Case Reports of Acquired and Reversible Tracheomegaly
A B S T R A C T
Dilation of the trachea, or tracheomegaly, is a rare phenomenon that can occur under a variety of disease processes and categorized into either congenital or acquired. In acquired cases, causes range from excessive tracheal wall pressure from prolonged intubation and cuff hyperinflation to inflammatory respiratory pathologies such as chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, and cystic fibrosis. However, due to the low number of reported cases, the nature of these acquired processes is unclear. We present two cases that developed tracheomegaly of unknown etiology, one of which was reversible. Patients with factors predisposing them to tracheomalacia during intubation can experience significant air leaks with difficulty ventilating the patient and that could represent increasing tracheomegaly. Changing the cuff location intermittently during prolonged intubations may prevent tracheomegaly from occurring or may diminish its’ extent once it does occur. To the best of our knowledge, the reversibility of this relatively rare disorder has not been previously reported.
Keywords
Tracheomegaly, tracheomalacia, tracheal injury, prolonged intubation, case report
Introduction
Abnormal dilation of the trachea, or tracheomegaly, can occur under a variety of disease processes and further categorized into either congenital or acquired. This rare phenomenon, characterized by a sagittal diameter greater than 27 mm in men and 23 mm in women, is thought to result from any condition that weakens the cartilage, or tracheomalacia [1]. According to case reports, congenital etiologies include connective tissue disorders such as Ehlers-Danlos and Marfan syndrome, and idiopathic tracheobronchomegaly or Mounier-Kuhn syndrome [2, 3]. In acquired cases, potential causes range from excessive force to the cartilage as seen in prolonged intubation and cuff hyperinflation to inflammatory respiratory conditions such as chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, and cystic fibrosis [2, 4, 5]. However, due to their low case counts, the dynamic nature of the acquired process is unclear.
We present two unique cases in which patients admitted to our otolaryngology service at a tertiary care center developed tracheomegaly of unknown etiology, one of which was reversible. To the best of our knowledge, the reversibility of this relatively rare disorder has not been previously documented nor reported. This paper has been reported in line with the SCARE and PROCESS criteria [6, 7].
Methods
I Retrospective Review
After obtaining (blinded for review) institutional review board approval, a retrospective review of patients diagnosed with tracheomegaly at a single, academic institution was undertaken. Two cases were identified.
II Case Descriptions
Case 1
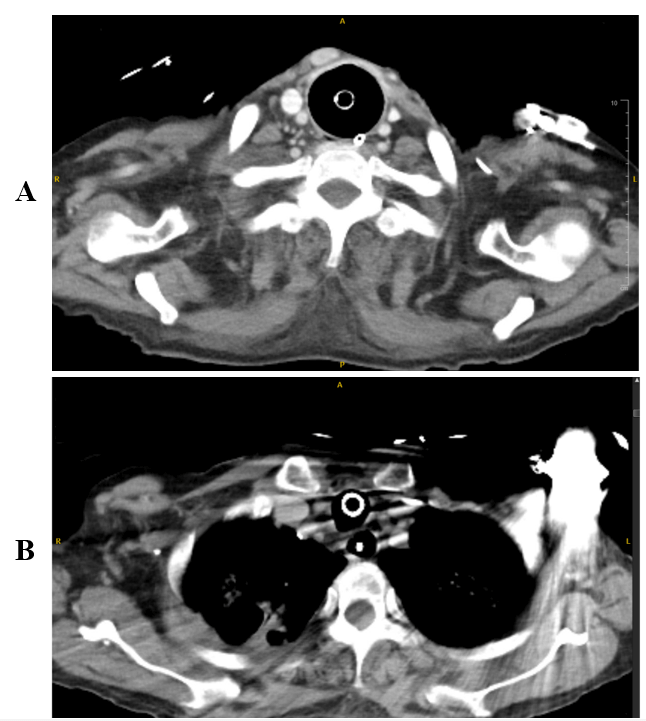
A 61-year-old female with a history of hypertension, implantable defibrillator, and alcohol and tobacco use disorder presented to our tertiary care center with second and third degree burns circumferentially to the neck, face, and scalp after catching her hair on fire. The patient was intubated upon arrival due to inhalation injury with a 7.5 mm endotracheal tube (ETT). After admission to the burn unit, the ETT was ultimately upsized to an 8.5 mm tube after several episodes of desaturation. These episodes were triggered by positioning changes and suspected cuff leak or tube displacement. The patient required a positive end-expiratory pressure (PEEP) of 8-10 cmH2O for 13 days and during that time had peak airway pressures up to 41 mmHg. Primary service stated that the cuff was initially inflated to the appropriate amount of pressure but needed to be progressively overinflated due to worsening cuff leak. The patient’s course was further complicated by necrotizing pneumonia with concern for spread to the trachea. A computed tomography (CT) chest with intravenous (IV) contrast noted a focal 4.1 cm dilatation near the expected location of the ETT cuff in the mid-thoracic trachea (Figure 1A).
Figure 1: A) CT neck of patient #1 showing tracheomegaly after intubation. B) Now 2 months after tracheostomy and off ventilator. CT chest showing return to normal diameter of trachea.
