire was then provided to a convenience sample of 5 students to measure the time they took to complete the instrument and feedback. Upon review, no suggestions for change were given, deeming the questionnaire ready for the study.
IV Procedure
The study design was a pre- and post- single cohort measurement. One week prior to the PNE presentation, PA students were given a link to complete an online (PsychData, State College, PA, USA) questionnaire. Students then attended the in-person lecture provided at the University as part of their course work. Afterward, they were invited to again complete the post-lecture questionnaire through the on-line PsychData link.
V Statistical Analysis
The survey data were extracted from PsychData and downloaded into an Excel file and data was analysed utilizing SPSS (version 24.0, IBM Corporation). Pre and post groups were analysed as independent samples, as no linking variable was used in data collection between pre and post measurements. Descriptive statistics of means, standard deviations, ranges, and percentages were reported for participant characteristics. Frequencies of top three treatment interventions were calculated. These interventions were categorical coded as medical intervention/medication use or alternative pain strategy intervention. Chi square test of goodness-to-fit was used to determine if categorical intervention strategy was equally preferred pre and post educational experience. Assessment of the effects of the educational experience on individual comfort level to treat patients with chronic pain patients and confidence level with various health care providers in care for patients with chronic pain was calculated with Mann-Whitney U-test for individual samples.
Results
I Participants
Table 1 provide demographic information on participants. Thirty-one participants (age range 22-30) underwent the PNE session. Two participant data sets were incomplete from both pre-educational experience and post-educational experience. They were excluded from final data analysis, leaving 29 participants in both pre and post educational experience for analysis.
Table 1: Participant demographics.
|
Characteristics |
n=29 |
|
Age, mean (SD), years |
23.86 (1.64) |
|
Gender, n (%) Female Male |
28 (97) 1 (3) |
|
Currently experiencing pain, n (%) Yes No |
2 (7) 27 (93) |
|
Pain within the last 6 months, n (%) Yes No |
9 (31) 20 (69) |
|
Family member with chronic pain, n (%) Yes No |
15 (52) 14 (48) |
II Healthcare Providers Providing Pain Management
Following the training the PA students showed an increase on the Likert scale regarding their confidence treating patients with chronic pain from 3.66 (±2.32) to 4.66 (±2.09), but this did not reach statistical significance, U = 541.5, z = 1.90, p = 0.057. The confidence level of other professionals treating individuals with chronic pain can be seen in (Table 2). The only significant shift in confidence was a decrease in confidence in orthopedic surgeons (p=0.015).
III Preferred Pain Interventions
The PA student selection of their top three treatment interventions for individuals with chronic pain can be seen in (Figure 1). Chi square test of goodness-of-fit showed that there was a significant shift of decreasing their choice of medical interventions/medication use and increasing alternative pain strategy interventions post the educational experience, Χ2 (1, N = 174) = 4.00, p = 0.046. There was a net change of 11 options from the medical intervention/medication use to the alternative pain strategy interventions, representing a reduction of 44% (Figure 2).
Table 2: Confidence in professional treating a person with chronic pain (0 [not recommended] and 10 [highly recommended]) - ranked post-education from highest to lowest.
|
Professional treating |
Pre (n=29) |
Post (n=29) |
p-value |
|
Family Medicine Physician |
7.24 (2.05) |
7.07 (2.12) |
.559 |
|
Orthopedic Surgeon |
7.59 (2.46) |
5.89 (2.67) |
.015 |
|
Psychologist |
7.76 (1.3) |
7.66 (2.09) |
.962 |
|
Physical therapist |
7.24 (1.5) |
8.00 (1.69) |
.600 |
|
Occupational therapist |
7.43 (1.9) |
7.52 (2.20) |
.734 |
|
Nurse practitioner |
7.10 (2.02) |
7.14 (2.10) |
.975 |
|
Chiropractor |
6.59 (2.06) |
6.31 (2.42) |
.666 |
|
Physician assistant |
7.86 (1.85) |
7.62 (2.13) |
.787 |
|
Pain Management Specialist |
9.32 (1.12) |
8.62 (1.70) |
.095 |
|
Massage Therapist |
6.17 (2.14) |
7.00 (2.82) |
.099 |
Figure 1: Top three choices of pain intervention for individuals with chronic pain.
M: Medical intervention/Medication use; A: Alternative pain treatment strategy; TENS: Transcutaneous Electrical Nerve Stimulation.
Figure 2: Totals for top three choices for pain treatment categorically as medical intervention/medication use or alternative pain treatment strategy.
Discussion
A 2-hour PNE lecture to PA students is able to decrease pharmaceuticals as first choice in treatment of chronic pain and shift towards more active, non-pharmaceutical cognitive targeted treatments.
Even though this study represents a small, convenience sample of PA students, the results are a potential first step towards changing medical prescription habits from a pharmaceutical first mindset to more preferred clinical practice guidelines of active, non-pharmaceutical treatments first. Current best-evidence systematic reviews and meta-analyses for various chronic pain conditions center around three common treatments: education (alter cognitions), movement and mechanisms to calm the central nervous system (i.e., ant-depressants and/or membrane stabilizers) [8]. Non-pharmacological ways of calming the nervous system, including mindfulness, relaxation, cognitive behavioural therapy and exercise, are showing increased evidence, and a potential choice over pharmaceuticals [9]. In this study, the student’s exposure to the updated biological and physiological understanding of pain facilitated a positive shift. Even though narcotics choices did not shift, it’s important to note that the various medication choices affected by this lecture are also associated with significant risk, especially taken over extended periods, which is associated with chronic pain [6].
