Class III malocclusion camouflage treatment in adults: A Systematic Review
A B S T R A C T
Objective: To evaluate the effects of camouflage treatment of Class III malocclusion in adults.
Methods: An electronic search was performed in MEDLINE/PubMed, Embase, Scopus, Web of Science, Google Scholar, Lilacs, and Cochrane databases, without limitations regarding publication year or language. Studies evaluating nongrowing individuals with Class III malocclusion undergoing orthodontic camouflage treatment with any orthodontic technique, including extraction and non-extraction approaches, were considered. Study selection, data extraction, and risk of bias assessment according to a modified Downs and Black checklist were performed by two independent reviewers. A third evaluator was included if disagreements emerged.
Results: Nine studies were included in the review. Eight presented high risk of bias. Different methods for Class III malocclusion correction were described and included maxillary and mandibular premolar extractions, mandibular incisor extraction, Class III elastics and distalization of the mandibular dentition. Extractions in the mandibular arch resulted in lingual tipping and retrusion of the mandibular incisors, and labial tipping and protrusion of the maxillary incisors. The use of Class III intermaxillary elastics promoted proclination of the maxillary incisors, extrusion of the maxillary molars, distal tipping of the mandibular molars, extrusion of the mandibular incisors, and clockwise rotation of the mandible. Distalization of the mandibular dentition resulted in distal tipping of the mandibular molars, retroclination and retraction of the mandibular incisors, and counter clockwise rotation of the mandible.
Conclusions: Treatment changes are influenced by the method used to correct the Class III malocclusion and are primarily dentoalveolar
Keywords
Class III treatment, adult treatment, evidence-based orthodontics, Class III
Introduction
Class III malocclusion is considered a real challenge for the orthodontist [1, 2]. In adult patients, treatment alternatives usually are orthodontic treatment combined with orthognathic surgery or orthodontic camouflage treatment. In severe cases, surgical procedures are indicated to correct the discrepancy and to improve facial aesthetics and function [3, 2]. In mild to moderate Class III malocclusions or when the patient declines orthognathic surgery and is satisfied with his/her facial appearance, camouflage treatment is a valid option, when well indicated [4, 5]. A correct diagnosis with the establishment of realistic treatment goals is necessary to prevent undesirable side effects [1, 5]. When the treatment plan includes dentoalveolar compensation, the costs and benefits involved must be carefully evaluated [1, 5]. It is known that excessive dental compensations may result in undesirable facial aesthetics [5].
Camouflage treatment can be carried out by different approaches and may include teeth extractions, distalization of the mandibular dentition, and use of Class III intermaxillary elastics [2, 6-13]. Different approaches result in different outcomes and an overview of the effects of camouflage treatment in adults is not available as a systematic review. Therefore, the aim of the present review was to assess the effects of camouflage treatment of Class III malocclusion in nongrowing patients.
Methods
I Registration
The systematic review was prospectively registered in the PROSPERO database registration number CRD42017068642 and is reported according to the PRISMA guidelines [14].
II Information sources and search
Electronic databases were searched up to January 2019. A systematic electronic search was performed in MEDLINE/PubMed, Embase, Scopus, Web of Science, Google Scholar, Lilacs, and Cochrane databases. No limitations regarding publication year, status or language were applied. Mesh terms and free text words were used in the search. The MEDLINE/PubMed search strategy was: (Class III malocclusion OR Angle Class III malocclusion OR mesiocclusion OR Angle class III OR prognathism OR prognat* OR anterior crossbite) AND (compensatory OR compensat* OR compensation OR camouflage OR non-surgical OR "non-surgical" OR nonsurgical OR conservative). Additional studies were identified by reviewing the reference lists of relevant articles. Unpublished studies were searched on ClinicalTrials.gov.
III Eligibility criteria and study selection
To be included in the review, studies had to meet the following inclusion criteria: (1) Types of studies: randomized or non-randomized clinical studies (prospective or retrospective); (2) Participants: nongrowing individuals with Class III malocclusion, undergoing orthodontic camouflage treatment; (3) Interventions: Class III malocclusion camouflage treatment with any orthodontic technique, including extraction and non-extraction treatment; (4) Primary outcomes: incisor position measured on cephalometric radiographs before and after treatment; (5) Secondary outcomes: other dental, skeletal and soft tissue changes measured on cephalometric radiographs before and after treatment.
Reviews, case studies, case series, descriptive or qualitative studies were excluded. Studies that included growing individuals, individuals treated with orthognathic surgery or studies involving participants with cleft lip or palate or any craniofacial deformity were also excluded. The study selection process was carried out independently by two authors. All concerns and disagreements were resolved after discussion with a third reviewer if necessary, until consensus was reached. Possible inclusion was assessed first based on title and secondly based on abstract reading. The full text was assessed for eligibility if the abstract suggested relevance.
IV Data extraction
Data extraction of the selected studies was performed with the use of a data collection form. Information extracted included: authors, publication year, study design, method of evaluation, study location, characteristics of participants (sample size, age, gender), inclusion and exclusion criteria, details of intervention and outcome measures. Data extraction was performed by two authors independently and in duplicate. Disagreements were resolved through discussion.
V Assessment of risk of bias in individual studies
The risk of bias was assessed with a modification of the checklist described by Downs and Black (Table 1). We simplified the last item (power assessment) by scoring this answer at 0 or 1 point, giving 1 point for a preliminary power analysis calculation [15, 16]. Minor adaptations were performed and questions regarding specific topics for Class III malocclusion treatment were included in the reporting section. Items that were not applicable for the study were removed from the checklist (#14 and #24) [16]. Therefore, the maximum score for this modified Downs and Black tool was 28, with a higher score indicating higher methodological quality. Serious methodological limitations were judged to exist when a study collected less than 15 points on the modified checklist [17]. Assessment of risk of bias was performed independently by two authors. Disagreements were resolved through discussion.
VI Summary measures and synthesis of results
Due to heterogeneity of the studies included in this systematic review, mainly in relation to the characteristics of the interventions applied, it was not feasible to perform a meta-analysis. Therefore, a qualitative synthesis of the data was performed by comparing the results from individual studies according to the study characteristics, type of intervention and outcome measures.