The patient underwent direct microlaryngoscopy and bronchoscopy after 3 weeks of intubation. At the level of the cuff, the trachea was significantly dilated with no signs of necrotizing disease. The distal trachea down to the level of the carina and mainstem bronchi had a normal diameter. The ETT was repositioned to have the cuff located below this level of dilation. Intraoperatively, given the wide caliber of dilation, there was concern for a possible congenital etiology.
At 6 weeks of admission, the ETT was exchanged for an 8.0 mm tracheostomy tube. Bronchoscopy showed that the dilated section of trachea had reduced to 2.3 cm in diameter (Figure 1B). A workup for congenital etiologies of the tracheomegaly was negative.
Case 2
A 58-year-old Hispanic male with a history of COPD, hypertension, and diabetes was initially transferred to our tertiary care center from an outside hospital for surgical evaluation of a sub-centimeter intrathoracic tracheal diverticulum and potential lung transplant. A year prior, he was hospitalized for a severe Covid-19 infection that was complicated by respiratory failure, long-term mechanical intubation requiring tracheostomy, and extensive pulmonary fibrosis. It was unknown how long the patient had been intubated, though he was decannulated within the past 4 months. However, during this period he experienced a cardiac arrest secondary to a myocardial infarction and required a second tracheostomy. Since then, he suffered recurrent episodes of respiratory decompensation.
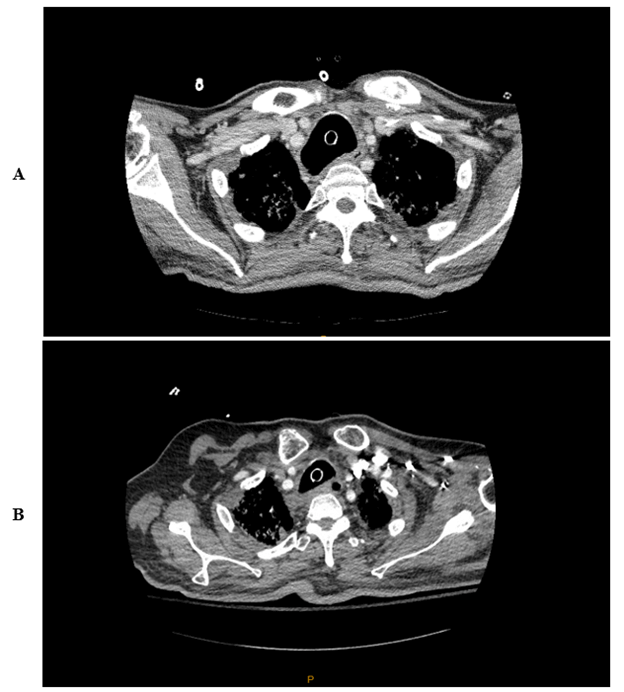
A few days after the patient’s transfer, his tracheostomy tube dislodged and required endotracheal intubation. On radiographic review, tracheobronchomegaly was appreciated in addition to his known tracheal diverticulum and pulmonary fibrosis (Figure 2A). It was noted that the tracheobronchomegaly was not present in a CT chest one month prior (Figure 2B). Due to this patient’s complex airway, the otolaryngology service was consulted. The patient was consented for and underwent direct laryngoscopy and tracheostomy revision. The ETT tube was easily exchanged for a 6.0 mm tracheostomy tube.
Figure 2: A) Patient #2 status post 2nd tracheostomy and on ventilator. B) CT showing normal tracheal diameter 8 months prior to hospital admission.
Discussion
The differential diagnosis of tracheal dilation remains broad, though we believe the extent of tracheomegaly documented in these cases resulted from more than ETT cuff overinflation. The most common acquired causes are prolonged tracheostomy or intubation. Pressure from the cuff against the tracheal wall leads to impaired blood flow micronecrosis, and eventually gradual cartilage destruction [8]. In patients with a history of tobacco use, evidence of decreased airway integrity from cigarette smoke has been identified in about 23% of those with COPD [4]. Generally speaking, a 7.0 or 7.5 mm ETT is appropriate for the average female with an outer diameter of 8.6 and 10.2 mm, and an 8.0 or 8.5 mm ETT for the average male with an outer diameter of 11.0 and 11.6 mm, respectively. Even after maximal cuff inflation, the widest diameter would still be less than 3 cm. Thus, it seemed possible at the time of initial evaluation that there were other contributing etiologies other than overinflation of the cuff.
For patient #1, we explored possible contributing etiologies such as Ehlers Danlos and Marfan syndrome that can cause an intrinsically weak trachea [2]. Although her height of 1.8 m could suggest an underlying connective tissue disease, she did not have classically associated valvular abnormalities seen on a transthoracic echocardiogram. Even more rare would be Mounier-Kuhn syndrome, characterized by atrophy of longitudinal elastic fibers and thinning of the muscularis mucosa which causes dilation of the trachea and central bronchi [3]. Ultimately, given that the area of dilation improved after removal of the cuff and there were no other obvious characteristics, it seemed unlikely that there was an underlying congenital condition.
