Complicated Abdominal Seat Belt Injuries in Children
A B S T R A C T
Background: The proper use of security accessories in cars has resulted in the reduction of morbidity and mortality both in adults and children. Improper use of abdominal seat belt is associated in some cases with severe abdominal injuries.
Objectives: Investigation of the treatment outcomes of children who suffered complicated abdominal seat belt injuries between 1998 and 2013.
Methods: We present five cases of children aged 6-14 years, who suffered complicated abdominal injuries due to improper use of the seat belt. Abdominal injuries included injuries to the liver, spleen, small bowel (duodenum, jejunum, and ileum), colon and aorta, mesenterial bleeding, retroperitoneal bleeding, bowel obstruction and pelvic fractures.
Results: Three children were operated on within a few hours of admission due to peritoneal irritation, hemodynamic instability after fluid resuscitation, bowel injuries including perforation and bowel ischemia. Two children who were hemodynamically stable, were operated on after few days. One of them had a diagnosis of aortic injury and the other, bowel obstruction. The first child was treated in two stages: i. repair of duodenal rupture, and ii. repair of the aortic injury by using interposition Gore-Tex graft. For the child with bowel obstruction, segmental resection and primary anastomosis were performed. The operation and postoperative periods for all children were uneventful, and all five children are healthy today.
Conclusion: 1) The abdominal seat belt should always be used in conjunction with the chest seat belt. 2) An abdominal seat belt sign should always raise the possibility of complicated abdominal injuries. 3) Gastrointestinal tract injuries are common in this setting. 4) Aortic injury is rare; however, it can easily be missed initially. 5) Abdominal aortic trauma is associated with duodenal injuries in almost all cases.
Keywords
Seat belt injuries, abdominal injuries, abdominal seat belt, aortic trauma
Introduction
The mortality of passengers in road traffic accidents is decreasing as a result of increased use of seat belts. However, the use of seat belts is associated with a unique injury profile, collectively termed seat belt syndrome (SBS) [1]. This syndrome includes injuries to the intestinal viscera, tears and perforations of the gastrointestinal tract and its mesentery, and lumbar fracture-dislocations. In some cases, lumbar spine dislocation and fractures are also associated with this profile [2]. A planned sub-analysis of a prospective study of 12,000 children with blunt torso trauma had shown a greater risk for intra-abdominal injuries in patients with a seat belt sign than in those without a seat belt sign (relative risk, 1.6), and was largely indicative of an increased risk for gastrointestinal injuries (RR, 9.4). Children with seat belt signs had an increased risk for undergoing any acute interventions (RR, 4.5), including therapeutic laparotomy (RR, 9.5) [3]. Some evidences had shown a similar trend among the adult population. Biswas S et al. reported that patients with seat belt injury who have solid-organ injury require urgent intervention. Solid-organ injuries associated with malpositioned seat belts lying higher on the abdomen tend to result in hemodynamic instability, necessitating immediate surgery. These patients have more postoperative complications and greater mortality [4]. Vincent O'Dowd et al. presented significant devascularisation injuries to the small bowel requiring emergency surgical intervention among passengers wearing a seat belt sustained [5].
These injuries are more prevalent in the pediatric population due to improper-fitting safety belts [6]. For example, García-Espana’s study demonstrated that one out of five 8-12-year-olds misused the shoulder portion of the vehicle seat belt [7]. Pickrell and Ye suggested that 2009 data designated 45% of 4-7-year-olds were not restrained in accordance with best practice recommendations for their age [8]. The preferable child protection routine during a motor ride is using an age-appropriate restraint and rear seating [9]. According to NHTSA, vehicle safety belts are considered to fit correctly when the lap portion of the belt rides low over the hips or thighs and the shoulder portion crosses the sternum and shoulder. Day-to-day survey of children safety belt use was described by CHOP study, which suggested that one-third of 8-12-year-olds was routinely seated in the car front row (CHOP 2008) [10]. In addition, some old vehicles only have a lap belt, which constrains the child in two points.
