Common Jejunal Tract Intussusception into the Jejuno-Jejunal Anastomosis as Long-Term Complication after near Total Gastrectomy for Distal Gastric Cancer
A B S T R A C T
Background: Intussusception is a rare complication after Roux-en-Y gastric bypass (RYGB) and extremely rare after near total gastrectomy.
Case Presentation: 46-years-old woman (BMI=40 kg/m2, co-morbidity: hypertension) operated about seven months before of near total gastrectomy (for distal gastric cancer) with a small bowel resection with Roux and Y gastric reconstruction , presented epigastric pain after meals, alvus alterations lasting by a week, vomiting in the last days with leukocytosis and transaminase and amylase increase. The CT scan showed peri-hepatic fluid, gastric, duodenal and jejunal dilatation, a "target like imagine" of jejuno-jejunal anastomosis with small bowel air-fluid levels, normal intestinal loop downstream the jejuno-jejunal anastomosis. During laparoscopy we discovered ischemia of common jejunal tract intussuscepted into the jejuno-jejunal anastomosis. The common ischemic intestinal tract and the anastomosis were resected “en-bloc” and jejuno-jejunal anastomosis was performed again.
Conclusion: The symptoms of small bowel intussusception after near total gastrectomy are not specifics but the risk of severe complications requires an early diagnosis and treatment. According to literature data, CT-scan is the gold standard for the diagnosis but in unclear cases it is mandatory an early laparoscopic exploration to confirm the clinical suspicion and to perform the appropriate treatment.
Keywords
Near total gastrectomy, small bowel intussusception intestinal ischemia, bowel obstruction, gastric cancer
Background
Adult intussusception is uncommon, making up only 5% of total cases of intussusception and accounting for 1-5% of adult intestinal bowel obstructions . Tumors cause the majority of adult intussusception (benign 25% and malignant 27.3%). Other causes include inflammatory bowel disease and anatomic abnormalities, such as the Meckel’s diverticulum or the mobile caecum [1]. Intussusception after near total gastrectomy is a rare cause of intussusception, with an increasing incidence [2, 3]. It is usually associated with lesions defined “lead point”, such as cancer, polyps, adhesion it is defined anterograde or retrograde by isoperistaltic or antiperistaltic behavior of the intestinal loop intussuscepted [4-14]. Its pathophysiology after near total gastrectomy is still unclear. Due to the rapid increase in the rate of bariatric surgery, intussusception is becoming an increasingly emergent post-operative complication, also post-laparoscopic Roux en Y gastric bypass (LGBP) [9]. It usually develops one year after a laparoscopic gastric intervention with Roux en Y reconstruction, predominantly in females after an important weight loss [6, 8, 15]. The symptoms (abdominal pain, nausea and vomiting) are unspecific and are common to the other causes of intestinal obstruction such as internal hernia, [5, 8, 15-18]. CT scan with contrast is highly recommended, with a specificity of 80% reported in the literature [1, 2, 5, 9, 19]. It has not yet been established what is (resection or reduction) the best treatment for intussusception after near total gastrectomy, anyway surgical exploration is highly recommended in the literature [18].
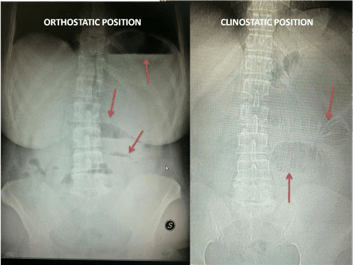
Figure 1: Abdomen Rx shows gastro-duodenal and jejunal dilatation with air-fluid levels.
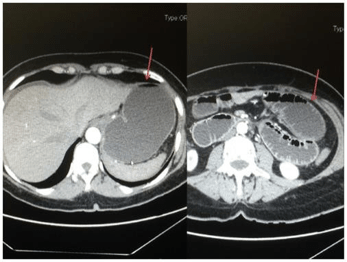
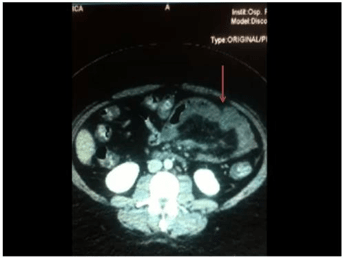
Figure 2: CT scan shows gastric-stump and jejunal distention and perihepatic fluid.