Results
I Study selection
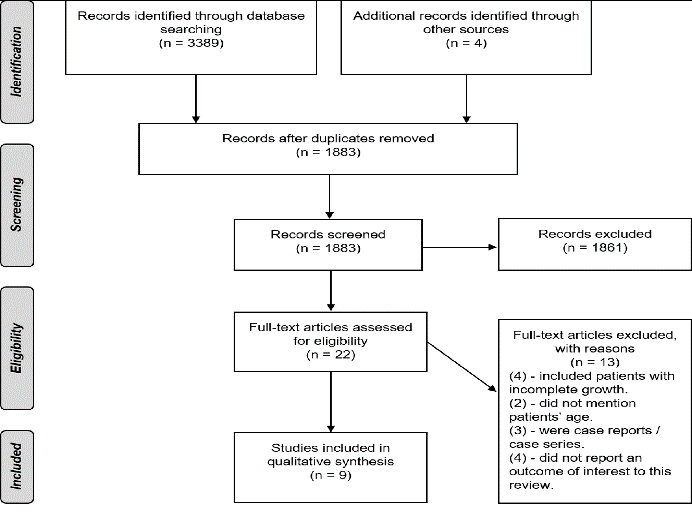
A total of 3393 studies were identified through electronic and hand searching. Of those, 1883 remained after duplicates removal. Titles and abstracts of the remaining studies were assessed, and 1861 were excluded for not being related to the subject or meeting the eligibility criteria. The full texts of 22 articles were assessed for eligibility and 13 were excluded for different reasons (Figure 1). Nine studies fulfilled all inclusion and exclusion criteria and were included in the qualitative synthesis. The characteristics of the included studies are described in (Table 2).
Figure 1: PRISMA flow diagram.
Table 1: Modified Downs and Black checklist.
|
Reporting |
|
1. Is the objective of the study clearly described? |
|
2. Are the main outcomes to be measured clearly described in the Introduction or Methods section? |
|
3. Were inclusion and exclusion criteria clearly stated? |
|
4. Are the characteristics of the patients included clearly described? |
|
5. Is the Class III malocclusion fully described? |
|
6. Are the interventions of interest clearly described? |
|
7. Are the distributors of principal confounders in each group of subjects to be compared clearly described? |
|
8. Are the main findings of the study clearly described? |
|
9. Does the study provide estimates of the random variability in the data for the main outcomes? |
|
10. Have all important adverse events that may be a consequence of the intervention been reported? |
|
11. Have the characteristics of patients lost to follow-up been described? |
|
12. Have actual probability values been reported for the main outcomes except where the probability value is less than 0.001? |
|
External validity |
|
13. Were the patients asked to participate in the study representative of the entire population from which they were recruited? |
|
14. Were those subjects who were prepared to participate representative of the entire population from which they were recruited? |
|
15. Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive? |
|
Internal validity – bias |
|
16. Was an attempt made to blind those measuring the main outcome of the intervention? |
|
17. If any of the results of the study were based on “data dredging”, was that made clear? |
|
18. Do the analyses adjust for different lengths of follow-up of patients? |
|
19. Were the statistical tests used to assess the main outcomes appropriate? |
|
20. Was compliance with the intervention reliable? |
|
21. Were the main outcomes measures used accurate (valid and reliable)? |
|
Internal validity – confounding |
|
22. Were the patients in different intervention groups recruited from the same population? |
|
23. Were the baseline characteristics comparable? |
|
24. Were study subjects in different intervention groups recruited over the same period of time? |
|
25. Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? |
|
26. Were losses of patients to follow-up taken into account? |
|
Power |
|
27. Prior estimate of sample size |
II Study designs and treatment interventions
Of the nine included studies, eight were retrospective cohort and one was retrospective case-control [2, 6-13]. No prospective studies, randomized or not, satisfying the inclusion criteria were found. Different methods of Class III malocclusion treatment were described. Five studies included patients treated with teeth extractions [6-10]. Extraction of two mandibular premolars was performed in two studies while extraction of four premolars was performed in one study [8-10]. One study included patients with extraction of one mandibular incisor [6]. One study included patients treated with and without extractions in the same group [7]. No extraction approaches were implemented in four studies [2,11-13] and included distalization of the mandibular dentition, associated or not with Class III intermaxillary elastics. One study used high-pull J-hook headgear to the mandibular arch to correct the malocclusion [11]. Temporary anchorage devices (TADs) were used in three studies [2, 12, 13]. He et al. associated the MEAW (Multiloop Edgewise Archwire) technique with maxillary mini-implants and modified Class III elastics [2]. Yu et al. performed distalization of the mandibular dentition using ramal plates. Nakamura et al. associated TADs and coil springs or elastic chains [12, 13]. The high heterogeneity presented by the selected studies, especially regarding the treatment approaches, prevented performing a meta-analysis.
III Risk of bias assessment
Detailed information on the risk of bias in individual studies is shown in Table 3. The overall scores ranged from 13 to 21. Four studies scored less than 15 points and presented serious methodological limitations according to the modified Downs and Black checklist [6, 8-10]. Eight studies showed high risk of bias, with the total quality score less than 20, as previously suggested [2, 6-11, 13, 18].
IV Main results
The main results of the included studies are summarized in (Table 2). The studies that included groups with extractions in the mandibular arch presented lingual tipping and retrusion of the mandibular incisors, and buccal tipping, and protrusion of the maxillary incisors after treatment [6-10]. In general, the groups where Class III elastics were used to correct the malocclusion, proclination of maxillary incisors, extrusion of maxillary molars, distal tipping of mandibular molars, extrusion of mandibular incisors, clockwise rotation of the mandibular plane angle, and increase in the lower anterior face height were reported [2,7,12]. Similarly, distal tipping of mandibular molars retroclination and retraction of mandibular incisors, and a counter clockwise rotation of the mandibular plane angle were reported in the studies that performed distalization of the mandibular dentition [11-13].