Here we describe children with complicated abdominal seat belt injuries between the years 1998-2013, diagnosis process and treatment results. This study describes five children diagnosed with SBS injuries, three males and two females, aged 6-14 years. These children suffered from complicated abdominal injuries due to the use of a lap seat belt while five different motor vehicle crashes occur. The diagnosed abdominal injuries in these cases were injuries to liver, spleen, small intestine (duodenum, jejunum, and ileum), colon and aorta, mesenterial bleeding, peritoneal bleeding, intestine obstruction and pelvic fractures.
Results
All children were rear-seat passengers wearing lap or 3-point restraints. All had abdominal lap-belt ecchymosis and multiple abdominal injuries due to the common mechanism of seat-belt compression as a result of sudden deceleration that followed car collision.
Case Analysis
Five children (three boys and two girls, ranging in age from 6-15 yrs.) involved in multiple-victim motor vehicle crashes were seen at the Galilee Medical Center. All five children arrived with an ecchymosis across the abdominal wall, which is the typical sign of the lap belt injury.
Case I
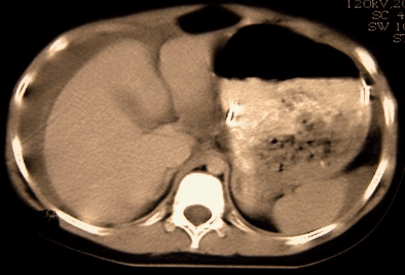
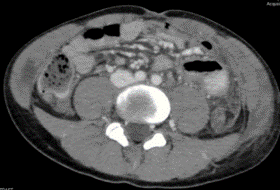
An 11-year-old girl was restrained in a lap belt of the central back seat of a private car at the time of a hard kinematics head-on collision. Two other girls, the same age were sitting from both of her sides. All other passengers were slightly injured. On admission, her Glasgow Coma Scale score was 15, and she was a little bit sleepy. Her heart rate was 111 beats/min and her blood pressure was 118/49. 27 breathings per minutes were recorded, with 100% saturation, and RTS 12. Pertinent physical findings included an area of ecchymosis at the right side of the umbilicus, abdominal distension and guarding. Her CT scan demonstrated significant amount of blood, and a pelvic fracture. In addition, a liver subcapsular hematoma was identified. Figure 1 demonstrates the CT scan of this 11-year-old girl.
Figure 1: CT scan result of 11yrs girl crash car injured. At the time of the crash, the girl was restraint by lap seat belt.
She was taken rapidly to the operating room, and an invasion of 80cm of the terminal ileum with an active mesenterial bleeding was found. At this stage, the following procedures were performed: i. ligation of the mesenterial arterial and venous vessels, ii. segmental ileal resection, and iii. end to end anastomosis. At the end of the operation, she was hospitalized in the intensive care unit for three days. After this period, she transferred to the pediatric surgical department. Today, she is 27 years old, healthy and active woman.
Case II
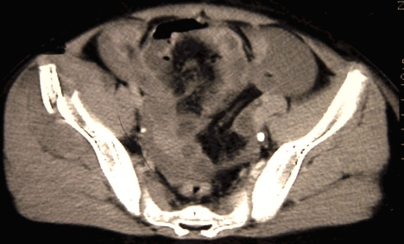
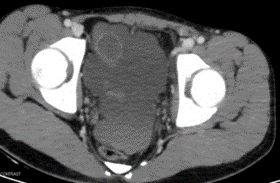
A 6 year-old-girl was restrained in a lap belt of the central back row of an old car when a crash with a 2.5t vehicle had occurred. On admission, her Glasgow Coma Scale score was 15, slightly sleepy. Her heart rate was 130beats/min and her blood pressure was 110/55. 22 breathings per minute were measured, with 100% saturation (with an oxygen mask), and RTS 12. Her VAS scale score was 4/5. Pertinent physical findings included an area of ecchymosis of the umbilicus, without abdominal distension and/or guarding. Her CT scan demonstrated low to medium amount of pelvis free fluid, clear edema of the intestinal loop no evidence for free air was found. Figure 2 demonstrates the CT scan of this 6-year-old girl.