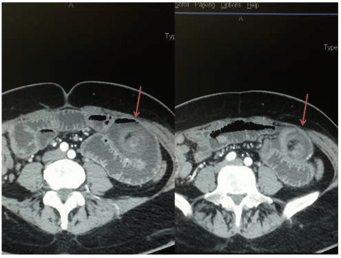
Figure 3: CT scan shows the “target sign” of intestinal intussusception.
Case Presentation
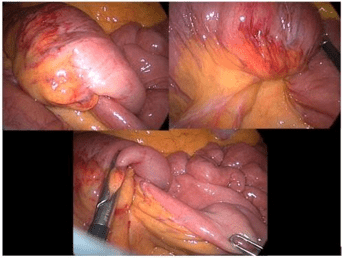
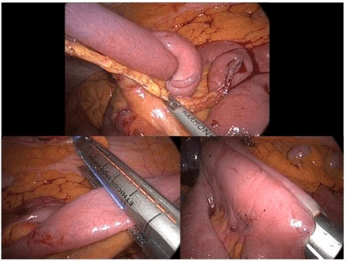
We performed a near total gastrectomy for distal gastric cancer in a 46- years-old woman. She had a BMI of 40 kg/m2 and reported an history of hypertension, urinary stress incontinence, hiatal hernia, reflux esophagitis, previous tonsillectomy and a caesarean section. The follow- up was regular until the seventh month after the intervention when she presented post-prandial epigastric pain, alvus alterations and vomiting in the last day. For these reasons she was readmitted in our center. The patient was apyretic, presented normal vital parameters and an important weight loss (33 kg). The physical abdomen examination showed an intestinal distention, pain at deep palpation in the left side but no signs of peritoneal irritations. Blood tests showed leucocytosis, slight alteration of transaminases and amylases. The Abdomen-RX showed gastric, duodenal and jejunal dilatation with small bowel air-fluid levels abdominal CT scan showed peri-hepatic fluid and signs of intussusception at the level of jejuno-jejunal anastomosis with distention of the upstream loops and stomach with air-fluid levels (Figure 1-3). The patient was immediately treated by laparoscopy. The abdominal exploration did not show internal hernias, but we found the ischemia of common jejunal tract intussuscepted into the jejuno-jejunal anastomosis (retrograde intussusception) producing an occlusion of biliary and alimentary intestinal tract (Figure 4). The anastomosis was resected “en- bloc” with common ischemic ileal tract and the jejuno-jejunal anastomosis was performed again with a temporary gastrostomy (Figure 5). The postoperative course was regular with progressive removal of abdominal drains and gastrostomy closure after the canalization. The patient was discharged in the 10th post-operative day and the 12th month follow-up was regular, except for an incisional supraumbelical hernia.
Figure 4: Laparoscopic exploration shows a not reducible intussusception.
Figure 5: Intussuscepted anastomosis laparoscopic resection and jejuno- jejunal re-anastomosis.
Discussion
According to the literature intussusception is a rare disease in adults, with an incidence of 1-5%[1]. It may be primitive or secondary, in particular it may be a surgical complication with a percentage of 0.06- 1,2% [5, 6, 8, 15, 19]. Intussusception is anterograde or retrograde according with the direction of peristalsis: isoperistaltic or antiperistaltic [7, 11-14, 20, 21]. There are four theories in literature to explain the onset of a post Roux -En-Y jejunal reconstruction intussusception. Stephenson et al. in their review of literature, deemed that a rapid weight loss associated with a thinning of the mesentery may cause retrograde peristalsis [22]. We would emphasize there is a predisposition of women to intussusception at the nadir of their weight loss. The second theory supports the presence of lead point promoting intussusception such as the suture line or adhesions or lymphoid hyperplasia [4, 5, 19, 23]. Hocking et al. performed manometric studies on the Roux limb, finding peristalsis alterations that may explain the onset of retrogade intussusception [24]. Karlstrom et al. performed furher studies on dogs submitted to vagotomy and Roux gastrectomy, analizing myoelectric activity and founding an ectopic pacemaker that produces retrograde peristalsis [25].
