Clinical Significance of Oral Care and Oral Management on the Treatment and Prevention of Aspiration Pneumonia in the Elderly: Evidences and Pitfalls
A B S T R A C T
Oral care and oral management are important for preventing aspiration pneumonia (ASP). The main pathology of ASP is microaspiration of oropharyngeal contents during night, swallowing rehabilitation must be necessary for the ASP treatment. However, swallowing rehabilitation cannot totally restore the normal swallowing function. Oral healthcare management should be initiated and continued in parallel with antibiotic treatment of ASP. Oral care helps to prevent aspiration pneumonia by reducing oral bacteria, while oral management helps by improving masticatory and rehabilitating functions. The efficacy of oral care for reducing the incidence of pneumonia has been clearly observed in untreated frail elderly patients, but not in well-cared elderly persons. It has been established that oral care is cyclically significant for the prevention of ASP in the elderly. However, oral problems are not the primary cause of ASP in the elderly. Although there is an amount of evidences of oral care for ASP prevention, there are some controversies of the clinical significance of oral care for ASP treatment.
Keywords
Aspiration pneumonia, dysphagia, oral care, oral management, elderly, nursing and healthcare-associated pneumonia (NHCAP)
Introduction
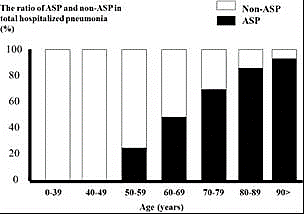
Pneumonia is the leading cause of death in developed countries including Japan, and most of the deaths from pneumonia occur in patients older than 65 years of age [1-3]. The developed countries are facing the advent of unprecedented aging of society, and the field of nursing and the prevalence of aspiration pneumonia (ASP) in both nursing homes and healthcare facilities are rapidly expanding [4-6]. Importantly, ASP is the dominance of hospitalized CAP and hospital-acquired pneumonia (HAP) among the elderly population (Figure 1) [7]. In the therapeutic point of view, ASP comprises two pathological conditions: airspace infiltration with bacterial pathogens and dysphagia-associated misswallowing. The first-line therapy for the treatment of ASP is appropriate antibiotics administration. In addition to an appropriate course of antibiotics, pharmacologic and non-pharmacologic approaches for dysphagia and upper airway management are necessary for the treatment and prevention of ASP in the elderly [8].
Figure 1: Incidence of aspiration pneumonia (ASP) and non-ASP in total pneumonia as a function of age. ASP, aspiration pneumonia; non-ASP, pneumonia without aspiration nor dysphagia [7].
In the non-pharmacologic approaches for ASP, swallowing rehabilitation and oral healthcare are two key components of treatment and further prevention for repeated occurrence of ASP in older populations. Although there is an amount of evidences of oral care for ASP prevention, there are some controversies of the clinical significance of oral care for ASP treatment.
In this review, we summarized the EBM of the clinical significance of oral care for the treatment and/or prevention of ASP in the elderly. Then, we raised the unsolved questions of the clinical roles of oral care for ASP in the elderly.
Aspiration Pneumonia Management Strategies for the Elderly
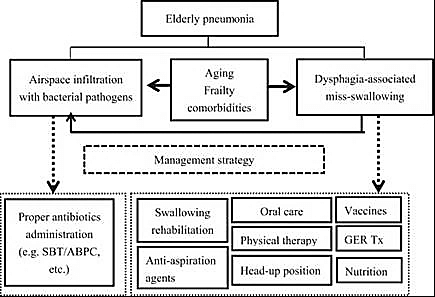
For the bacterial pathogens, the empirical antibiotic therapy recommended for ASP is considered to be appropriate for the majority of elderly patients with ASP [4, 7, 9]. A narrow spectrum of antibiotics, including sulbactam/ampicillin, which are effective against major lower respiratory infection pathogens and anaerobes, may be selected as first-line therapy for ASP in the elderly (Figure 2). For the treatment of dysphagia, pharmacologic approaches for dysphagia and upper airway management are necessary. Several anti-aspiration agents, which improve swallowing dysfunction, are clinically available. Angiotensin-converting enzyme (ACE) inhibitors and cilostazol have reported efficacy in the prevention of pneumonia among older patients who have a history of cerebral infarction [10]. On the other hand, several swallowing disturbance agents are known to exist; anticholinergic medications, which cause dry mouth, and antipsychotic/neuroleptic medications may interfere with swallowing by impairing the elderly person`s ability to move food and swallowing reflexes. These medications should not be administered in elderly patients with a high risk of pneumonia. Both pneumococcal and influenza vaccines are recommended for the administration of the prevention of ASP.