Figure 2: CT scan result of a 6yrs girl, lap seat belt restraint crash car injured.
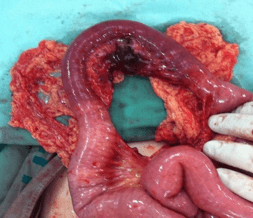
She was taken to the operating room, and jejunal mesenterial rupture was found accompanied by active bleeding. Clear signs of ischemic jejunum were found as well. This ischemic part of the small intestine was resected, followed by a primary end to end anastomosis. Figure 3 demonstrates the 6-year-old girl’s operative findings. It is important to mention that in all imaging and scans, no spine damages were found.
Figure 3: operation evidence [ 6yrs girl, lap seat belt restraint crash car injured].
On the 6th day after the operation, she was sent home. Two weeks later, she suffered from an event of partial bowel obstruction that was successfully treated by conservative treatment.
Case III
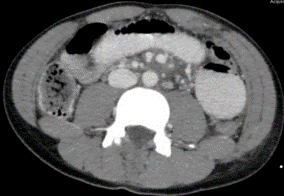
A 14-year-old boy arrived at the emergency room as a result of abdominal pain and vomiting one day prior to his complaint. This patient was hospitalized in intensive care and in our department about three days before this episode, as per his involvement in a severe car crash. The diagnosis then was blunt abdominal trauma following the car seat belt which had been shown as jejunal hematoma and a partial intestinal obstruction. According to his description, at the car crash time, he used a 3-restriction points seat belt improperly, and put the torso part of the belt under his right arm. Although he suffered from some facial injuries, he remembered the crash in detail, and didn't suffer from consciousness loss.
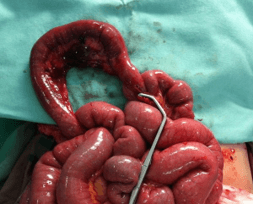
On admission, right after the accident, his Glasgow Coma Scale score was 15, his hemodynamic and respiratory parameters were stable, and he was cooperative. Pertinent physical findings included an area of ecchymosis at the umbilicus, abdominal distension and guarding. His primary CT scan evidenced a slight amount of fluid in his pelvis, without parenchymal injuries. In addition, a partial jejunal hematoma was indicated. 24 hours after the car crash, the jejunal hematoma resulted in a partial intestinal obstruction with a traumatic ileum. Figure 4 described the imaging of this patient by CT scan.
Figure 4: CT scan result of a 14yrs boy car crash injured when using improperly a 3 points seat belt restraint.
It is important to mention that all of his physiological indexes were found stable and normal. He was treated conservatively; TPN and feeding tube. On the 5th day, he was transferred to our division- drinking clear fluids with normal defecations. The TPN was completed in 24hrs and wasn't renewed. Drinking and eating were not accompanied by abdominal pain vomiting and/or nausea. On his last day in the hospital, he was walking around free. He lost 10% of his weight during hospitalization- according to his report.
Coming back to the delayed episode – he arrived in a good performance, while he lost some more weight (~2kg) during his three days staying at home. The old damaged abdominal area looks as recovered in accordance with the time period from the crash date. The stomach was thin, soft with a slight sensitivity in the upper part of it. His US scan was not optimal as per the multiplicity of the stomach and intestinal gases. A small amount of free fluid was noted in the pelvic region. The jejunal hematoma was still detected on the left side of the stomach. At this stage, conventional treatment influence was insufficient. In another set of scanning, edema and extended jejunum were noticed.
At this stage, he was transferred to the operating room. Initial laparoscopy evidenced a complicated condition in the abdomen middle-left side. Exploratory laparotomy evidenced suffered jejunum covered by omentum. This part of the jejunum was resected, followed by a primary end to end anastomosis. The rest of the intestine as well as the spleen and the liver were found normal. At the 2nd day after the operation, the feeding tube was taken out, followed by well eating and drinking. The following day he was sent home with a non-sensitive soft stomach, and a well-recovering operation scar.