Figure 6: CT scan shows an early intestinal intussusceptions with the “telescope sign”.
Currently authors agree on a multifactorial etiology that includes all these four theories [3, 18]. Generally, intussusception presents a symptomatic triad, especially in children, characterized by: abdominal pain, red-currant jelly stool and palpable mass. The symptoms of intussusception after near total gastrectomy are aspecific; the most reported symptoms in the literature are: intermittent acute or chronic abdominal pain without a peritoneal reactivity, nausea, vomiting [5, 8, 11, 16, 17, 18]. Daellenbach emphasizes that in the intussusception of biliopancreatic tract the patient does not complain any symptoms of a bowel obstruction, but reports abdominal pain, increased pancreatic and bile enzymes, associated with tachycardia or hypotension if there is intestinal ischemia [6]. Our patient had an exacerbation of the symptoms characterized by the appearance of vomiting and an alteration of transaminases and amylases, according to the Literature but without specific symptoms of intussusception. All Authors agree with the importance of the CT-scan as the gold standard for the diagnosis with an accuracy of 80% [4, 5, 14, 17, 26]. CT specific signs are: “target” imagine which confirms the presence of bowel wall intussuscepted inside the tract that appears expanded the “telescope” sign when the intussuscepted bowel seems a telescope into the adjacent distal intestinal loop (Figure 3 & 6) [27-28]. In this case we performed both X-ray and CT scan.The X ray of the abdomen only showed the intestinal dilatation. On the contrary the subsequent contrast CT-scan showed both signs of intussusception and a dilatation of the small intestine with peri-hepatic fluid due to the loop suffering, so we proceeded to early surgery.
Currently, there is no consensus on definitive treatment for intussusception post- near total gastrectomy. It may include the simple intussusception reduction with or without the plication and the anastomotic resection with intestinal stump re-anastomosis [5, 6, 15]. Manual reduction with or without plication/pexy procedure has been described in many studies [3, 29, 30]. The resection must be conducted when there are signs of bowel necrosis. According to some studies the resection has statistically lower recurrence rates compared to manual reduction (7.7% versus 31.5%) [31]. Simper reported a 100% intussusception recurrence in patients only treated by the reduction, suggesting the need of performing a resection with the repair of the intussuscepted tract. [32]. Daellenbach supports this theory emphasizing the importance of the resection to remove the lead point, as the staple line, and also reports a 33.3% of recurrences in patients who underwent only to loop reduction with or without plication versus 7.7% in patients with loop resection. [6]. Stephenson on the contrary supports the reduction with the plication and Varban sustains that a conservative approach can reduce postoperative complications compared to a single case of relapse reported in his own series which however has a mean follow-up of 9 months [18, 22]. These two types of intervention may be conducted by open or laparoscopic tecnique depending on surgeon’s expertice and skill [6, 18].
In our patient, the laparoscopy showed an intestinal ischemia so the bowel resection with redo-anastomosis was mandatory. In conclusion the intussusception may be a rare complication after near total gastrectomy and predominantly affects females with an high weight loss. Diagnosis is difficult and should be supported by CT. In literature the etiology and the best treatment are still discussed although recently most studies recommend in all cases the intestinal resection with anastomosis’s remaking [6, 8, 9, 15, 16, 17, 31].