Table 2: Characteristics of included studies.
|
Method |
Participants |
Age (y) |
Inclusion criteria |
Exclusion criteria |
Interventions |
Total treatment duration (y) |
Class III diagnosis |
Outcomes |
|
Lew (1990) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: not specified. |
N=38 (10 male, 28 female) |
24.3 (SD=3.2) |
True Class III dental malocclusion (without mandibular displacement). |
- |
Extraction of mandibular first premolars. Edgewise technique without the use of extraoral appliances or Class III elastics. Anchorage control during space closure mechanics in the mandibular arch was boosted by a lingual arch in all cases. |
1.7 (SD=3.2) |
Molar relationship of half to full-unit Class III; ANB= -2.3° (SD=2.2); overjet= -4.2 mm (SD=2.8); |
Cephalometric changes: Increase in: NU1-HP, GLs-HP. Decrease in: NL1-HP, NL6-HP, CmSnLs, GLi-HP. |
|
Faerovig and Zachrisson (1999) |
||||||||
|
Retrospective, cohort. Cephalometric and model analysis. Setting: private practice and Department of Orthodontics, University of Oslo. |
N=36 (15 male, 21 female) |
27.8 (SD=11.1) |
Nongrowing adult; occlusion with tendency toward or established mild-to-moderate Class III malocclusion with reduced or no overbite; mild-to-moderate anterior mandibular crowding. |
- |
Extraction of one mandibular incisor. Edgewise technique. Nineteen patients received orthodontic treatment in both maxilla and mandible and 17 were treated only in the mandibular arch. |
1.5 (SD=0.6) |
Tendency toward or established mild-to- moderate Class III malocclusion. |
Retrusion and retroinclination of mandibular incisors. |
|
Ning et al. (2009) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: Department of Orthodontics, School of stomatology, Fourth Military Medical University, China. |
N=13 (5 male, 8 female) |
22.0 (SD=4.5) |
Molar relationship between half- to full-unit Class III; anterior crossbite; concave facial profile; -3°<ANB<0; no mandibular shift due to occlusal interference or premature contact of teeth; no congenitally missing teeth (excluding third molars); severe crowding in the maxillary arches (arch length discrepancy < -8 mm); patients and their families intensely rejected surgery; adult patients (ages ≥ 17 years); no subjects had undergone orthodontic therapy of any type prior to this treatment. |
- |
Extraction of 4 premolars. Standard edgewise technique. Class III elastics were used in some cases where required. |
2.1 (SD=0.4) |
Molar relationship of half to full-unit Class III; ANB= -2° (SD=0.7) |
Cephalometric changes: Increase in: Cm.Sn.Ls. Decrease in: U1.SN, L1.MP, U1.L1, L1.NB, L1-NB, Li-E, Li-H, Ls-RL2, Li-RL2 |
|
Ning and Duan (2010) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: Department of Orthodontics at the Fourth Military Medical University. |
N=28 (15 male, 13 female). |
18.8 |
Anterior crossbite; Class III molar relationship, no mandibular shift due to occlusal interference or premature contact of teeth; concave facial profile; −4.0° ≤ ANB < 0°; over the adolescent growth spurt; originally classified as surgical cases by other orthodontists but the patients and their families rejected surgical treatment. |
- |
Extraction of 2 mandibular premolars. Standard edgewise technique. Class III elastics were used in some cases when required. |
2.0 (SD=0.6) |
Molar relationship of half-unit Class III or superior; ANB= -2.4° (SD=2.5). |
Cephalometric changes: Increase in: U1.SN, U1.L1, Ls-E, overjet. Decrease in: L1.MP, L1.NB, L1-NB, Li-E, Li-H, Cm.Sn.Ls, Li-RL2. |
|
Kuroda et al. (2010) |
||||||||
|
Retrospective, cohort. Cephalometric and plaster cast analysis. Setting: private practice. |
N=14 (4 male, 10 female) |
21.1 (SD=4.4) |
ANB angle ≤ 1.0° (range -2.0° to 1.0°), Angle Class III molar relationship, and no congenital deformity in the craniofacial area. |
- |
No extraction. Association between edgewise appliance (The Alexander Discipline) and high-pull J-hook headgear applied directly to the mandibular archwire with 200 g of force on each side at night only. Short Class III elastics were used for 7.9 months to maintain the occlusion. The mandibular third molars were extracted in all subjects before treatment. |
2.2 (SD=0.5) |
Angle Class III molar relationship; ANB= 0.2° (SD=1.0); Wits= -6.0 mm (SD= 2.8); overjet= 0 mm (SD=1.2). |
Cephalometric changes: Increase in: U1.FH, Wits, U1-NA, L1e-MP, overjet, overbite. Decrease in: FH.Occ, L1.MP, L6.MP, L1-NB, L1-A-Po, L1e-PTV, L1a-PTV, L6c-PTV, L6a-PTV, E line- mandibular lip. Model analysis change: intermolar width increased. |
|
He et al. (2013) |
||||||||
|
Retrospective, case control. Cephalometric analysis. Setting: Department of Orthodontics, West China Hospital of Stomatology, Chengdu, China. |
N=44 Divided in two groups: Experimental group: 20 patients (10 male, 10 female) Control group: 24 patients (10 male, 14 female)
|
Experimental group: 20.6 (SD=4.0) Control group: 21.3 (SD=1.9) |
(1) mild to moderate skeletal Class III relationship (-4° ≤ ANB ≤ 0); Angle Class III molar relationship bilaterally; no or mild crowding (<4 mm); lack of a functional mandibular shift and inability of the mandible to move back spontaneously; and lack of temporomandibular disorder symptoms. |
- |
Experimental group: 20 patients treated with MEAW and modified Class III elastics from the maxillary mini-implants. Control group: 24 patients treated with MEAW and long Class III elastics. Mini-implants were placed in the buccal interradicular spaces between the maxillary second premolars and the first molars in the experimental group. Symmetric or asymmetric light Class III elastics (5/16 inch and weight 3.5 ounces) were used from the implants in the experimental group and from the maxillary second molars in the control group to the first loops on the MEAW (mesial to the canines). |
