Coexistence of COVID-19 with Pregnancy: A Challenge to Manage
A B S T R A C T
The number of Coronavirus Disease-19 (COVID-19) cases are on a rise globally due to the highly contagious nature of its causative agent Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Physiological and Immunological changes during pregnancy may put pregnant women at increased risk for severe COVID-19 respiratory infection which may require Intensive care. Along with medical management, physiotherapy interventions namely patient education, relaxation, breathing exercises, positioning in bed, and mobility exercises are an integral part of acute care set up. The aim of this report is to share our experience as a frontline physiotherapist working as an integral part of the medical team in a dedicated COVID-19 Government Tertiary Care Hospital in Mumbai. It highlights physiotherapy management of a COVID-19 patient, in her 24th week of gestation, in an Acute Care Set Up.
Keywords
Coronavirus, pregnant women, physiotherapy, acute care set up
Introduction
In December 2019, in Wuhan, China, the outbreak of novel coronavirus disease was first identified which spread rapidly making it a pandemic as declared on 11th March 2020 by the World Health Organisation (WHO). The main source of infection is through droplets generated by an infected person during coughing, sneezing and talking which may infect other people when inhaled or through contact with contaminated surfaces [1]. Symptoms of COVID-19 are classified as Asymptomatic, Mild (fever, fatigue, breathlessness, sore throat, runny nose, myalgia, expectoration, loss of smell or taste, digestive symptoms namely nausea, vomiting, diarrhoea), Moderate (Pneumonia without hypoxemia), Severe (Pneumonia with hypoxemia; SPO2 <92%) and Critical (ARDS, shock, encephalopathy, cardiac injury, heart failure, coagulation dysfunction, and renal injury) [1, 2].
Most people infected with COVID-19 have mild symptoms and recover easily without any special treatment [1]. The risk of infection and clinical features in pregnant women are similar to that of the general population [3]. However, there are immunological changes during pregnancy making them more susceptible to severe viral infection. On top of this, there is physiological dyspnoea due to pregnancy (increased physiological oxygen demands due to increased maternal metabolism, gestational anaemia, and foetal oxygen consumption) [3, 4]. These factors may put pregnant women in a state of hypoxic compromise requiring hospitalization and ICU admission. In a study done by Dashraath et al., females when affected with COVID-19 during pregnancy; 84% had fever, 28% had cough, 18% had dyspnoea, the mortality rate was zero but 2% required mechanical ventilation, 43% had preterm deliveries with 2% neonatal deaths and 9% IUGR (intra uterine growth retardation) [4]. According to CDC’s MMWR, pregnant women with COVID-19 are 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to receive mechanical ventilation than non-pregnant women [5].
Currently, no COVID-19 specific vaccine or treatment is available. Hence, a multi-disciplinary approach which includes symptomatic medical management, oxygen therapy, physiotherapy, nutritional and psychological support is important for early recovery and to prevent complications arising due to COVID-19 affecting the mother and foetal health. In acute care setup, physiotherapy helps with non-invasive support, postural changes, mobilization as well as weaning from mechanical ventilator support [6]. Physiotherapy interventions optimize oxygenation by improving alveolar ventilation, ventilation-perfusion mismatch, mucociliary clearance [7].
Case Presentation
A 33-year-old, graduate woman, in her 24th week of gestation, G2P1L1 (gravida, para, living) with normal BMI had exposure to COVID-19 positive neighbour and started experiencing breathlessness on walking short distances which worsened in a span of next 5 days. She was tested for RT-PCR which gave positive report for COVID-19. As her symptoms of breathlessness worsened, she was transferred to dedicated COVID-19 Government Tertiary Health Care Hospital where on admission, her pulse rate was 100 bpm, BP 110/70 mmHg with SPO2 of 87% on room air. Owing to low level of SPO2 she was kept under observation in the ICU with bag and mask ventilation (15 L/min). Refer (Tables 1 & 2) for summary of laboratory investigations.