Figure 2: The management strategy for the treatment of pneumonia in relation to its mechanisms. Pneumonia in the elderly is characterized by airspace infiltration with bacterial pathogens and dysphagia-associated misswallowing. SBT/ABPC, sulbactam/ampicillin; GER Tx, treatment for gastroesophageal reflex [8].
For the treatment of dysphagia, non-pharmacologic approaches are strongly necessary for elderly patients with ASP. Since antimicrobial agents cannot improve swallowing problems, dysphagia therapy is a fundamental approach for the treatment of ASP. The main pathology of ASP is microaspiration of oropharyngeal contents during night, swallowing rehabilitation must be necessary for the ASP treatment. Unfortunately, swallowing rehabilitation cannot totally restore the normal swallowing function in patients with ASP. That is why oral healthcare management should be initiated and continued in parallel with antibiotic treatment of ASP [11-15]. Oral care reduces fever and pneumonia incidence among elderly patients with a risk of ASP (Figure 3) [16]. The addition of oral cavity brushing and rehabilitation to conventional oral care is reported to reduce fever in tube-fed patients with tube feeding [17]. Oral hygiene management intervention may be an efficient mortality risk factor modifier in nursing home-associated pneumonia [18]. It has been reported that oral care level, the number of decayed teeth, and tube feeding are significant predictors for the development of ASP.
Figure 3: The rate of pneumonia in elderly people receiving oral care and in those who did not receive oral care [16].
Participants were selected from 11 nursing homes. Nurses or caregivers cleaned their teeth by toothbrush after each meal and scrubbed the pharynx with an applicator with povidone iodine (1%) every day. Dentists assessed oral status once a week for the oral-care group. Participants were randomly assigned oral care or no active treatment in September, 1996, and were followed up for 2 years.
Importantly, fasting does not prevent the development of ASP in the frail elderly. The silent aspiration of oropharyngeal content, which predominantly occurs during night, may not be avoided by the fasting itself. Then, percutaneous endoscopic gastrostomy (PEG) is sometimes performed as a means of preventing ASP; however, there is little evidence to indicate that it prevents pneumonia [19].
Definition of Oral Care and Oral Management
In the literature, oral care and oral management are often overlapping and confused. In this review, we determined the terms of oral care and oral management as follows: “Oral care” includes tooth brushing or mouth rinsing for oral cavity cleansing [1]. The term “oral management” is a more comprehensive notion of oral care, which refers to oral hygiene as well as maintenance and restoration of chewing and swallowing function using oral rehabilitation and dental treatment through the use of prosthesis such as dentures. Thus, oral management usually aims to maintain optimal oral intake and speech function. Effective oral management requires multidisciplinary collaboration between dentists, dental hygienists, pulmonologists, rehabilitation physicians, nursing staff, pharmacists, speech therapists, physical therapists, occupational therapists, and nutritionists. But dentists and dental hygienists have a central role in good performance of oral management for the elderly patients with dysphagia.