- |
Angle Class III molar relationship bilaterally. Experimental group: ANB= -1.9° (SD= 1.3); Wits= -9.8 mm (SD= 1.9); overjet= -0.9 mm (SD= 1.3). Control group: ANB= -2.1° (SD= 1.5); Wits=-8.8 mm (SD= 2.1); overjet= -1.3 mm (SD= 2.3). |
Changes in experimental group: Increase in: ODI, U1-L1°, U1-SN°, L1-MP (mm), Wits, Overjet, Overbite. Decrease in: OP-SN, Pog-McNa line, APDI, L1.MP, L6.MP, L6-MP, U6-FHV, L1-FHV, L6-FHV, LL-EP. Changes in control group: Increase in: S-Go/N-Me, ODI, U1-PP, U6-PP, L1-MP, L6-MP, U1-FHV, Wits, Overjet, Overbite, UL-EP, LL-EP. Decrease in: OP-SN, SN-MP, Pog-McNa line, APDI, U1.SN, L1.MP, L6.MP, L1-FHV, L6-FHV. |
|
Janson et al. (2014) |
||||||||
|
Retrospective, cohort. Cephalometric analysis and occlusal evaluation (TPI). Setting: private office file. |
N=23 (10 male, 13 female) |
25.2 (SD= 6.7) |
Dental and skeletal Class III malocclusion (ANB, NAP and Wits) with at least an end-to-end bilateral Class III molar relationship, anterior and posterior crossbites, and concave facial profile. |
- |
Fourteen patients were treated with two mandibular premolar and 6 with two mandibular first molar extractions. Three patients were treated without extractions. |
3.1 (SD= 0.9) |
At least an end-to-end bilateral Class III molar relationship; ANB= -2.91° (SD= 2.99); Wits= -9.40 mm (SD= 4.63); overjet= -1.26 mm (SD= 1.99). |
Cephalometric changes: Increase in: A-NPerp, Co-A, Co-Go, Co-Gn, ANB, Wits, NAP, LAFH, Mx1.NA, IS.PP, Mx6-PP, Md1-MP, Md6-MP. Decrease in: SNB, Md1.NB, Md1-NB, Md1.MP, overjet, overbite. Occlusal changes: TPI change: 9.85 Percent TPI reduction: 82.17% |
|
Yu et al. (2016) |
||||||||
|
Retrospective, cohort (not clear). Cephalometric analysis. Setting: Department of Orthodontics, Seoul St. Mary’s Hospital, The Catholic University of Korea. |
N=22 (11 male; 11 female) |
23.9 (SD=5.5) |
Patients older than 18 years at the start of treatment, with dental Class III malocclusion with more than a one-half cusp discrepancy at the molars, missing or extracted third molars, and no syndrome or systemic disease. |
- |
Patients received ramal plates for mandibular molar distalization, placed in the retromolar fossa between the anterior border of the mandibular ramus and the temporal crest. Power chain elastics were connected from the plate hooks to the first molar bracket hooks to deliver a force of 300 g per side. |
- |
Angle Class III molar relationship with more than ½ cusp discrepancy; ANB= 0.61° (SD= 3,04); Wits= -6.02 mm (SD=3.35). |
Cephalometric changes: Increase in: 6R-FH, 6C-MP, ANB, Wits. Decrease in: 1C-FH, 1R-FH, 6C-VFH, 6R-VFH, 1C-VFH, 6.FH, 1.FH, 1C-MP, 1R-MP, 6C-VMP, 6R-VMP, 1C-VMP, 1.MP, SNB, Pog-Nperp, TVL-LL, TVL-Pog’. |
|
Nakamura et al. (2017) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: Department of Orthodontics, Okayama University Hospital, Japan. |
N=23 Divided in two groups according to treatment modality: TADs: 11 patients (2 male, 9 female). Elastic: 12 patient (5 male, 7 female).
|
TADs: 25.1 (SD=12.9) Elastic: 18 (SD=2.7) |
Angle Class III molar relationship, mild or moderate skeletal Class III discrepancy, nongrowing patients with nonextraction orthodontic treatment, and comprehensive orthodontic treatment with a multibracket edgewise appliance (0.018 3 0.025-in slot). |
Congenital deformity in the craniofacial area and retreatment patient. |
TADs: Distalization was performed with miniscrews, miniplates, or titanium screws, placed on the retromolar pad (3 patients) or on the buccal sides. After 4 weeks of TADs placement, a distal force (estimated at either 150 or 200 g) was directly applied on the hook between the canine and first premolar with closing coils. Elastic: patients were treated with Class III elastics from the maxillary first molar to the mandibular canine. |
TADs: 3.0 (SD= 1.0). Elastic: 2.7 (SD= 1.0).
|
Angle Class III molar relationship. TADs: ANB= -1.0° (SD= 2.0); overjet= -0.5 mm (SD= 2.6). Elatic: ANB= 0.4° (SD= 1.0); overjet= 0.6 mm (SD= 2.3). |
Changes in TADs: Increase in: U1.SN, L6.MP, overjet, U6-PP. Decrease in: Occ plane. Changes in Elastic: Increase in: ANB, SN.MP, y-axis, U1.SN, L1.MP, L6.MP, U6-PP, overjet. Decrease in: Occ plane. |
Discussion
To the best of our knowledge, this is the first systematic review on the effects of Class III malocclusion camouflage treatment in adults. One systematic review investigated the different treatments of Angle Class III malocclusion in adults, but only two studies that evaluated surgical interventions were included, since the review included solely randomized or quasi-randomized controlled trials [19]. At the same time, several systematic reviews investigated the effects of Class III malocclusion treatment in growing patients with different treatment approaches [18, 20-22]. Despite a wide bibliographic search, we only found nine studies, and all of them were retrospective. Since there is a lack in the literature of randomized controlled clinical trials or even prospective trials on the effects of Class III malocclusion camouflage treatment in adults, we had to perform this review with the retrospective studies found. Therefore, in the absence of stronger evidence, they can provide information to guide clinicians.