Table 1: Summary of laboratory investigations.
|
Investigations |
Values |
Interpretation |
|
Haemoglobin |
12g/dl |
Borderline Normal |
|
Interleukin- 6 |
22 pg/ml |
Increased |
|
D-dimer levels |
18.8 μg/ml |
Increased |
|
Ferritin levels |
1475 ng/ml |
Increased |
|
RT-PCR (1st day of admission) |
Positive |
Positive for COVID 19 |
|
RT-PCR (9th day of admission) |
Negative |
Negative for COVID 19 |
Table 2: Arterial Blood Gas Analysis Reports from the date of admission till discharge show improvement in patient’s hypoxaemia and degree of ARDS.
|
Day |
Day 1 |
Day 6 |
Day 10 |
Day 12 |
|
O2 status |
BMV 15L/min |
BiPAP FiO2 80% |
BMV 10 L/min |
BMV 5 L/min |
|
pH |
7.396 |
7.418 |
7.422 |
7.407 |
|
PCO2 (mmHg) |
40.6 |
40.5 |
39 |
38 |
|
HCO3 (mmol/L) |
24 |
25.5 |
26.2 |
25.1 |
|
PO2 (mmHg) |
54.4 |
76 |
142 |
143 |
|
SPO2 (%) |
87.8 |
100 |
99 |
99.3 |
|
PaO2/FiO2 |
62 |
127 |
152 |
238 |
Table 3: Physiotherapy management from 1st day of physiotherapy till discharge.
|
Physiotherapy Treatment Day |
1 |
2 |
3 |
4-9 |
10 |
11 |
12 |
13 |
14 |
|
|
O2 Supply |
BMV 15 L/min |
BMV 10 L/min |
BMV 15 L/min |
BiPAP FiO2 80% |
BMV 10 L/min |
BMV 8 L/min |
BMV 5 L/min |
BMV 2L (Weaning Trials) |
Off sup. O2 |
|
|
Pulse Rate |
Pre |
99 |
114 |
108 |
Range 92-104 |
112 |
122 |
105 |
120 |
128 |
|
Post |
98 |
128 |
128 |
Range 98-110 |
114 |
120 |
120 |
121 |
120 |
|
|
SPO2 |
Pre |
98 |
100 |
100 |
100 |
100 |
100 |
100 |
100 |
100 |
|
Post |
100 |
94 |
98 |
100 |
100 |
100 |
100 |
100 |
100 |
|
|
Positioning |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
Relaxation |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
Breathing Exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
In-bed exercise |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
Sitting exercises |
N |
Y |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Standing |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Balance exercises in Standing |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Spot Marching |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Walking |
N |
N |
N |
N |
N |
N |
N |
Y |
Y |
|
Y: Yes; N: No; BMV: Bag and Mask Ventilation; BiPAP: Bilevel Positive Airway Pressure; O2: Oxygen; SPO2: Saturation of oxygen in blood; L/min: litres/minute; m: meters; FiO2: Fraction of oxygen; sup: supplementary.
Her medical management comprised of medications namely Inj. Piptaz (Broad- spectrum antibiotics), Inj. Low Molecular Weight Heparin (anticoagulant), Inj. Methylprednisolone (immunosuppressant) along with Oxygen Therapy (BiPAP, Bag and Mask followed by Nasal Cannula). She was referred for physiotherapy on the second day of admission. She was conscious, co-operative and oriented to time, place, and person. She complained of breathlessness at rest, fatigue (RPE:3; modified Borg Scale), and dizziness while sitting. Her pulse rate was 98 bpm and SPO2 99 percent. The patient had tachypnoea with increased work of breathing as accessory muscle work was evident. Prior to physiotherapy treatment, vital parameters were checked, and physiotherapy intervention (Table 3) was implemented as per our institutional COVID-19 physiotherapy guidelines [6].
