Conservative Management of Streptococcus pyogenes Sternoclavicular Septic Arthritis
A B S T R A C T
We present a case of sternoclavicular septic arthritis (SCSA) in a 50-year-old female who presented to the emergency room with abdominal pain and vomiting after a bout of pharyngitis. Subsequent SCSA was diagnosed and treated with antibiotics. Strep pharyngitis could be a risk factor for SCSA in healthy patients, and conservative management may be adequate in treating strep A SCSA, depending on the patient’s risk factors and presentation. Our report reveals the necessity for establishing meaningful measures in staging and management to minimize risks of unnecessary harm.
Keywords
Sternoclavicular joint, conservative management, Streptococcus pyogenes
Introduction
Septic arthritis of the sternoclavicular joint is a rare but severe form of septic arthritis that may progress to life-threatening complications, including osteomyelitis, chest wall abscess, and mediastinitis [1]. SCSA is encouraged to be managed surgically due to conservative management's historically high failure rate, but the evidence is building of the sufficiency for medical treatment [1, 2]. This report illustrates the second successful report of non-operative management of SCSA caused by Streptococcus pyogenes. The Institutional Review Board (IRB) or equivalent ethics committee of the Brigham and Women's Hospital did not approve this study as the study was a report written based on a case. The subject provided informed written consent for the publication of the study data.
Case Presentation
A 50-year-old woman with a history of hypothyroidism and spondylolisthesis developed pharyngitis. Her symptoms subsided, but she began experiencing vomiting and abdominal pain and called for emergency assistance. Upon evaluation, she was febrile to 103°F and had a leukocytosis of 13,000. Her blood cultures grew Strep pyogenes. She was placed on Zosyn and Vancomycin with a transition to ampicillin.
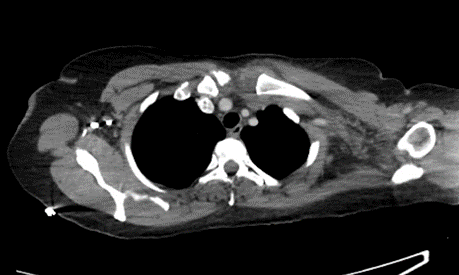
She subsequently developed severe left sternoclavicular shoulder pain, limiting movement and function, and erythema overlying the sternoclavicular joint (SCJ). Magnetic resonance imaging showed a small effusion with associated capsular thickening on the left sternoclavicular joint (Figure 1). She was transferred to Thoracic Surgery and was stable. Laboratory values were notable for CRP 95.8, ESR 92 and WBC 11,600. Repeat imaging showed unchanged small effusion without osseous erosion or other changes. Surgical interventions were deferred, and the patient was treated with IV ceftriaxone (inpatient) and PO fluoroquinolone (outpatient). She was seen in follow-up off antibiotics and was without symptoms or findings on exam. She remained symptom-free five months following her diagnosis.
Figure 1: CT image demonstrating effusion and capsular thickening of the left sternoclavicular joint.
Discussion
The most common risk factors identified for SCSA are IV drug use, end-stage renal disease, diabetes mellitus, trauma, presence of central venous line, and immunocompromised state [1]. Our case involves a 50-year-old woman with no comorbidities who developed SCSA in the setting of recent pharyngitis. Her presentation was similar to the antecedent case report of Strep pyogenes SCSA: both patients were previously healthy with a history of recent pharyngitis presenting with an isolated sternoclavicular joint infection found on CT [3]. Although less known, strep pharyngitis may be a risk factor for strep SCSA in otherwise healthy patients.
Because SCJ is a diarthrodial synovial joint surrounded with heavy ligaments and a capsule serving as a walled bacterial nidus, en-bloc resection of the SCJ and ipsilateral pectoralis major muscle flap is considered the gold-standard of treatment [1]. We opted for conservative management, referring to the literature and considering factors such as our patient’s clinical stability, high baseline performance status, no erythema, edema, and warmth on physical examination, and isolated monoarthritis infection [3].
Antibiotics for SCSA are recommended for an average duration of 5.5 weeks for intravenous antibiotics and ten weeks of oral antibiotics postoperatively [4]. The antibiotic regimen for our patient consisted of a four-week regimen of IV ceftriaxone (inpatient) followed by PO Levofloxacin (outpatient). The patient’s clinical course was followed carefully, and she recovered well. The patient showed signs of complete remission on her subsequent visits.
Unnecessary surgical procedures may place patients at risk for complications, extended hospital stay, pain, and disfigurement. In our patient, factors such as lack of comorbidities, type of pathogen (strep A), and the limited extent of the infection likely accounted for her successful outcome. In those patients without significant complications from Strep pyogenes SCSA, conservative non-operative therapy may be more favourable.
Conclusion
We present the second reported case of successful medical management of group A streptococcal sternoclavicular monoarthritis in an otherwise healthy patient. Streptococcus pharyngitis could be a risk factor for Strep pyogenes SCSA, and conservative management may more likely be successful in patients with similar presentations. Our report demonstrates a need for an establishment of meaningful measures in staging and management required to minimize risks of unnecessary harm.
Data Availability
Data not discussed or displayed in this report remains unavailable for patient privacy.
Conflicts of Interest
None.
Funding
None.
Acknowledgment
None.
Abbreviation
SCSA: Sternoclavicular Septic Arthritis
SCJ: Sternoclavicular Joint
IV: Intravenous (into a Vein)
PO: Per Os (by mouth)
CT: Computed Tomography
Article Info
Article Type
Case ReportPublication history
Received: Fri 28, Oct 2022Accepted: Thu 24, Nov 2022
Published: Mon 19, Dec 2022
Copyright
© 2023 SangMin Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2022.04.03
Author Info
SangMin Kim Evert A. Sugarbaker M. Blair Marshall
Corresponding Author
SangMin KimHarvard Medical School, Boston, Massachusetts, USA
Figures & Tables
References
1. Tasnim S, Shirafkan
A, Okereke I (2020) Diagnosis and management of sternoclavicular joint
infections: a literature review. J Thorac Dis 12: 4418-4426. [Crossref]
2. Bayfield NGR, Wang
E, Larbalestier R (2020) Medical and conservative surgical management of
bacterial sternoclavicular joint septic arthritis: a case series. ANZ J Surg
90: 1754-1759. [Crossref]
3. Savcic Kos RM, Mali P, Abraham A, Issa M, Rangu V et al. (2014) Streptococcus pyogenes sternoclavicular septic arthritis in a healthy adult. Clin Med Res 12: 155-159. [Crossref]
4. Kachala SS, D'Souza DM, Teixeira Johnson L, Murthy SC, Raja S et al. (2016) Surgical Management of Sternoclavicular Joint Infections. Ann Thorac Surg 101: 2155-2160. [Crossref]