Table 3: Quality assessment of the studies.
|
Study |
Reporting (0-13) |
External validity (0-3) |
Bias (0-6) |
Confounding (0-5) |
Power (0-1) |
Total (0-28) |
|
Lew (1990) |
8 |
0 |
4 |
1 |
0 |
13 |
|
Faerovig and Zachrisson (1999) |
9 |
0 |
4 |
1 |
0 |
14 |
|
Ning et al. (2009) |
9 |
1 |
3 |
1 |
0 |
14 |
|
Ning and Duan (2010) |
9 |
1 |
3 |
1 |
0 |
14 |
|
Kuroda et al. (2010) |
9 |
0 |
5 |
1 |
0 |
15 |
|
He et al. (2013) |
10 |
1 |
5 |
3 |
0 |
19 |
|
Janson et al. (2014) |
9 |
0 |
5 |
1 |
0 |
15 |
|
Yu et al. (2016) |
11 |
1 |
4 |
1 |
1 |
18 |
|
Nakamura et al. (2017) |
11 |
1 |
4 |
4 |
1 |
21 |
We evaluated the quality of the studies with a modified Downs and Black checklist and most studies presented high risk of bias. Only one study presented quality score higher than 20 [12]. The small number of participants, the lack of sample size estimation and the absence of comparison groups were some of the main shortcomings. Several reasons prevented some articles to be included in this review. Since our main objective was to evaluate the effects of camouflage treatment in adults, articles that did not specify the patients’ age had to be excluded, even when it was related to the permanent dentition. There are cases where a control group or at least a comparison group is required to include a study in a systematic review [18, 23]. Since the articles included only nongrowing patients, the lack of a comparison group was not considered an exclusion criterion for the study selection, as growth would not be considered a confounding factor [24]. Heterogeneity was observed in malocclusion severity and type of appliance used. There was a lack of standardization in the description of Class III malocclusion. Identification of malocclusion severity is essential to characterize the sample, describe the treatment difficulty, and, most importantly, determine the best treatment approach [25]. Although description of anteroposterior molar relationship is essential to evaluate and compare treatment results, it was not clearly described in the included studies. Even in nongrowing patients, long-term follow-up is required to confirm effectiveness of the employed treatment. Most included studies focused only on the short-term treatment results, with a lack of long-term follow-up. One study evaluated the effects of mandibular incisor extraction and presented a 4.3-year follow-up (SD=2.3 years) with stable results [6]. It is important to emphasize that all patients kept bonded mandibular lingual retainers at the time of follow-up in that study. Another study evaluated the effects of the high-pull J-hook headgear at least 2 years after the retention period and observed minimal horizontal relapse of the maxillary and mandibular incisors, indicating that the treatment results were fairly stable [11]. From clinical observation, the occlusion was well-maintained when the effects of the MEAW technique with and without mini-screws were evaluated, despite the fact that some statistically significant differences were found one year after retention [2]. Still, short-term favorable results are not conclusive and robust enough to allow prediction of the long-term treatment effects achieved by the appliances used.
Cephalometric changes
Extraction groups
The patterns of extractions varied in the studies and included extraction of two mandibular premolars, extraction of four premolars and of one mandibular incisor [6, 8-10]. Extraction of four premolars had the main goal of relieving the maxillary arch crowding and decreasing the mandibular arch. It was indicated only in cases with great length discrepancy (over 8 mm) [10]. Differences in maxillary incisor position were observed in cases where only two mandibular premolars were extracted and resulted in their labial tipping [8, 9]. Most of the dental changes were seen in the position of the mandibular incisors, characterized as retroclination and retrusion.
Non-extraction group
Two studies included groups that used Class III intermaxillary elastics to correct the malocclusion [2, 12]. The mechanics resulted in counter clockwise rotation of the occlusal plane, increase in mandibular plane angle and clockwise rotation of the mandible, and increased anterior face height. Therefore, the use of intermaxillary Class III elastics should be avoided in patients with open bite and high mandibular plane angle and indicated for patients with short face and mandibular prognathism. Four studies attempted to restrain the effects to the mandibular arch. Molar uprighting was the main factor that contributed to correction of the Class III relationship when the J-hook headgear and the Class III elastics with maxillary mini-screws were used [2, 11]. The effects promoted by the two mechanics were similar and characterized by retroclination and extrusion of mandibular incisors and distal tipping of the mandibular molars. Since extrusion of anterior teeth benefits open bite correction, both mechanics could be suitable to correct Class III malocclusions with open bite tendency. The insertion of TADs in the mandibular arch allowed distalization of the mandibular dentition [12, 13]. Further investigations are necessary to clarify the relationship between TADs insertion sites and the effects in mandibular dentition distalization. The selected studies included patients with mild to moderate skeletal Class III malocclusions. For those patients, almost all of the studies reported achievement of satisfying and adequate results. Only one reported a few cases with a tendency to unilateral or edge-to-edge canine or premolar relationships [6]. Because the skeletal changes were mostly characterized by changes in the mandibular plane angle and changes in the skeletal bases anteroposterior relationship were not obvious in most of the studies, it is important to emphasize that orthodontic camouflage treatment for skeletal Class III patients has limited results. Thus, for severe cases, surgical orthodontic treatment is the best option.
Conclusion
From the limited available evidence, it is possible to suggest that the treatment changes are influenced by the method used to correct the Class III malocclusion. The treatment effects are primarily dentoalveolar. The quality of the evidence available was low, with most of the studies classified as having high risk of bias. Further studies with an improved quality level are needed to determine the effects of Class III malocclusion camouflage treatment.
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable.
Acknowledgements
Not applicable.
Article Info
Article Type
Review ArticlePublication history
Received: Mon 07, Oct 2019Accepted: Fri 15, Nov 2019
Published: Fri 29, Nov 2019
Copyright
© 2023 Karine Laskos Sakoda Sakoda. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDOA.2019.01.04
Author Info
Arnaldo Pinzan Aron Aliaga-Del Castillo Guilherme Janson Karine Laskos Sakoda Sakoda Sérgio Elias Neves Cury Silvio Bellini-Pereira
Corresponding Author
Karine Laskos Sakoda SakodaDepartment of Orthodontics, Bauru Dental School, University of São Paulo, Brazil
Figures & Tables
Table 1: Modified Downs and Black checklist.