Discussion
COVID-19 has infected more than 14 million people worldwide and resulted in mortality of more than 6 million people and still counting (as reported on 20th July 2020) [1]. It has spared no one, affecting people of all age groups and medical conditions including pregnancy. Pregnancy is a dynamic process associated with tremendous physiological, anatomical and psychological changes. Changes in the cardiovascular and respiratory system include increased heart rate, reduction in blood pressure (leading to the feeling of dizziness during prolonged standing); increase in respiratory rate, tidal volume, oxygen consumption and reduced chest excursion leading to hyperventilation causing dyspnoea. These changes along with reduced immune response make them physiologically more susceptible to severe COVID-19 infection requiring Intensive care [4, 5, 8, 9]. Holistic approach for the successful treatment of COVID-19 is important to alleviate patients from physical, and psychological stress to promote early recovery by reducing hospital stay, improving functional independence and quality of life, in turn reducing mortality and morbidity.
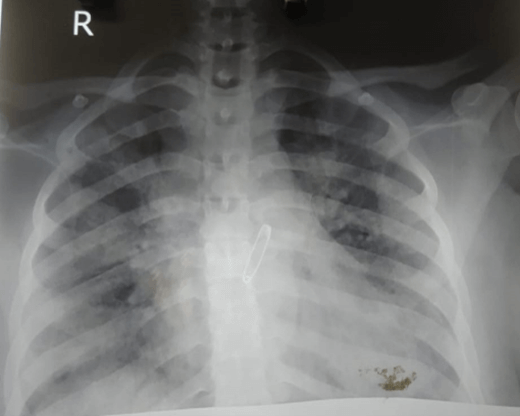
Figure 1: Anteroposterior view of chest X-ray shot on 1st day of hospitalization.
This report illustrates the management of a 24-week pregnant woman with severe symptoms of COVID-19 through combined efforts of multidisciplinary medical team at our dedicated COVID-19 Government Tertiary Care Hospital. The patient was admitted to the ICU as she was experiencing grade 4 breathlessness (mMRC) and was unable to maintain her oxygen saturation. Her ABG report was suggestive of moderate hypoxemia with severe ARDS (refer Table 2). Her X-ray showed reduced air entry, patchy ground glass opacities predominant in B/L middle and lower zones; asymmetric in apparency; right more than left, obliteration of cardiophrenic and costophrenic angles bilaterally (Figure 1).
She was diagnosed with COVID-19 pneumonia and ARDS with type 1 respiratory failure. At the time of hospitalisation, she was in a lot of mental stress and anxiety due to unpredictability of the course of disease, social stigma, lack of knowledge and myths about COVID-19. The social media had only added to this stress. She was worried about being hospitalised, away from her husband and four-and-a-half-year-old son, and future of the unborn child. She and her husband were counselled by the medical team and she was started with a medical regime which included medications and oxygen therapy. During the patient education and relaxation session we were able to redirect her fear and achieve a positive outlook by constant communication, discussing the line of management, pros and cons of treatment, her improvement in condition and hence giving her hope for the future. She was motivated and co-operative with the treatment protocol and was going an extra mile to recover early, protect her unborn child and to reunite with her son at home.
Our primary physiotherapy goal was to reduce dyspnoea, improve oxygenation, early weaning from oxygen support, and prevention of ICU related complications like ICU acquired weakness (ICUAW). As per COVID awake repositioning/ proning protocol (CARP), patient was given upright sitting (60-90) positioning, left and right recumbent positioning for 30 minutes and was asked to perform it every 2 hours [10]. Taking pregnancy into consideration, prone positioning was not given rather one quarter turn from prone was given which was more comfortable for the patient. Positioning helped in improving oxygenation. Dyspnoea relieving position with pursed lip breathing was given to relax the thorax and accessory muscles. Her husband made sure via telecommunication she was following it every 2 hourly and kept motivating and supporting her throughout the treatment. Patient was taught breathing exercises which included diaphragmatic breathing, thoracic expansion exercises and lateral chest expansion in side-lying to improve ventilation, reduce tachypnoea and to help alleviate stress and anxiety.