The Prevention of Postoperative ASP by Using Oral Care and Oral Management
One of the major postoperative complications is pneumonia. Because many surgeries performed on elderly patients with cancer and orthopedic disorders in the recent aged society, the postoperative pneumonia is largely depending on the ASP mechanism. It has been repeatedly reported that preoperative oral care effectively prevents postoperative pneumonia in patients undergoing surgery under general anaesthesia [20-22]. In addition to the reduction of postoperative pneumonia, and perioperative oral management reduces the incidence of febrile episodes, probably due to silent aspiration [23, 24]. Based on these evidences, most of the general hospitals prepared for the clinical path of perioperative oral care program including preoperative and postoperative oral management, collaborated with dental professionals [25]. Further, patients who undergo esophageal or head and neck cancer surgery and those with stroke are predisposed to oral dysfunction and dysphagia. Dental prosthetic rehabilitation is necessary to maintain and restore oral and swallowing function to prevent aspiration pneumonia.
Oral Management for Elderly Patients Requiring Long-Term Care in Homes or Care Facilities: Clinical Significance of NHCAP
Many older subjects faced the risk of ASP. In particular, elderly patients in special care facilities and nursing homes have the highest risk of pneumonia. The type of pneumonia has been recently determined as nursing and healthcare associated pneumonia (NHCAP) in Japan. The persons requiring long-term care sometimes cannot care for themselves due to diminished activities of daily living and therefore require a caregiver. A study conducted with bedridden elderly patients hospitalized for chronic illnesses found that when these patients received proactive oral care (tooth brushing), fevers at 1 month after admission and pneumonia during hospitalization occurred less frequently [17]. For patients with a risk of NHCAP, oral care and oral management have a beneficial effect on the prevention of pneumonia development.
Basic Oral Care Techniques
Oral care is performed in the following order: oral moisturizing, softening of dried contaminants, cleaning of tooth surfaces, removal of softened contaminants, swabbing, and oral moisturizing (Table 1). In addition to these basic techniques, the oral cavity is suctioned as appropriate during care to prevent the aspiration of contaminated saliva and water. Patients who require oral care often suffer from dry lips and/or mouth. The appropriate oral moisturizing is necessary for the good performance of the initiation of oral management. In the event of severe dry mouth, dried contaminants are softened via humidification. Oral moisturizer is applied to dried desquamated epithelium and phlegm on the oral mucosa to soften them. Once brushing is completed, care is performed, starting with the moisturized mucosa. The tongue is cleaned from back to front with a tongue brush applied with light pressure. In the event of severe dry mouth, swabbing and oral moisturizing are concluded by lightly applying oral moisturizer to the patient’s lips and oral cavity.
Table 1: Basic oral care techniques.
|
i) Oral moisturizing. |
The lips and mouth are moistened with a moisturizer or mouthwash and then cleaned. An oral moisturizer is applied to the lips and then to the dry oral mucosa. |
|
ii) Softening of dried contaminants. |
Oral moisturizer is applied to dried desquamated epithelium and phlegm on the oral mucosa to soften them. After the moisturizer is applied, desquamated epithelium requires several minutes to soften, during which time tooth surfaces are cleaned. |
|
iii) Cleaning of tooth surfaces. |
A soft toothbrush is used for patients with bleeding tendency or severe pain. An interdental brush is also used as necessary. |
|
iv) Removal of softened contaminants. |
Once brushing is completed, care is performed, starting with the moisturized mucosa. The contaminants are removed by brushing them out from the back of the oral cavity toward the opening of the patient’s mouth using a sponge brush. The tongue is cleaned from back to front with a tongue brush applied with light pressure. |
|
v) Swabbing and oral moisturizing. |
Oral care results in a temporary increase in the number of oral bacteria. The contaminants must be collected properly. Patients who are capable of gargling are asked to gargle. Patients who cannot gargle or are at a high risk of aspiration should not be forced to gargle. Instead, oral bacteria can be collected by wiping tooth surfaces and oral mucosa with oral cleansing wipes. |
The Controversy Results of Oral Care for the Prevention of Pneumonia in Elderly Patients in Several Circumstances
The efficacy of oral care for reducing the incidence of pneumonia has been clearly observed in untreated frail elderly patients, but not in well-cared elderly persons. Yoneyama and others first described that oral care lowered the risk of pneumonia in institutionalized elderly patients in 1999 [16]. At that time, institutionalized elderly patients had never performed standardized oral care in the facilities. The efficacy of oral care was strongly observed in the untreated elderly subject with untreated oral hygiene. In these days, standardized oral care and oral management are commonly performed in nursing homes and hospitals. Thus, the preventive effect of oral care for ASP was rarely identified in the facilities and hospitals. The Cochrane systematic review concerning oral care for nursing home-acquired pneumonia (NHAP) claimed that no high-quality evidence could determine which oral care measures are most effective for reducing NHAP. Although low-quality evidence suggests that professional oral care could reduce mortality due to pneumonia in nursing home residents when compared to usual care, this finding must be considered with caution. Evidence for other outcomes is inconclusive [26].