|
Reporting |
|
1. Is the objective of the study clearly described? |
|
2. Are the main outcomes to be measured clearly described in the Introduction or Methods section? |
|
3. Were inclusion and exclusion criteria clearly stated? |
|
4. Are the characteristics of the patients included clearly described? |
|
5. Is the Class III malocclusion fully described? |
|
6. Are the interventions of interest clearly described? |
|
7. Are the distributors of principal confounders in each group of subjects to be compared clearly described? |
|
8. Are the main findings of the study clearly described? |
|
9. Does the study provide estimates of the random variability in the data for the main outcomes? |
|
10. Have all important adverse events that may be a consequence of the intervention been reported? |
|
11. Have the characteristics of patients lost to follow-up been described? |
|
12. Have actual probability values been reported for the main outcomes except where the probability value is less than 0.001? |
|
External validity |
|
13. Were the patients asked to participate in the study representative of the entire population from which they were recruited? |
|
14. Were those subjects who were prepared to participate representative of the entire population from which they were recruited? |
|
15. Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive? |
|
Internal validity – bias |
|
16. Was an attempt made to blind those measuring the main outcome of the intervention? |
|
17. If any of the results of the study were based on “data dredging”, was that made clear? |
|
18. Do the analyses adjust for different lengths of follow-up of patients? |
|
19. Were the statistical tests used to assess the main outcomes appropriate? |
|
20. Was compliance with the intervention reliable? |
|
21. Were the main outcomes measures used accurate (valid and reliable)? |
|
Internal validity – confounding |
|
22. Were the patients in different intervention groups recruited from the same population? |
|
23. Were the baseline characteristics comparable? |
|
24. Were study subjects in different intervention groups recruited over the same period of time? |
|
25. Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? |
|
26. Were losses of patients to follow-up taken into account? |
|
Power |
|
27. Prior estimate of sample size |
Table 2: Characteristics of included studies.
|
Method |
Participants |
Age (y) |
Inclusion criteria |
Exclusion criteria |
Interventions |
Total treatment duration (y) |
Class III diagnosis |
Outcomes |
|
Lew (1990) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: not specified. |
N=38 (10 male, 28 female) |
24.3 (SD=3.2) |
True Class III dental malocclusion (without mandibular displacement). |
- |
Extraction of mandibular first premolars. Edgewise technique without the use of extraoral appliances or Class III elastics. Anchorage control during space closure mechanics in the mandibular arch was boosted by a lingual arch in all cases. |
1.7 (SD=3.2) |
Molar relationship of half to full-unit Class III; ANB= -2.3° (SD=2.2); overjet= -4.2 mm (SD=2.8); |
Cephalometric changes: Increase in: NU1-HP, GLs-HP. Decrease in: NL1-HP, NL6-HP, CmSnLs, GLi-HP. |
|
Faerovig and Zachrisson (1999) |
||||||||
|
Retrospective, cohort. Cephalometric and model analysis. Setting: private practice and Department of Orthodontics, University of Oslo. |
N=36 (15 male, 21 female) |
27.8 (SD=11.1) |
Nongrowing adult; occlusion with tendency toward or established mild-to-moderate Class III malocclusion with reduced or no overbite; mild-to-moderate anterior mandibular crowding. |
- |
Extraction of one mandibular incisor. Edgewise technique. Nineteen patients received orthodontic treatment in both maxilla and mandible and 17 were treated only in the mandibular arch. |
1.5 (SD=0.6) |
Tendency toward or established mild-to- moderate Class III malocclusion. |
Retrusion and retroinclination of mandibular incisors. |
|
Ning et al. (2009) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: Department of Orthodontics, School of stomatology, Fourth Military Medical University, China. |
N=13 (5 male, 8 female) |
22.0 (SD=4.5) |
Molar relationship between half- to full-unit Class III; anterior crossbite; concave facial profile; -3°<ANB<0; no mandibular shift due to occlusal interference or premature contact of teeth; no congenitally missing teeth (excluding third molars); severe crowding in the maxillary arches (arch length discrepancy < -8 mm); patients and their families intensely rejected surgery; adult patients (ages ≥ 17 years); no subjects had undergone orthodontic therapy of any type prior to this treatment. |
- |
Extraction of 4 premolars. Standard edgewise technique. Class III elastics were used in some cases where required. |
2.1 (SD=0.4) |
Molar relationship of half to full-unit Class III; ANB= -2° (SD=0.7) |
Cephalometric changes: Increase in: Cm.Sn.Ls. Decrease in: U1.SN, L1.MP, U1.L1, L1.NB, L1-NB, Li-E, Li-H, Ls-RL2, Li-RL2 |
|
Ning and Duan (2010) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: Department of Orthodontics at the Fourth Military Medical University. |
N=28 (15 male, 13 female). |
18.8 |
Anterior crossbite; Class III molar relationship, no mandibular shift due to occlusal interference or premature contact of teeth; concave facial profile; −4.0° ≤ ANB < 0°; over the adolescent growth spurt; originally classified as surgical cases by other orthodontists but the patients and their families rejected surgical treatment. |
- |
Extraction of 2 mandibular premolars. Standard edgewise technique. Class III elastics were used in some cases when required. |
2.0 (SD=0.6) |
Molar relationship of half-unit Class III or superior; ANB= -2.4° (SD=2.5). |
Cephalometric changes: Increase in: U1.SN, U1.L1, Ls-E, overjet. Decrease in: L1.MP, L1.NB, L1-NB, Li-E, Li-H, Cm.Sn.Ls, Li-RL2. |
|
Kuroda et al. (2010) |
||||||||
|
Retrospective, cohort. Cephalometric and plaster cast analysis. Setting: private practice. |
N=14 (4 male, 10 female) |
21.1 (SD=4.4) |
ANB angle ≤ 1.0° (range -2.0° to 1.0°), Angle Class III molar relationship, and no congenital deformity in the craniofacial area. |
- |