In anticipation of increase in oxygen demand during exercise, oxygen levels were increased prior to the physiotherapy session to prevent desaturation [6]. Vitals were monitored continuously, and adequate rest pauses were given. As her resting heart rate was always on the higher side more focus was given on adequate rest pauses between consecutive exercises. In-bed exercises comprising of ankle toe movement, heel slides, finger pumping, pelvic rotations were given to prevent complications arising from immobility. Shoulder shrugs and shoulder rotations were given to relax the thorax and the shoulders (5-10 repetitions each).
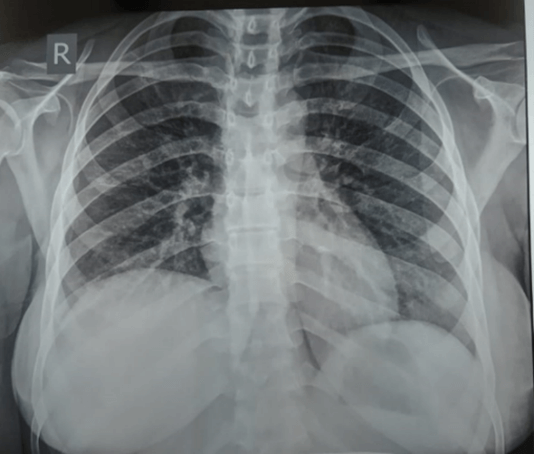
Patient was gradually taken into sitting in bed without support followed by bedside sitting wherein dynamic quadriceps, neck range of motion exercises, trunk rotations, and perturbations were given. This was progressed to standing, balance exercises in standing which included rotation and side-stepping to improve balance and reduce risk of fall. Spot marching was started, progressing from 1 set of 15 repetitions to 3 sets of 15 repetitions with sufficient rest-pauses. On the last day of hospitalization, patient was able to ambulate 3 rounds of 15 meters without supplementary oxygen maintaining normal oxygen saturation and RPE of 1.5 on modified Borg Scale. Improvement in her health condition can be seen objectively through her ABG and X-ray reports (Table 2 & Figure 2).
Figure 2: Portable chest X-ray shot on the 2nd last day of hospitalization. The X-ray suggests resolving ARDS and an overall improvement in the air entry.
She was discharged after she was able to maintain oxygen saturation on room air. After discharge patient is followed up via telecommunication; currently she experiences breathlessness on strenuous activity, for which dyspnoea relieving positions along with pursed lip breathing has been taught. Her SPO2 at rest ranges between 97-99% monitored by herself at home using a pulse oximeter. She experiences fatigue after standing for more than 10 minutes and on stair climbing. She is able to manage all her ADLs, household chores and is taking care of her 4-and-a-half-year-old son and herself with ease. Her QOL-Grav questionnaire score is 15 out of the total score of 45, which suggests excellent quality of life in pregnant women [11]. Thus, challenge of managing COVID-19 in a pregnant woman was successfully tackled by a multidisciplinary team of experts which helped her to go back to the society with better quality of life.
Abbreviations
COVID-19: Coronavirus Disease-19
WHO: World Health Organisation
CDC: Centers for Disease Control and Prevention
MMWR: Morbidity and Mortality Weekly Report
ICU: Intensive Care Unit
MMRC: Modified Medical Research Council
ABG: Arterial Blood Gas
BMI: Body Mass Index
BMV: Bag and Mask Ventilation
BiPAP: Bilevel Positive Airway Pressure
HR: Heart Rate
BP: Blood Pressure
RPE: Rating of Perceived Exertion
SPO2: Oxygen saturation in the blood
O2: Oxygen
ARDS: Acute Respiratory Distress Syndrome
ICUAW: ICU Acquired Weakness
CARP: COVID Awake Repositioning Protocol
g/dl: Gram/decilitre
ng/ml: Nanogram/millilitre
pg/ml: Picogram/millilitre
μg/ml: Microgram/millilitre
L/min: Litres/min
Inj.: Injection
PCO2: Partial Pressure of Carbon Dioxide
HCO3: Bicarbonate
PaO2: Partial Pressure of Oxygen
FiO2: Fraction of Inspired Oxygen
ADLs: Activities of Daily Living
mmHg: Millimetre of Mercury
mmol/L: Millimoles per Litre
IUGR: Intra Uterine Growth Retardation
G P L: Gravida, Para, Living
Bpm: Beats per minute
B/ L: Bilaterally
QoL: Quality of Life
Conflicts of Interest
None.