So far, few clinical guidelines for cancer treatment recommend oral management by dentists as routine perioperative care. Pneumonia can be a complication of esophageal cancer. Shin J et al. analysed 3412 esophagectomy cases of which 812 were open, and 2600 were thoracoscopic surgery [27]. The postoperative aspiration pneumonia was 4.5 % of 730 patients with open surgery and 4.9% of 1271 patients with thoracoscopic esophagectomy. The preoperative oral management (POM) by dentists reduced the risk of AP to 2.2% and 3.2% of surgery, respectively. Similar results obtained by other researches [28]. The results suggested that in patients undergoing open or thoracoscopic esophagectomy, POM by dentists prevented the occurrence of postoperative aspiration pneumonia. However, the risk difference of postoperative aspiration pneumonia ranged from only -2.49% to -2.02% between the POM and control groups. The evidence of the preventive effect of POM in esophageal cancer patients is very solid, but the clinical impact may be very limited.
Conclusion
Oral care and management have a potential role in preventing aspiration pneumonia by reducing oral bacteria and improving oral functions. The efficacy of oral care for reducing the incidence of pneumonia has been clearly observed in untreated frail elderly patients, but not in well-cared elderly persons. It has been established that oral care is cyclically significant for the prevention of ASP in the elderly. However, oral problems are not the primary cause of ASP in the elderly. For the treatment of dysphagia, both approaches, such as swallowing rehabilitation and oral healthcare, must be necessary for elderly patients with a high risk of ASP in nursing homes. Although there is an amount of evidences of oral care for ASP prevention, there are some controversies of the clinical significance of oral care for ASP treatment.
Conflicts of Interest
None.
Article Info
Article Type
Review ArticlePublication history
Received: Mon 20, Jul 2020Accepted: Tue 04, Aug 2020
Published: Tue 11, Aug 2020
Copyright
© 2023 Shinji Teramoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2020.04.01
Author Info
Corresponding Author
Shinji TeramotoDepartment of Respiratory Medicine, Tokyo Medical University Hachioji Medical Center, Tokyo, Japan
Figures & Tables
Table 1: Basic oral care techniques.
|
i) Oral moisturizing. |
The lips and mouth are moistened with a moisturizer or mouthwash and then cleaned. An oral moisturizer is applied to the lips and then to the dry oral mucosa. |
|
ii) Softening of dried contaminants. |
Oral moisturizer is applied to dried desquamated epithelium and phlegm on the oral mucosa to soften them. After the moisturizer is applied, desquamated epithelium requires several minutes to soften, during which time tooth surfaces are cleaned. |
|
iii) Cleaning of tooth surfaces. |
A soft toothbrush is used for patients with bleeding tendency or severe pain. An interdental brush is also used as necessary. |
|
iv) Removal of softened contaminants. |
Once brushing is completed, care is performed, starting with the moisturized mucosa. The contaminants are removed by brushing them out from the back of the oral cavity toward the opening of the patient’s mouth using a sponge brush. The tongue is cleaned from back to front with a tongue brush applied with light pressure. |
|
v) Swabbing and oral moisturizing. |
Oral care results in a temporary increase in the number of oral bacteria. The contaminants must be collected properly. Patients who are capable of gargling are asked to gargle. Patients who cannot gargle or are at a high risk of aspiration should not be forced to gargle. Instead, oral bacteria can be collected by wiping tooth surfaces and oral mucosa with oral cleansing wipes. |

References
- Tomomi Mitsuhata, Shinji Teramoto (2020) Epidemiology of Aspiration Pneumonia: How Frequently Does Aspiration Pneumonia Occur in Older Adults? In Shinji Teramoto, Kosaku Komiya (eds.) Aspiration pneumonia: The Current Clinical Giant for Respiratory Physicians (Respiratory Disease Series: Diagnostic Tools and Disease Managements. Springer Nature Springer Ltd. 1-13.