Case IV
A 13-year-old boy was restrained in a lap belt of the central back row at a serious car accident. At arrival, he was conscious with a Glasgow Coma Scale score of 15, pulse 100 to 110 bpm, and blood pressure 127/55, subsequently settling to between 120–130/60 –70. A lap belt mark was present across the abdomen, which was hard and tender with signs of mild peritoneal irritation. At this stage, the child was treated by a conservative treatment procedure. On the 2nd day, an abdominal bruit was noticed, followed by a CECT that pointed out a subrenal aortic intimal flap, with narrowing of the lumen at this level and dilatation to 15 mm immediately distally. Aortography led us to place a covered stent across the injury using a combined brachiofemoral transvascular approach.
Because of the 38.5°C to 40.0°C body temperature during the next few days, he was again sent to CECT. This examination demonstrated the widening of the injured aortic segment to 17 mm with a change in the pattern of distribution of the contrast medium within the layers of the aortic wall. Due to the dynamic situation, the patient was taken to the operating room. At laparotomy on day 8, about 400 mL of old blood accompanied a transverse tear in the caudal pole of the spleen. Two small necrotic areas were noted in the mesentery close to the ligament of Treitz and to the proximal jejunum, immediately anterior to the spine. Mobilization of the duodenum uncovered an unsuspected walled-off small tear of the posterior aspect of the third part. The duodenum was closed primarily, and an Anderson tube was inserted into the jejunum.
In this case, continued monitoring by CECT showed progressive enlargement of the aneurysmal aortic segment, finally reaching 19 mm with a continuous change in the pattern of distribution of the contrast medium. Consequently, after six days of antibiotic therapy and appropriate clinical response, the abdomen was reopened, the aorta controlled and opened, and ultimately a 12-mm interposition Gore-Tex graft placed from 10 mm below the most caudal renal artery to just cranial the inferior mesenteric artery. Subsequently, a full physical recovery ensued. Almost seven years later, the patient is well and participates in sporting activities with no limitations.
Case V
A 13-year-old boy was restrained in the back row by a lap safety belt when a tough kinematics crash with a heavy vehicle had occurred. On admission, his Glasgow Coma Scale score was 15. His heart rate was 100beats/min and his blood pressure was 121/76. His hemodynamic and respiratory parameters were stable. Relevant physical findings included a safety belt sign in the lower abdomen. His stomach was soft but sensitive to touch, particularly around the lower abdomen. His abdomen CT scan demonstrated free fluid, mostly at its right side. His spleen suffered from a minimal rupture, which could not explain the free abdomen fluid. According to these findings and despite his hemodynamic stability, he was taken to the operation room with a suspect of mesenterial or jejunum injury.
During the laparotomy, the following findings were mentioned: small amount of blood, mesenterial rupture with no active bleeding, a long desaturation of the cecum (8cm- to the appendix base), another minimal rupture of the spleen (Grade I) with no active bleeding, and a small retroperitoneal stable hematoma around the right kidney. In this case, the decision of surgical intervention was principally based on our previous experience more than the physiological indexes. According to the description of the car crash, the use of a lap seat belt, and the child age- it was reasonable to assume that the car crash resulted in a compression of the lower abdomen internal organs against the lumbar spine. In this example, the surgical procedure was found required and contributed to a rapid full recovery of the patient.
Discussion
In this paper, we describe 5 cases of car crash abdominal injured children. All patients had a “seat belt sign” consisting of contusions, petechiae and a band-like pattern of abrasions across the lower abdomen. Children with abdominal injury caused by blunt trauma might have equivocal or absent physical findings. Inadequate physical functioning might develop several days after the car crash occurred. Repeated physical examinations of the abdomen are mandatory as physiological or clinical signs can be missed when the child arrives at the hospital. Furthermore, a diagnosis of hollow viscus injury in children is difficult even with CT, and only a close clinical follow-up can help identify children with these injuries [11-13]. However, we might keep in mind that CT is useful and specific in solid organ injury diagnosis but lacks sensitivity when diagnosing bowel and mesenteric injury. The exploratory laparotomy results described in this paper are with a good agreement with Breen et al. [14]. Their assessment of the diagnostic performance of CT signs in blunt abdominal and mesenteric injury was; bowel wall thickening, bowel wall discontinuity, extraluminal air, and mesenteric hematoma are all reasonably specific (84%, 95%, 100%, 94%) but not sensitive (50%, 58%, 44%, 54%). They also reported that the presence of moderate to large volume of intraperitoneal fluid without visible organ damage is an important sign [14].