Funding
None.
Acknowledgements
The authors acknowledge Dr. Mohan Joshi (Dean) for allowing us to carry out this study, Dr. Hetal Mistry and Dr. Rachna Arora (Assistant Professor, Physiotherapy School and Centre) for assistance in editing and reviewing, Dr. Rakesh Bhadade (Associate Professor, Department of Internal Medicine), Patient whose information was used, All Postgraduate Students, Faculty and Staff Members of Physiotherapy School & Centre, T.N.M.C & B.Y.L Ch Nair Hospital.
Ethical Approval
Our institution, Topiwala National Medical College and B. Y. L. Nair Ch. Hospital does not require ethical approval for reporting individual cases or case series.
Consent
Written informed consent was obtained from the patient for their anonymized information to be published in this article.
Author Contributions
|
|
CV Verma |
GS Jere |
SK Patel |
R Desouza |
|
Concepts |
ü |
NA |
NA |
NA |
|
Design |
ü |
NA |
NA |
NA |
|
Definition of intellectual content |
ü |
ü |
ü |
NA |
|
Literature search |
ü |
ü |
ü |
NA |
|
Clinical studies |
ü |
ü |
ü |
ü |
|
Experimental studies |
NA |
NA |
NA |
NA |
|
Data acquisition |
ü |
ü |
ü |
ü |
|
Data analysis |
ü |
ü |
ü |
ü |
|
Statistical analysis |
NA |
NA |
NA |
NA |
|
Manuscript preparation |
ü |
ü |
ü |
NA |
|
Manuscript editing |
ü |
ü |
ü |
NA |
|
Manuscript review |
ü |
ü |
ü |
ü |
|
Guarantor |
ü |
NA |
NA |
NA |
|
Approved manuscript for publishing |
ü |
ü |
ü |
ü |
Article Info
Article Type
Case ReportPublication history
Received: Sat 08, Aug 2020Accepted: Tue 22, Sep 2020
Published: Fri 27, Nov 2020
Copyright
© 2023 Chhaya V. Verma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GCCR.2020.01.04
Author Info
Chhaya V. Verma Gayatri S. Jere Suresh K. Patel Rosemarie Desouza
Corresponding Author
Chhaya V. VermaPhysiotherapy School & Centre, TN Medical College & BYL Nair Ch. Hospital, Mumbai, India
Figures & Tables
Table 1: Summary of laboratory investigations.
|
Investigations |
Values |
Interpretation |
|
Haemoglobin |
12g/dl |
Borderline Normal |
|
Interleukin- 6 |
22 pg/ml |
Increased |
|
D-dimer levels |
18.8 μg/ml |
Increased |
|
Ferritin levels |
1475 ng/ml |
Increased |
|
RT-PCR (1st day of admission) |
Positive |
Positive for COVID 19 |
|
RT-PCR (9th day of admission) |
Negative |
Negative for COVID 19 |
Table 2: Arterial Blood Gas Analysis Reports from the date of admission till discharge show improvement in patient’s hypoxaemia and degree of ARDS.
|
Day |
Day 1 |
Day 6 |
Day 10 |
Day 12 |
|
O2 status |
BMV 15L/min |
BiPAP FiO2 80% |
BMV 10 L/min |
BMV 5 L/min |
|
pH |
7.396 |
7.418 |
7.422 |
7.407 |
|
PCO2 (mmHg) |
40.6 |
40.5 |
39 |
38 |
|
HCO3 (mmol/L) |
24 |
25.5 |
26.2 |
25.1 |
|
PO2 (mmHg) |
54.4 |
76 |
142 |
143 |
|
SPO2 (%) |
87.8 |
100 |
99 |
99.3 |
|
PaO2/FiO2 |
62 |
127 |
152 |
238 |
Table 3: Physiotherapy management from 1st day of physiotherapy till discharge.