No extraction. Association between edgewise appliance (The Alexander Discipline) and high-pull J-hook headgear applied directly to the mandibular archwire with 200 g of force on each side at night only. Short Class III elastics were used for 7.9 months to maintain the occlusion. The mandibular third molars were extracted in all subjects before treatment. |
2.2 (SD=0.5) |
Angle Class III molar relationship; ANB= 0.2° (SD=1.0); Wits= -6.0 mm (SD= 2.8); overjet= 0 mm (SD=1.2). |
Cephalometric changes: Increase in: U1.FH, Wits, U1-NA, L1e-MP, overjet, overbite. Decrease in: FH.Occ, L1.MP, L6.MP, L1-NB, L1-A-Po, L1e-PTV, L1a-PTV, L6c-PTV, L6a-PTV, E line- mandibular lip. Model analysis change: intermolar width increased. |
|
He et al. (2013) |
||||||||
|
Retrospective, case control. Cephalometric analysis. Setting: Department of Orthodontics, West China Hospital of Stomatology, Chengdu, China. |
N=44 Divided in two groups: Experimental group: 20 patients (10 male, 10 female) Control group: 24 patients (10 male, 14 female)
|
Experimental group: 20.6 (SD=4.0) Control group: 21.3 (SD=1.9) |
(1) mild to moderate skeletal Class III relationship (-4° ≤ ANB ≤ 0); Angle Class III molar relationship bilaterally; no or mild crowding (<4 mm); lack of a functional mandibular shift and inability of the mandible to move back spontaneously; and lack of temporomandibular disorder symptoms. |
- |
Experimental group: 20 patients treated with MEAW and modified Class III elastics from the maxillary mini-implants. Control group: 24 patients treated with MEAW and long Class III elastics. Mini-implants were placed in the buccal interradicular spaces between the maxillary second premolars and the first molars in the experimental group. Symmetric or asymmetric light Class III elastics (5/16 inch and weight 3.5 ounces) were used from the implants in the experimental group and from the maxillary second molars in the control group to the first loops on the MEAW (mesial to the canines). |
- |
Angle Class III molar relationship bilaterally. Experimental group: ANB= -1.9° (SD= 1.3); Wits= -9.8 mm (SD= 1.9); overjet= -0.9 mm (SD= 1.3). Control group: ANB= -2.1° (SD= 1.5); Wits=-8.8 mm (SD= 2.1); overjet= -1.3 mm (SD= 2.3). |
Changes in experimental group: Increase in: ODI, U1-L1°, U1-SN°, L1-MP (mm), Wits, Overjet, Overbite. Decrease in: OP-SN, Pog-McNa line, APDI, L1.MP, L6.MP, L6-MP, U6-FHV, L1-FHV, L6-FHV, LL-EP. Changes in control group: Increase in: S-Go/N-Me, ODI, U1-PP, U6-PP, L1-MP, L6-MP, U1-FHV, Wits, Overjet, Overbite, UL-EP, LL-EP. Decrease in: OP-SN, SN-MP, Pog-McNa line, APDI, U1.SN, L1.MP, L6.MP, L1-FHV, L6-FHV. |
|
Janson et al. (2014) |
||||||||
|
Retrospective, cohort. Cephalometric analysis and occlusal evaluation (TPI). Setting: private office file. |
N=23 (10 male, 13 female) |
25.2 (SD= 6.7) |
Dental and skeletal Class III malocclusion (ANB, NAP and Wits) with at least an end-to-end bilateral Class III molar relationship, anterior and posterior crossbites, and concave facial profile. |
- |
Fourteen patients were treated with two mandibular premolar and 6 with two mandibular first molar extractions. Three patients were treated without extractions. |
3.1 (SD= 0.9) |
At least an end-to-end bilateral Class III molar relationship; ANB= -2.91° (SD= 2.99); Wits= -9.40 mm (SD= 4.63); overjet= -1.26 mm (SD= 1.99). |
Cephalometric changes: Increase in: A-NPerp, Co-A, Co-Go, Co-Gn, ANB, Wits, NAP, LAFH, Mx1.NA, IS.PP, Mx6-PP, Md1-MP, Md6-MP. Decrease in: SNB, Md1.NB, Md1-NB, Md1.MP, overjet, overbite. Occlusal changes: TPI change: 9.85 Percent TPI reduction: 82.17% |
|
Yu et al. (2016) |
||||||||
|
Retrospective, cohort (not clear). Cephalometric analysis. Setting: Department of Orthodontics, Seoul St. Mary’s Hospital, The Catholic University of Korea. |
N=22 (11 male; 11 female) |
23.9 (SD=5.5) |
Patients older than 18 years at the start of treatment, with dental Class III malocclusion with more than a one-half cusp discrepancy at the molars, missing or extracted third molars, and no syndrome or systemic disease. |
- |
Patients received ramal plates for mandibular molar distalization, placed in the retromolar fossa between the anterior border of the mandibular ramus and the temporal crest. Power chain elastics were connected from the plate hooks to the first molar bracket hooks to deliver a force of 300 g per side. |
- |
Angle Class III molar relationship with more than ½ cusp discrepancy; ANB= 0.61° (SD= 3,04); Wits= -6.02 mm (SD=3.35). |
Cephalometric changes: Increase in: 6R-FH, 6C-MP, ANB, Wits. Decrease in: 1C-FH, 1R-FH, 6C-VFH, 6R-VFH, 1C-VFH, 6.FH, 1.FH, 1C-MP, 1R-MP, 6C-VMP, 6R-VMP, 1C-VMP, 1.MP, SNB, Pog-Nperp, TVL-LL, TVL-Pog’. |
|
Nakamura et al. (2017) |
||||||||
|
Retrospective, cohort. Cephalometric analysis. Setting: Department of Orthodontics, Okayama University Hospital, Japan. |
N=23 Divided in two groups according to treatment modality: TADs: 11 patients (2 male, 9 female). Elastic: 12 patient (5 male, 7 female).
|
TADs: 25.1 (SD=12.9) Elastic: 18 (SD=2.7) |
Angle Class III molar relationship, mild or moderate skeletal Class III discrepancy, nongrowing patients with nonextraction orthodontic treatment, and comprehensive orthodontic treatment with a multibracket edgewise appliance (0.018 3 0.025-in slot). |
Congenital deformity in the craniofacial area and retreatment patient. |
TADs: Distalization was performed with miniscrews, miniplates, or titanium screws, placed on the retromolar pad (3 patients) or on the buccal sides. After 4 weeks of TADs placement, a distal force (estimated at either 150 or 200 g) was directly applied on the hook between the canine and first premolar with closing coils. Elastic: patients were treated with Class III elastics from the maxillary first molar to the mandibular canine. |
TADs: 3.0 (SD= 1.0). Elastic: 2.7 (SD= 1.0).
|
Angle Class III molar relationship. TADs: ANB= -1.0° (SD= 2.0); overjet= -0.5 mm (SD= 2.6). Elatic: ANB= 0.4° (SD= 1.0); overjet= 0.6 mm (SD= 2.3). |
Changes in TADs: Increase in: U1.SN, L6.MP, overjet, U6-PP. Decrease in: Occ plane. Changes in Elastic: Increase in: ANB, SN.MP, y-axis, U1.SN, L1.MP, L6.MP, U6-PP, overjet. Decrease in: Occ plane. |
Table 3: Quality assessment of the studies.
