Case of Invasive Metastatic Breast Cancer Mimicking Crohn’s Disease
A B S T R A C T
Background: A female patient with a history of stage IIB invasive lobular breast cancer presented with symptoms of partial small bowel obstruction and workup led to a presumptive diagnosis of Crohn’s disease. However, at the time of surgical intervention, she was found to have metastatic lobular breast cancer with carcinomatosis and metastases to the small and large intestines.
Summary: Our patient presented at age 55 with intermittent nausea and vomiting, dyspepsia, altered bowel habits, and weight loss. She had a history of invasive lobular carcinoma of the right breast treated with right modified radical mastectomy followed by adjuvant chemoradiation and hormonal therapy 5 years earlier. She was thought to be in remission. Initial workup of her GI complaints was notable for thickening of the sigmoid colon and hepatic flexure on CT scan and stricturing and colitis in these areas on colonoscopy. Mucosal biopsies showed nonspecific active colitis. The patient was treated for a presumptive diagnosis of Crohn’s disease without significant improvement. She was eventually taken for surgery after presenting with a high-grade small bowel obstruction. On exploration, numerous additional small and large bowel strictures, some associated with intraluminal masses, were found and a small bowel resection and ileostomy performed. Pathology revealed metastatic invasive lobular breast carcinoma. Although isolated metastases to the bowel wall are rare, they have been reported secondary to a wide range of malignancies. Breast cancer, especially lobular carcinoma, is one of the most common tumors to metastasize to the GI tract and can present years after the primary cancer diagnosis. Therefore, the differential diagnosis for a patient with signs and symptoms of bowel obstruction and a history of lobular breast cancer should include metastatic disease.
Conclusion: Metastatic cancer to the GI tract can mimic Crohn’s disease and should be on the differential in older patients with abdominal complaints, particularly those with a history of breast cancer.
Keywords
Crohn’s disease, breast cancer, gastrointestinal metastases
Case Description
We report a rare presentation of metastatic lobular carcinoma to the small and large intestines mimicking Crohn’s disease five years after initial diagnosis of breast cancer. The patient is a 55 years-old female with intermittent nausea, vomiting, dyspepsia, intolerance of solid foods, altered bowel patterns and a 30-pound weight loss. She had a history of Stage IIB T2N1MO ER/PR positive, Her-2/neu positive invasive lobular carcinoma of the right breast diagnosed 5 years earlier. At that time, she underwent right modified radical mastectomy and left breast excisional biopsy followed by adjuvant chemoradiation and 5 years of hormonal therapy. She was thought to be in remission. She was initially seen at an outside facility for workup of her GI complaints. There, a CT scan showed thickening in the sigmoid colon and hepatic flexure with stricturing and nonpathologic mesenteric adenopathy. On colonoscopy, she was found to have moderate inflammation with congestion, edema, erythema and erosions in the sigmoid and transverse colon. Biopsies showed nonspecific active colitis with acute cryptitis and rare crypt abscesses. No granulomas, dysplasia, or malignancy was seen. A definitive diagnosis could not be made, however Crohn’s disease was presumed based on the clinical and imaging characteristics.
Figure 1: Sigmoid Stricture encountered during colonoscopy
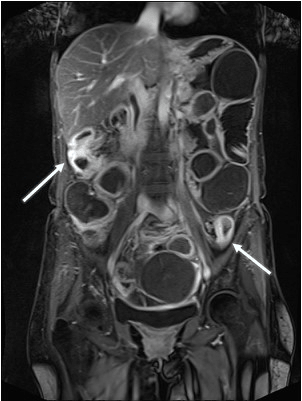
Figure 2: Intestinal strictures on magnetic resonance enterography.
Treatment was initiated with budesonide and balsalazide without any obvious improvement. Follow-up sigmoidoscopy and CT scan showed unchanged findings. Upper endoscopy was also nondiagnostic. Because the patient continued to have chronic obstructive symptoms, colonoscopy was repeated several months later and notable for rapid progression to severe stenosis in the sigmoid colon (Figure 1). Biopsies were again notable for focal cryptitis without evidence of malignancy. Follow-up MR enterography (Figure 2) revealed markedly dilated small bowel with a transition point to decompressed bowel at an area of thickening and hyperenhancement in the mid to distal ileum as well as discontinuous segments of colon. No masses were found on abdominal imaging, including in the liver.
Although surgical intervention was felt to be ultimately necessary, there was concern for extensive bowel resection and ensuing short bowel syndrome due to the large disease burden seen on imaging. Therefore, the decision was made to treat the patient with a loading regimen of infliximab, bowel rest and TPN in an effort to decrease inflammation prior to surgery. Despite this, the patient represented to the emergency department with a high-grade small bowel obstruction with possible closed-loop obstruction and was taken for urgent abdominal exploration. Intraoperatively, she was found to have numerous additional strictures of her small and large bowel, some associated with intraluminal masses. Her colon and mesentery were diffusely thickened, firm and hypopigmented. An area of small bowel with multiple strictures was resected. Frozen pathologic evaluation of this specimen was suspicious for malignancy, so a diverting ileostomy was brought up without further resection. Final pathology was positive for metastatic invasive lobular breast carcinoma. Postoperatively, the patient was treated by her original medical oncologist. She experienced disease and symptom progression despite trials of Ibrance, Anastrazole, Herceptin and palliative radiation. Ultimately, she decided to pursue home hospice and later passed.