- Gerald R Donowitz (2013) Community-acquired pneumonia: 2012 history, mythology, and science. Trans Am Clin Climatol Assoc 124: 283-293. [Crossref]
- Adamantia Liapikou, Eva Polverino, Catia Cilloniz, Paulo Peyrani, Julio Ramirez et al. (2014) A Worldwide Perspective of Nursing Home-Acquired Pneumonia compared to Community-acquired Pneumonia. Respir Care 59: 1078-1085. [Crossref]
- Shigeru Kohno, Yoshifumi Imamura, Yuichiro Shindo, Masafumi Seki, Tadashi Ishida et al. (2013) Clinical practice guidelines for nursing- and healthcare-associated pneumonia (NHCAP) [complete translation]. Respir Investig 51: 103-126. [Crossref]
- Shinji Teramoto, Masahiro Kawashima, Kosaku Komiya, Shunsuke Shoji (2009) Health care-associated pneumonia may be primary due to aspiration pneumonia. Chest 136: 1702-1703. [Crossref]
- Jordi Carratalà, Analía Mykietiuk, Núria Fernández Sabé, Cristina Suárez, Jordi Dorca et al. (2007) Health care-associated pneumonia requiring hospital admission: epidemiology, antibiotic therapy, and clinical outcomes. Arch Intern Med 167: 1393-1299. [Crossref]
- Shinji Teramoto, Yoshinosuke Fukuchi, Hidetada Sasaki, Koichi Sato, Kiyohisa Sekizawa et al. (2008) High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a prospective multi-center study in Japan. J Am Geriatr Soc 56: 577-579. [Crossref]
- Shinji Teramoto, Kazufumi Yoshida, Nobuyuki Hizawa (2015) Update on the pathogenesis and management of pneumonia in the elderly-roles of aspiration pneumonia. Respir Investig 53: 178-184. [Crossref]
- Shigeru Kohno, Katsunori Yanagihara, Yoshihiro Yamamoto, Issei Tokimatsu, Kazufumi Hiramatsu et al. (2013) Early switch therapy from intravenous sulbactam/ampicillin to oral garenoxacin in patients with community-acquired pneumonia: a multicenter, randomized study in Japan. J Infect Chemother19: 1035-1041. [Crossref]
- K Sekizawa, T Matsui, T Nakagawa, K Nakayama, H Sasaki (1998) ACE inhibitors and pneumonia. Lancet 352: 1069. [Crossref]
- Chia Wei Lin, Yeun Chung Chang, Wen Shiang Chen, Kevin Chang, Hui Ya Chang et al. (2012) Prolonged swallowing time in dysphagic Parkinsonism patients with aspiration pneumonia. Arch Phys Med Rehabil 93: 2080-2084. [Crossref]
- Franceen Kaizer, Anna Maria Spiridigliozzi, Matthew R Hunt (2012) Promoting shared decision-making in rehabilitation: development of a framework for situations when patients with Dysphagia refuse diet modification recommended by the treating team. Dysphagia 27: 81-87. [Crossref]
- Masako Iwamoto, Naoki Higashibeppu, Yasutaka Arioka, Yutaka Nakaya (2014) Swallowing rehabilitation with nutrition therapy improves clinical outcome in patients with dysphagia at an acute care hospital. J Med Invest 61: 353-360. [Crossref]
- Mohamed El Rabbany, Noha Zaghlol, Mohit Bhandari, Amir Azarpazhooh (2015) Prophylactic oral health procedures to prevent hospital-acquired and ventilator-associated pneumonia: a systematic review. Int J Nurs Stud 52: 452-464. [Crossref]