All 5 cases described here demonstrate a mechanism of seat belt compression as a result of motor vehicle collision. Different intra-abdominal injuries are described, followed by different treatment protocols. Three children were operated within a few hours of admission due to peritoneal irritation, hemodynamic instability after fluid resuscitation, bowel injuries including perforation and bowel ischemia. Two children seemed to be hemodynamically stable initially. Delayed dynamic changes appeared during the hospitalization time period. These changes required surgical intervention in the described cases. The "delayed response" was diagnosed as aortic injury in one child and bowel obstruction in the second child. The aortic injury child was treated in two stages: a. repair of duodenal rupture, and b. repair of the aortic injury by using interposition Gore-Tex graft. The bowel obstruction child was treated by segmental resection and primary anastomosis. Table 1 summarizes this case report shortly.
Table 1: Abdominal Seat Belt Syndrome patients – summary.
|
Case No. |
Age Years |
Operative Findings |
Operative Treatment |
|
I |
11 |
1500 ml blood Avulsion of Ileum with active bleeding of blood vessels of mesenterium Subcapsular hematoma of liver |
Ligation of mesenterial blood vessels Segmental resection of Ileum with end to end anastomosis |
|
II |
6 |
Ischemia of Jejunal segment Mesenterial rupture with an active bleeding |
The ischemic part of the small intestine was resected followed by primary end to end anastomosis |
|
III |
15 |
Complete small bowel obstruction |
Segmetal resection of Jejunum with end to end anastomosis |
|
IV |
13 |
400 ml old blood Duodenal perforation Splenic laceration without active bleeding |
Closure of duodenal perforation |
|
Aortic injury cranial to the inferior mesenteric artery |
Repair of Aortic injury by using interposition Gore-Tex-Graft |
||
|
V |
13 |
Small amount of blood Mesentrial rupture without active bleeding Laceration of spleen - Grade 1 Retroperitoneal hematoma around the Rt Kidney |
Closure of mesenterial rupture |
In the case of a school aged car crash injuries, especially if safety belt was used – particularly in cases of two anchoring points, the physician should consider the complete spectrum of intra-abdominal injuries. Intensive care physicians must keep in mind that children are vulnerable to such injury because their gravity center is higher as compared to the adults' gravity center. This difference and the non-developed iliac crests are the main reasons behind abdomen car crash injuries in children. On time diagnosis and management of intra-abdominal injuries is critical to optimizing outcomes; thus, public health point of view might emphasize the prevention of such injuries. It is well documented that these injuries result from improper or incorrect seat belt use. Much of the literature in this regard focuses on the pediatric population, particularly with regard to the use of age-appropriate seat belts [6].
Conclusion
To the best of our knowledge, this manuscript is one of the few reports of multiple paediatric victims suffers from seat belt syndrome. The evidence described here emphasizes the importance of abdominal seat belt signs in the context of complicated abdominal injury diagnosis. The occurrence of gastrointestinal tract injuries among these cases should be considered. Rare injuries, e.g., aortic injury, can easily be missed initially. Thus, it should be noticed that abdominal aortic trauma is associated with duodenal injuries in almost all described cases. These incidents emphasize the required serious awareness of the complete spectrum of intra-abdominal injuries in restrained pediatric passengers in motor vehicle crashes. This awareness might lead to a rigorous investigation of possible injuries, even when external signs and physical indexes seem to be normal.