|
Study |
Reporting (0-13) |
External validity (0-3) |
Bias (0-6) |
Confounding (0-5) |
Power (0-1) |
Total (0-28) |
|
Lew (1990) |
8 |
0 |
4 |
1 |
0 |
13 |
|
Faerovig and Zachrisson (1999) |
9 |
0 |
4 |
1 |
0 |
14 |
|
Ning et al. (2009) |
9 |
1 |
3 |
1 |
0 |
14 |
|
Ning and Duan (2010) |
9 |
1 |
3 |
1 |
0 |
14 |
|
Kuroda et al. (2010) |
9 |
0 |
5 |
1 |
0 |
15 |
|
He et al. (2013) |
10 |
1 |
5 |
3 |
0 |
19 |
|
Janson et al. (2014) |
9 |
0 |
5 |
1 |
0 |
15 |
|
Yu et al. (2016) |
11 |
1 |
4 |
1 |
1 |
18 |
|
Nakamura et al. (2017) |
11 |
1 |
4 |
4 |
1 |
21 |
References
- Burns NR, Musich DR, Martin C, Razmus T, Gunel E et al. (2010) Class III camouflage treatment: what are the limits? Am J Orthod Dentofacial Orthop 137: 9.e1-9.e13. [Crossref]
- He S, Gao J, Wamalwa P, Wang Y, Zou S et al. (2013) Camouflage treatment of skeletal Class III malocclusion with multiloop edgewise arch wire and modified Class III elastics by maxillary mini-implant anchorage. Angle Orthod 83: 630-640. [Crossref]
- Georgalis K, Woods MG (2015) A study of Class III treatment: orthodontic camouflage vs orthognathic surgery. Aust Orthod J 31: 138-148. [Crossref]
- Baik HS (2007) Limitations in orthopedic and camouflage treatment for Class III malocclusion. Semin Orthod 3: 158-174.
- Sperry TP, Speidel TM, Isaacson RJ, Worms FW (1977) The role of dental compensations in the orthodontic treatment of mandibular prognathism. Angle Orthod 47: 293-299. [Crossref]
- Faerovig E, Zachrisson BU (1999) Effects of mandibular incisor extraction on anterior occlusion in adults with Class III malocclusion and reduced overbite. Am J Orthod Dentofacial Orthop 115: 113-124. [Crossref]
- Janson G, Souza J, Bombonatti R, Gigliotti M, Andrade Júnior P (2014) Evaluation of dentoalveolar compensation in the treatment of Class III Malocclusion. J Interdiscipl Med Dent Sci 2: 1-6.
- Lew KK (1990) Soft tissue profile changes following orthodontic treatment of Chinese adults with Class III malocclusion. Int J Adult Orthodon Orthognath Surg 5: 59-65. [Crossref]
- Ning F, Duan Y (2010) Camouflage treatment in adult skeletal Class III cases by extraction of two lower premolars. Korean J Orthod 40: 349-57.
- Ning F, Duan Y, Huo N (2009) Camouflage treatment in skeletal Class III cases combined with severe crowding by extraction of four premolars. Orthod Waves 68: 80-87
- Kuroda Y, Kuroda S, Alexander RG, Tanaka E (2010) Adult Class lll Treatment Using a J-Hook Headgear to the Mandibular Arch. Angle Orthod 80: 336-343. [Crossref]
- Nakamura M, Kawanabe N, Kataoka T, Murakami T, Yamashiro T et al. (2017) Comparative evaluation of treatment outcomes between temporary anchorage devices and Class III elastics in Class III malocclusions. Am J Orthod Dentofacial Orthop 151: 1116-1124. [Crossref]
- Yu J, Park JH, Bayome M, Kim S, Kook Y-A et al. (2016) Treatment effects of mandibular total arch distalization using a ramal plate. Korean J Orthod 46: 212-219.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med 6: e1000100. [Crossref]
- Nucera R, Lo Giudice A, Rustico L, Matarese G, Papadopoulos MA et al. (2016) Effectiveness of orthodontic treatment with functional appliances on maxillary growth in the short term: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 149: 600-611. [Crossref]
- Perinetti G, Primozic J, Franchi L, Contardo L (2015) Treatment Effects of Removable Functional Appliances in Pre-Pubertal and Pubertal Class II Patients: A Systematic Review and Meta-Analysis of Controlled Studies. PloS one 10: e0141198. [Crossref]
- Zymperdikas VF, Koretsi V, Papageorgiou SN, Papadopoulos MA (2016) Treatment effects of fixed functional appliances in patients with Class II malocclusion: a systematic review and meta-analysis. Eur J Orthod 38: 113-126. [Crossref]
- Woon SC, Thiruvenkatachari B (2017) Early orthodontic treatment for Class III malocclusion: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 151: 28-52. [Crossref]
- Minami-Sugaya H, Lentini-Oliveira DA, Carvalho FR, Machado MA, Marzola C et al. (2012) Treatments for adults with prominent lower front teeth. Cochrane Database Syst Rev. [Crossref]
- Chatzoudi MI, Ioannidou-Marathiotou I, Papadopoulos MA (2014) Clinical effectiveness of chin cup treatment for the management of Class III malocclusion in pre-pubertal patients: a systematic review and meta-analysis. Prog Orthod 15: 62. [Crossref]
- Rongo R, D'Anto V, Bucci R, Polito I, Martina R et al. (2017) Skeletal and dental effects of Class III orthopaedic treatment: a systematic review and meta-analysis. J Oral Rehabil 44: 545-562. [Crossref]
- Watkinson S, Harrison JE, Furness S, Worthington HV (2013) Orthodontic treatment for prominent lower front teeth (Class III malocclusion) in children. Cochrane Database Syst Rev 30: CD003451. [Crossref]
- Janson G, Mendes LM, Junqueira CH, Garib DG (2016) Soft-tissue changes in Class II malocclusion patients treated with extractions: a systematic review. Eur J Orthod 38: 631-637. [Crossref]
- Pandis N, Cobourne MT (2013) Clinical trial design for orthodontists. J Orthod 40: 93-103. [Crossref]
- Janson G, Sathler R, Fernandes TM, Zanda M, Pinzan A (2010) Class II malocclusion occlusal severity description. J Appl Oral Sci 18: 397-402. [Crossref
]