- Keisuke Maeda, Junji Akagi (2014) Oral care may reduce pneumonia in the tube-fed elderly: a preliminary study. Dysphagia 29: 616-621. [Crossref]
- T Yoneyama, M Yoshida, T Matsui, H Sasaki (1999) Oral care and pneumonia. Oral Care Working Group. Lancet 354: 515. [Crossref]
- Kaoru Matsusaka, Atsuko Ohi, Keita Tahata, Ayako Shimizu, Megumi Numata et al. (2013) Addition of oral cavity brushing and rehabilitation reduces fever in tube-fed patients. Geriatr Gerontol Int 13: 1082-1084. [Crossref]
- Carol W Bassim, Gretchen Gibson, Timothy Ward, Brian M Paphides, Donald J Denucci (2008) Modification of the risk of mortality from pneumonia with oral hygiene care. J Am Geriatr Soc 56: 1601-1607. [Crossref]
- Claudio A R Gomes Jr, Régis B Andriolo, Cathy Bennett, Suzana A S Lustosa, Delcio Matos et al. (2015) Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst Rev 2015: CD008096. [Crossref]
- Yasunori Akutsu, Hisahiro Matsubara, Kiyohiko Shuto, Toru Shiratori, Masaya Uesato et al. (2010) Pre-operative dental brushing can reduce the risk of postoperative pneumonia in esophageal cancer patients. Surgery 47: 497-502. [Crossref]
- A J DeRiso 2nd, J S Ladowski, T A Dillon, J W Justice, A C Peterson (1996) Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest 109: 1556-1561. [Crossref]
- Eduardo H Bergan, Bernardo R Tura, Cristiane C Lamas (2014) Impact of improvement in preoperative oral health on nosocomial pneumonia in a group of cardiac surgery patients: a single arm prospective intervention study. Intensive Care Med 40: 23-31. [Crossref]
- Yoshikazu Kobayashi, Koichiro Matsuo, Risa Watanabe, Wataru Fujii, Daisuke Kanamori et al. (2013) The Oral environment in patients under Peri-operative Oral functional management and its intervention effects in our hospital. Jpn J Gerodontol 28: 69-78.
- Senoo Hitomi, Nakano Yuko, Tokumiya Mototomi, Otani Masataka (2015) Efficacy of professional perioperative oral care for elderly patients with femur fractures. J Jpn Soc Dent Med Comp Patient 24: 9-14.
- S L Russell, R J Boylan, R S Kaslick, F A Scannapieco, R V Katz (1999) Respiratory pathogen colonization of the dental plaque of institutionalized elders. Spec Care Dentist 19: 128-134. [Crossref]
- Chang Liu, Yubin Cao, Jie Lin, Linda Ng, Ian Needleman et al. (2018) Oral care measures for preventing nursing home‐acquired pneumonia. Cochrane Database Syst Rev 9: CD012416. [Crossref]
- Jung Ho Shin, Susumu Kunisawa, Kiyohide Fushimi, Yuichi Imanaka (2019) Effects of preoperative oral management by dentists on postoperative outcomes following esophagectomy: Multilevel propensity score matching and weighting analyses using the Japanese inpatient database. Medicine (Baltimore) 98: e15376. [Crossref]
- Yuka Yamada, Takashi Yurikusa, Kohei Furukawa, Yasuhiro Tsubosa, Masahiro Niihara et al. (2019) The Effect of Improving Oral Hygiene through Professional Oral Care to Reduce the Incidence of Pneumonia Post-esophagectomy in Esophageal Cancer. Keio J Med 68: 17-25. [Crossref]