Conclusion
The intestinal intussusception is a rare complication not only of near total gastrectomy but also of other types of gastric interventions requiring a Roux en Y jejunal reconstruction. The symptoms of small bowel intussusception after near total gastrectomy are not specifics and could be underestimated or confused with other benign pathologies but the risk of severe complications requires an early diagnosis and treatment. Recurrent pain, nausea, vomiting and diarrhea in patients with an history of near total gastrectomy could induce the suspicion of intestinal intussusception (or other mechanical causes of subocclusion as internal hernia). According to the Literature, CT-scan is the gold standard for the diagnosis showing specific "signs" of intussusception. In some cases, the diagnosis is unclear, and it must be obtained by laparoscopy: a high index of suspicion of mechanical subocclusion at physical examination especially in bariatric patients is enough for an early laparoscopic exploration and treatment. We recommend an early laparoscopic exploration to also confirm the diagnosis and to decide about the appropriate treatment infact in case of not reducible intussusception or ischemic intestinal loop, the resection and redo-anastomosis are mandatory.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Thu 19, Dec 2019Accepted: Fri 27, Dec 2019
Published: Mon 20, Jan 2020
Copyright
© 2023 Massimiliano Fabozzi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2019.01.07
Author Info
Angelo Gragnaniello Ferdinando Amodio Francesco Corcione Mafalda Romano Massimiliano Fabozzi Pia Cirillo Rosa Murano
Corresponding Author
Massimiliano FabozziUnit of General and Oncological Surgery ( Chief: M.FABOZZI,MD,PhD), “A. Tortora” Pagani Hospital, Italy
Figures & Tables
References
- Valentini V, Buquicchio GL, Galluzzo M, et al. (2016) Intussusception in adults: The role of MDCT in the identification of the site and cause of obstruction. Gastroenterol Res Pract 2016: 5623718. [Crossref]
- Honore M, Chiow AKH, Bryant R (2017) Retrograde intussusception post Roux-en-Y gastric bypass. ANZ J Surg 87: 518-520.
- Boudourakis LD, Divino C, Nguyen S (2013) Retrograde intussusception seven years after a laparoscopic Roux-en-Y gastric bypass. J Minim Access Surg 9: 82-83. [Crossref]
- Kasotakis G, Sudan R (2009) Retrograde intussusceptions after Roux- en-y gastric bypass for morbid obesity. Obes Surg 19: 381-384. [Crossref]
- Zainabadi K, Ramanathan R (2007) Intussusceptions after Roux-en-y gastric bypass. Obes Surg 17: 1619-16232.
- Daellenbach L, Suter M (2011) Jejunojejunal intussusception after Roux-en-Y gastric bypass: a review. Obes Surg 21: 253-263. [Crossref]
- O'Connor DB, Ryan R, O'Malley D, Macdermott E (2012) Retrograde intussusception 5 years after Roux-en-Y gastric bypass for morbid obesity. Ir J Med Sci 181: 419-421. [Crossref]
- Lo Menzo E, Stevens N, Kligman M (2010) Plication followed by resection for intussusception after laparoscopic gastric bypass. Surg Obes Relat Dis 6:563-565. [Crossref]
- McAllister MS, Donoway T, Lucktong TA (2009) Synchronous intussusceptions following Roux-en-Y Gastric Bypass: case report and review of the literature. Obes Surg 19: 1719-1723. [Crossref]
- Goverman J, Greenwald M, Gellman L, Gadaleta D (2004) Antiperistaltic (retrograde) intussusception after Roux-en-Y gastric bypass. Am Surg 70: 67-70.
- Kasotakis G, Sudan R (2009) Retrograde intussusception after Roux- en Y gastric bypass for morbid obesity. Obes Surg 19: 381-384. [Crossref]
- Pauli EM, Haluck RS (2008) Antiperistaltic (retrograde) intussusception after laparoscopic Roux-en-Y gastric bypass procedure. Surg Obes Relat Dis 4: 567-568. [Crossref]
- Hocking MP, McCoy DM, Vogel SB, Kaude JV, Sninsky CA (1991) Antiperistaltic and isoperistaltic intussusception associated with abnormal motility after Roux-en-Y gastric bypass: A case report. Surgery 110: 109-112. [Crossref]
- Gopal R, Elamurugan TP, Hage S, Muthukumarassamy R, Kate V (2014) Retrograde jejunogastric intussusception following Braun's jejunojejunostomy. World J Clin Cases 2: 24-26. [Crossref]
- Edwards M, Grinbaum R, Ellsmere J, Jones D, Schneider E (2006) Intussusceptions after Roux-en-y gastric bypass for morbid obesity: case report and literature review of a rare complication. Surgery for obesity and related diseases 2: 483-489. [Crossref]
- Lessmann J, Soto E, Merola S (2008)Intussusception after Roux-en-Y gastric bypass for morbid obesity. Surg Obes Relat Dis 4: 664-667.