Other risk factors for tracheomegaly include a history of obesity, diabetes, poor nutritional status, smoking, and poor overall health–all but one of which patient #2 had. In addition, pulmonary conditions such as COPD, pulmonary fibrosis, cystic fibrosis, and bronchiectasis have been associated with tracheomegaly [4, 5]. Given patient #2’s history of Covid-19 infection with prolonged intubation and tracheostomy along with his underlying COPD, diabetes, and pulmonary fibrosis, he may have been predisposed to tracheal wall weakening.
The literature commonly describes the development of laryngotracheal stenosis following prolonged intubation in burn patients with inhalation injury [9]. Katlic et al. have discussed cases that in the presence of tracheal inhalation injury, any amount of cuff pressure may lead to tracheal damage and dilation [10]. At our institution, cuff pressures are closely monitored by respiratory therapists to avoid overinflation and subsequent tracheal dilation leading to a cuff leak. In these two patients, despite closely monitoring the cuff pressure, inhalation injury in patient #1 and long-term increased cuff pressure in patient #2 likely resulted in tracheal damage and an inherent wall weakness.
We believe that both of these patients had an increased risk of tracheomalacia predisposing them to tracheal weakness despite having “normal” cuff pressures. In patient #1, the high PEEP and peak airway pressures resulted in further dilation beyond the diameter of the cuff. The resulting air leaks and subsequent poor ventilation led to a vicious cycle of increasing cuff pressure and/or size, and further increases in PEEP. This cycle only resolved when the cuff was advanced to a novel tracheal site, allowing an improved seal on a less weakened aspect of the tracheal wall.
These cases highlight the increased risk of tracheomalacia and tracheomegaly in patients predisposed to tracheal wall weakness regardless of the cuff pressure of the ETT. Movement of the ETT cuff to a non-dilated segment seems to help resolve the area of tracheal dilation. Of great importance is the partial reversibility of this disorder. However, whether these patients are prone to recurrences of tracheomegaly if future intubations and ventilatory support are necessary is unknown.
Conclusion
Patients with factors predisposing them to tracheomalacia during intubation need to be monitored for worsening air leaks that could represent increasing tracheomegaly. Changing the cuff location intermittently during prolonged intubations may prevent tracheomegaly from occurring or may diminish its’ extent once it does occur. Clinical awareness of this entity is warranted especially because of the more commonplace prolonged intubations during the Covid-19 pandemic. Future studies incorporating larger number of patients are needed to more definitively define the appropriate management of patients with this disease process.
Author Contributions
SY and SC collected data for case 1. AS conducted the literature search. SA collected data for case 2. All authors wrote and reviewed the final manuscript.
Location of Study
Loyola University Medical Center.
Prior Meetings or Forums
None.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 09, Nov 2022Accepted: Wed 30, Nov 2022
Published: Sat 17, Dec 2022
Copyright
© 2023 Alice Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2022.03.01
Author Info
Alice Su Sara Yang Shaley Albaugh Steven J. Charous
Corresponding Author
Alice SuLoyola University Chicago Stritch School of Medicine, Maywood, Illinois, USA
Figures & Tables
References
1.
Breatnach E, Abbott GC, Fraser RG (1984) Dimensions of the
normal human trachea. AJR Am J Roentgenol 142: 903-906. [Crossref]
2.
Carden KA, Boiselle PM, Waltz DA, Ernst A (2005)
Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth
review. Chest 127: 984-1005. [Crossref]
3.
Celik B, Bilgin S, Yuksel C (2011) Mounier-Kuhn syndrome: a
rare cause of bronchial dilation. Tex Heart Inst J 38: 194-196. [Crossref]
4.
Pais C, Silva RC, Gomes T, Carvalho S (2018) A Case of
Tracheomalacia in Chronic Obstructive Pulmonary Disease: What Went Wrong? Eur
J Case Rep Intern Med 5: 000906. [Crossref]
5.
Woodring J, Barrett P, Rehm, Nurenberg P (1989) Acquired
tracheomegaly in adults as a complication of diffuse pulmonary fibrosis. Am
J Roentgenol 152: 743-747. [Crossref]
6.
Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A et al.
(2018) The SCARE 2018 statement: Updating consensus Surgical CAse REport
(SCARE) guidelines. Int J Surg 60: 132-136. [Crossref]
7.
Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A et al.
(2018) The PROCESS 2018 Statement: Updating Consensus Preferred Reporting Of
CasE Series in Surgery (PROCESS) Guidelines. Int J Surg 60: 279-282. [Crossref]
8.
Feist JH, Johnson TH, Wilson RJ (1975) Acquired
tracheomalacia: etiology and differential diagnosis. Chest 68: 340-345.
[Crossref]
9. Gaissert HA, Lofgren RH, Grillo HC (1993) Upper airway compromise after inhalation injury. Complex strictures of the larynx and trachea and their management. Ann Surg 218: 672-678. [Crossref]
10. Katlic MR, Burke JF (1981) Severe low-pressure cuff tracheal injury in burn patients. Intensive Care Med 7: 89-92. [Crossref]