In regard to the various non-pharmacological treatments, the results also show a shift away from passive interventions (massage therapy, chiropractic, TENS) towards more active treatment (physical therapy) and more importantly various psychological interventions (mindfulness, relaxation, and cognitive behavioural therapy). This result is encouraging as it is in line with current evidence suggesting more active treatments (internal locus of control) and a realization that pain and cognitions are powerfully interconnected and need a broader, biopsychosocial approach versus the traditional biomedical approach [10]. The only professional choice significantly altered was orthopedic surgery, which concurs with the treatment choices moving from pharmacological/interventional to more conservative, non-pharmacological and non-interventional treatments. This result further showcases the ability of PNE to shift PA students away from a biomedically focused model of ‘fixing’ tissue issues (surgery) to help people with chronic pain.
This study contains various limitations including small, convenience sample size; only immediate post-education results with no follow-up; no control groups and potential bias towards physical therapy since the lecture was delivered by a physical therapist. This study, however, showcases that a lecture on pain biology and physiology (PNE) is able to shift PA students to treatment choices more in line with current best-evidence for chronic pain. Larger studies with longer follow-up and included controls are needed to validate these findings.
Conflicts of Interest
None.
Internal Review Board
This study was approved by St. Ambrose University, Institutional Review Board, Davenport, IA.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 27, Jul 2020Accepted: Thu 06, Aug 2020
Published: Fri 14, Aug 2020
Copyright
© 2023 Nicholas Maiers. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.PDR.2020.02.03
Author Info
Adriaan Louw Angela Schmieder Elizabeth Peppin Kevin Farrell Kory Zimney Nicholas Maiers
Corresponding Author
Nicholas MaiersPhysical Therapy Department, Des Moines University, Iowa, USA
Figures & Tables
Table 1: Participant demographics.
|
Characteristics |
n=29 |
|
Age, mean (SD), years |
23.86 (1.64) |
|
Gender, n (%) Female Male |
28 (97) 1 (3) |
|
Currently experiencing pain, n (%) Yes No |
2 (7) 27 (93) |
|
Pain within the last 6 months, n (%) Yes No |
9 (31) 20 (69) |
|
Family member with chronic pain, n (%) Yes No |
15 (52) 14 (48) |
Table 2: Confidence in professional treating a person with chronic pain (0 [not recommended] and 10 [highly recommended]) - ranked post-education from highest to lowest.
|
Professional treating |
Pre (n=29) |
Post (n=29) |
p-value |
|
Family Medicine Physician |
7.24 (2.05) |
7.07 (2.12) |
.559 |
|
Orthopedic Surgeon |
7.59 (2.46) |
5.89 (2.67) |
.015 |
|
Psychologist |
7.76 (1.3) |
7.66 (2.09) |
.962 |
|
Physical therapist |
7.24 (1.5) |
8.00 (1.69) |
.600 |
|
Occupational therapist |
7.43 (1.9) |
7.52 (2.20) |
.734 |
|
Nurse practitioner |
7.10 (2.02) |
7.14 (2.10) |
.975 |
|
Chiropractor |
6.59 (2.06) |
6.31 (2.42) |
.666 |
|
Physician assistant |
7.86 (1.85) |
7.62 (2.13) |
.787 |
|
Pain Management Specialist |
9.32 (1.12) |
8.62 (1.70) |
.095 |
|
Massage Therapist |
6.17 (2.14) |
7.00 (2.82) |
.099 |
M: Medical intervention/Medication use; A: Alternative pain treatment strategy; TENS: Transcutaneous Electrical Nerve Stimulation.
References
- IOM, Institute of Medicine (2011) Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research. Washington DC: National Acad Press. [Crossref]
- Manchikanti L, Fellows B, Ailinani H, Pampati V (2010) Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician 13: 401-435. [Crossref]
- Moseley GL (2007) Reconceptualising pain acording to modern pain science. Physical Ther Rev 12: 169-178.
- Louw A, Zimney K, Puentedura EJ, Diener I (2016) The Efficacy of Therapeutic Neuroscience Education on Musculoskeletal Pain – A Systematic Review of the Literature. Physiother Theory Pract 32: 332-355. [Crossref]
- Malfliet A, Kregel J, Coppieters I, Pauw RD, Meeus M et al. (2018) Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA Neurol 75: 808-817. [Crossref]
- Zheng P, Kao M, Karayannis NV, Smuck M (2017) Stagnant Physical Therapy Referral Rates Alongside Rising Opioid Prescription Rates in Patients With Low Back Pain in the United States 1997-2010. Spine (Phila Pa 1976) 42: 670-674. [Crossref]
- Zimney K, Louw A, Johnson J, Peppers S, Farrell K (2018) Effects of Pain Neuroscience Education on Physician Assistant Students Understanding of Pain and Attitudes and Beliefs About Pain. S D Med 71: 506-511. [Crossref]
- Carville SF, Arendt Nielsen L, Bliddal H, Blotman F, Branco JC et al. (2008) EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis 67: 536-541. [Crossref]
- Bernardy K, Klose P, Busch AJ, Choy EH, Hauser W (2013) Cognitive behavioural therapies for fibromyalgia. Cochrane Data Syst Rev 9: CD009796. [Crossref]
- Brosseau L, Wells GA, Tugwell P, Egan M, Wilson KG et al. (2008) Ottawa Panel Evidence-Based Clinical Practice Guidelines for Aerobic Fitness Exercises in the Management of Fibromyalgia: Part 1. Phys Ther 88: 857-871. [Crossref]