Discussion
Breast cancer is the most common malignancy in females worldwide and is the second leading cause of cancer-related death in the United States [1]. Isolated metastases to the bowel wall are rare but have been reported secondary to a wide range of malignancies, including breast cancer [2-12]. In fact, after melanoma, breast cancer is the second most common metastasis to the GI tract [2]. Lobular carcinoma is the most likely to metastasize to the GI tract, despite representing only a minority of breast cancers [8]. Cases of GI metastases from lobular breast cancer in particular, have been reported to occur even several years after the primary cancer diagnosis [8, 10].
Symptoms from bowel wall metastases can mimic small and/or large intestinal Crohn’s disease in presentation and on imaging [3-8]. Metastases can occur along the entire length of the GI tract [8]. As a result, presenting symptoms of bleeding, obstruction, or perforation can mimic a range of other diseases, including peptic ulcer disease, gastritis, Crohn's disease, and gastric linitis plastica [8, 12, 13]. Pathologic appearance varies but tends to be either focal and nodular (most common in solid organs) or diffuse (most common in the retroperitoneum, peritoneum and in hollow viscera) in nature [13]. Imaging of GI metastases of lobular breast cancer may show diffuse small and large bowel stenosis, infiltrative linitis plastica, and/or multiple lesions with contours consistent with submucosal or serosal masses.
With continued advances in breast cancer therapies leading to improved survival, clinicians are likely to see diverse presentations of metastatic disease. Histologic examination is necessary for diagnosis, however endoscopic biopsies are often low yield due to the submucosal nature of the cancer [6-8]. As a result, it is important to maintain a high level of suspicion for metastasis in patients with prior history of lobular breast cancer presenting with symptoms mimicking GI diseases, especially those who are not responding to traditional therapy.
Conclusion
Breast cancer, especially lobular carcinoma, can metastasize to the GI tract and mimic diseases, such as Crohn’s disease. We present a case of metastatic lobular breast cancer mimicking Crohn’s disease that occurred 5 years after initial cancer diagnosis and treatment.
Lessons learned
Metastatic lobular breast cancer to the GI tract can present years after initial cancer diagnosis. Diagnosis can be difficult given this delayed presentation, the often nonspecific signs and symptoms leading to a broad differential, and the submucosal nature of the bowel metastases, which can result in misleading endoscopic biopsies.
Conflicts of interest
The authors have no conflicts of interest to report.
Article Info
Article Type
Case ReportPublication history
Received: Wed 06, Nov 2019Accepted: Sat 23, Nov 2019
Published: Mon 30, Dec 2019
Copyright
© 2023 Bryce E. Haac. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2019.01.04
Author Info
Jonah N. Rubin Andrea Chao Bafford Bryce E. Haac Fikru Merechi Kaci Christian Raymond K. Cross Seema A. Patil Uni Wong
Corresponding Author
Bryce E. HaacDepartment of Surgery, University of Maryland Medical Center, Baltimore, MD 21201, USA
Figures & Tables

References
- Cancer Facts and Figures (2016) American Cancer Society.
- Ng CE, Wright L, Pieri A, Belhasan A, Tarannum F (2015) Rectal metastasis from Breast cancer: A rare entity. Int J Surg Case Rep 13: 103-105. [Crossref]
- Meyers MA, Oliphant M, Teixidor H, Weiser P (1975) Metastatic carcinoma simulating inflammatory colitis. Am J Roentgenol Radium Ther Nucl Med 123: 74-83. [Crossref]
- Katon RM, Brendler SJ, Ireland K (1989) Gastric linitis plastic with metastases to the colon: a mimic of Crohn’s disease. J Clin Gastroenterol 11: 555-560. [Crossref]
- Tanakaya K, Takeuchi H, Yasui Y, Takeda A, Umeda Y et al. (2004) Metastatic carcinoma of the colon similar to Crohn’s disease: a case report. Acta Med Okayama 58: 217-220. [Crossref]
- Madeya S, Borsch G (1989) [Differential diagnosis of Crohn disease: segmental intestinal metastasis of breast and stomach cancer]. Leber Magen Darm 19: 140, 143-146, 149-152. [Crossref]
- Zenda T, Taniguchi K, Hashimoto T, Takeshita Y, Choto S et al. (2007) Metastatic colon cancer mimicking Crohn’s disease. Ann Diagn Pathol 11: 427-432. [Crossref]
- Nazareno K, Taves D, Preiksaitis H (2006) Metastatic breast cancer to the gastrointestinal tract: a case series and review of the literature. World J Gastroenterol 12: 6219-6224. [Crossref]
- Balthazar EJ, Rosenberg HD, Davidian MM (1979) Primary and metastatic scirrhous carcinoma of the rectum. AJR Am J Roentgenol 132: 711-715. [Crossref]
- Jang HJ, Lim HK, Kim HS, Cho EY, Lee SJ et al. (2001) Intestinal metastases from gastric adenocarcinoma: helical CT findings. J Comput Assist Tomogr 25: 61-67. [Crossref]
- Critchley AC, Harvey J, Carr M, Iwuchukwu (2011) Synchronous gastric and colonic metastases of invasive lobular breast carcinoma: case report and review of the literature. Ann R Coll Surg Engl 93: e49-e50. [Crossref]
- DiPiro PJ, Tirumani SH, Cruz GP, Ramaiya NH, Lester SC et al. (2019) Lobular breast cancer: patterns of intraabdominal metastatic spread on imaging and prognostic significance. Abdom Radiol (NY) 44: 362-369. [Crossref]
- Kidney DD, Cohen AJ, Butler J (1997) Abdominal metastases of infiltrating lobular breast carcinoma: CT and fluoroscopic imaging findings. Abdom Imaging 22: 156-159. [Crossref]