- Singla S, Guenthart BA, May L, Gaughan J, Meilahn JE (2012) Intussusception after laparoscopic gastric bypass surgery: an underrecognized complication. Minim Invasive Surg 2012: 464853. [Crossref]
- Varban O, Ardestani A, Azagury D, Lautz DB, Vernon AH et al. (2013) Resection or reduction? The dilemma of managing retrograde intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis 9: 725-730. [Crossref]
- Al-Sabah S, Christou N (2008) Intussusceptions after laparoscopic Roux-en-y gastric bypass. Surgery for obesity and related diseases 4: 205-209.
- Efthimiou E, Court O, Christou N (2009) Small bowel obstruction due to retrograde intussusception after laparoscopic Roux-en-Y gastric bypass. Obes Surg 19: 378-380. [Crossref]
- Coster DD, Sundberg SM, Kermode DS, Beitzel DT, Noun SH et al. (2008) Small bowel obstruction due to antegrade and retrograde intussusception after gastric bypass: three case reports in two patients, literature review, and recommendations for diagnosis and treatment. Surg Obes Relat Dis 4:69-72. [Crossref]
- Stephenson D, Moon RC, Teixeira AF, Jawad MA (2014)Intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis 10: 666-670. [Crossref]
- Duane TM, Wohlgemuth S, Ruffin K (2000)Intussusception after Roux-en-Y gastric bypass. Am Surg 66: 82-84.
- Hocking MP, McCoy DM, Vogel SB, Kaude JV, Sninsky CA (1991) Antiperistaltic and isoperistaltic intussusception associated with abnormal motility after Roux-en-Y gastric bypass: a case report. Surgery 110: 109-112. [Crossref]
- Karlstrom L, Kelly KA (1989) Ectopic jejunal pacemakers and gastric emptying after Roux gastrectomy: effect of intestinal pacing. Surgery 106: 867-871. [Crossref]
- Toso C, Erne M, Lenzlinger PM, Schmid JF, Büchel H et al. (2005) Intussusception as a cause of bowel obstruction in adults. Swiss Med Wkly 135: 87-90. [Crossref]
- Hokama A, Kinjo T, Kishimoto K, Fujita J (2014) Crescent-in- doughnut sign and telescope sign of intussusception in Peutz-Jeghers syndrome. BMJ Case Rep 2014. [Crossref]
- Srikanth MS, Keskey T, Fox SR, Oh KH, Fox ER et al. (2004) Computed tomography patterns in small bowel obstruction after open distal gastric bypass. Obes Surg 14: 811-822. [Crossref]
- Carilli S, Arisoy M, Alper A (2015) A rare complication following laparoscopic Roux & Y gastric bypass: Intussusception-case report. Springerplus 4: 603. [Crossref]
- Yoshiyama S, Toiyama Y, Ichikawa T et al. (2019) Laparoscopic diagnosis of retrograde peristalsis and intussusception in Roux-en-Y limb after laparoscopic gastrectomy: A case report. Asian J Endosc Surg 12: 171-174. [Crossref]
- Mukerji AN, Shah A, Parithivel VS (2016) Retrograde intussusception after Roux-en-Y gastric bypass. Am Surg 82: e238-e239.
- Simper SC, Erzinger JM, McKinlay RD, Smith SC (2008) Retrograde (reverse) jejunal intussusception might not be such a rare problem: a single group's experience of 23 cases. Surg Obes Relat Dis 4: 77-83. [Crossref]