|
Physiotherapy Treatment Day |
1 |
2 |
3 |
4-9 |
10 |
11 |
12 |
13 |
14 |
|
|
O2 Supply |
BMV 15 L/min |
BMV 10 L/min |
BMV 15 L/min |
BiPAP FiO2 80% |
BMV 10 L/min |
BMV 8 L/min |
BMV 5 L/min |
BMV 2L (Weaning Trials) |
Off sup. O2 |
|
|
Pulse Rate |
Pre |
99 |
114 |
108 |
Range 92-104 |
112 |
122 |
105 |
120 |
128 |
|
Post |
98 |
128 |
128 |
Range 98-110 |
114 |
120 |
120 |
121 |
120 |
|
|
SPO2 |
Pre |
98 |
100 |
100 |
100 |
100 |
100 |
100 |
100 |
100 |
|
Post |
100 |
94 |
98 |
100 |
100 |
100 |
100 |
100 |
100 |
|
|
Positioning |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
Relaxation |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
Breathing Exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
In-bed exercise |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|
|
Sitting exercises |
N |
Y |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Standing |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Balance exercises in Standing |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Spot Marching |
N |
N |
N |
N |
Y |
Y |
Y |
Y |
Y |
|
|
Walking |
N |
N |
N |
N |
N |
N |
N |
Y |
Y |
|
Y: Yes; N: No; BMV: Bag and Mask Ventilation; BiPAP: Bilevel Positive Airway Pressure; O2: Oxygen; SPO2: Saturation of oxygen in blood; L/min: litres/minute; m: meters; FiO2: Fraction of oxygen; sup: supplementary.
References
- World Health Organisation Corona Virus disease 2019 (COVID 19).
- Government of India Ministry of Health & Family Welfare Directorate General of Health Services (EMR Division); Clinical Management Protocol: COVID-19; Version 3, 13th June 2020.
- ICMR - National Institute for Research in Reproductive Health. Guidance for Management of Pregnant Women in COVID-19 Pandemic; 14th April 2020.
- Dashraath P, Wong JLJ, Lim MXK, Lim LM, Li S et al. (2020) Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol 222: 521-531. [Crossref]
- Ellington S, Strid P, Tong VT, Woodworth K, Galang RR et al. (2020) Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status – United States, January 22-June 7, 2020. Morbidity and Mortality Weekly Report 69: 769-775.
- Verma CV, Arora RD, Shetye JV, Karnik ND, Patil PC et al. (2020) Guidelines of physiotherapy management in acute care of COVID-19 at dedicated COVID center in Mumbai. Physiotherapy 14: 55-60.
- Dean E, Dean E (1994) Oxygen transport: a physiologically-based conceptual framework for the practice of cardiopulmonary physiotherapy. Physiotherapy 80: 347-354.
- Margaret Polden, Jill Mantle (2007) Physiotherapy in Obstetrics and Gynaecology. New Delhi: Jaypee Publication; Ch. 2: Physiology of Pregnancy 2: 33-34.
- Lee SY, Chien DK, Huang CH, Shih SC, Lee WC et al. (2017) Dyspnea in pregnancy. Taiwan J Obstet Gynecol 56: 432-436. [Crossref]
- COVID Awake Repositioning Protocol (CARP). Resuscitation & Acute Critical Care, Janus General Medicine; Version 1, 6th April 2020.
- Vachkova E, Jezek S, Mares J, Moravcova M (2013) The evaluation of the psychometric properties of a specific quality of life questionnaire for physiological pregnancy. Health Qual Life Outcomes 11: 214. [Crossref]