Article Info
Article Type
Case ReportPublication history
Received: Thu 02, Jan 2020Accepted: Sat 08, Feb 2020
Published: Mon 17, Feb 2020
Copyright
© 2023 Yechiel Sweed. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.02.03
Author Info
Alon Yulevich Gabriela Ciceu Jonathan Singer-Jordan Liat Apel-Sarid Norman Loberant Tatyana Arzumanov Yechiel Sweed Yoav Hoffmann Yuri Grozovsky
Corresponding Author
Yechiel SweedPediatric Surgery, Galilee Medical Center, Nahariya, Azrieli Faculty of Medicine, Bar-Ilan University, Israel
Figures & Tables
Table 1: Abdominal Seat Belt Syndrome patients – summary.
|
Case No. |
Age Years |
Operative Findings |
Operative Treatment |
|
I |
11 |
1500 ml blood Avulsion of Ileum with active bleeding of blood vessels of mesenterium Subcapsular hematoma of liver |
Ligation of mesenterial blood vessels Segmental resection of Ileum with end to end anastomosis |
|
II |
6 |
Ischemia of Jejunal segment Mesenterial rupture with an active bleeding |
The ischemic part of the small intestine was resected followed by primary end to end anastomosis |
|
III |
15 |
Complete small bowel obstruction |
Segmetal resection of Jejunum with end to end anastomosis |
|
IV |
13 |
400 ml old blood Duodenal perforation Splenic laceration without active bleeding |
Closure of duodenal perforation |
|
Aortic injury cranial to the inferior mesenteric artery |
Repair of Aortic injury by using interposition Gore-Tex-Graft |
||
|
V |
13 |
Small amount of blood Mesentrial rupture without active bleeding Laceration of spleen - Grade 1 Retroperitoneal hematoma around the Rt Kidney |
Closure of mesenterial rupture |




References
- Garrett JW, Braunstein PW (1962) The seat belt syndrome. J Trauma 2: 220-238. [Crossref]
- Santschi M, Echavé V, Laflamme S, McFadden N, Cyr C (2005) Seat-belt injuries in children involved in motor vehicle crashes. Can J Surg 48: 373-376. [Crossref]
- Borgialli DA, Ellison AM, Ehrlich P, Bonsu B, Menaker J et al. (2014) Association between the seat belt sign and intra-abdominal injuries in children with blunt torso trauma in motor vehicle collisions. Acad Emerg Med 21: 1240-1248. [Crossref]
- Biswas S, Adileh M, Almogy G, Bala M (2014) Abdominal injury patterns in patients with seatbelt signs requiring laparotomy. J Emerg Trauma Shock 7: 295-300. [Crossref]
- O'Dowd V, Kiernan C, Lowery A, Khan W, Barry K (2011) Seatbelt Injury Causing Small Bowel Devascularisation: Case Series and Review of the Literature. Emerg Med Int 2011: 675341. [Crossref]
- McGrath N, Fitzpatrick P, Okafor I, Ryan S, Hensey O et al. (2010) Lap belt injuries in children. Ir Med J 103: 216-218. [Crossref]
- García Espana JF, Durbin DR (2008) Injuries to belted older children in motor vehicle crashes. Accid Anal Prev 40: 2024-2028. [Crossref]
- Pickrell TM, Ye TJ (2010) The 2009 national survey of the use of booster seats. NHTSA DOT HS 811 377.
- National Highway Traffic Safety Administration (2010a) Traffic safety facts: 2009 data children. NHTSA DOT HS 811 387.
- Children’s Hospital of Philadelphia 2008 PCPS Fact and Trend Report.
- Sivit CJ, Taylor GA, Newman KD, Bulas DI, Gotschall CS et al. (1991) Safety-belt injuries in children with lap-belt ecchymosis: CT findings in 61 patients. AJR Am J Roentgenol 157: 111-114. [Crossref]
- Sherck JP, Oakes DD (1990) Intestinal injuries missed by computed tomography. J Trauma 30: 1-7. [Crossref]
- Bulas DI, Taylor GA, Eichelberger MR (1989) The value of CT in detecting bowel perforation in children after blunt abdominal trauma. AJR Am J Roentgenol 153: 561-564. [Crossref]
- Breen DJ, Janzen DL, Zwirewich CV, Nagy AG (1997) Blunt bowel and mesenteric injury: diagnostic performance of CT signs. J Comput Assist Tomogr 21: 706-712. [Crossref]
