Cyst of Canal of Nuck in a 62-Year-Old Woman: Case Report of a Rare Disease
A B S T R A C T
Introduction: Cyst of Nuck in women is a rare development disorder corresponding to hydrocoele of the spermatic cord in males; it can be associated with inguinal hernia in 30-40% of cases. Only 400 cases have been described in literature and in there are no older than 50.
Case Presentation: A 62-year-old presented a right aching inguinal swelling. On physical examination the mass was not reducible, without signs of incarceration or strangulation. On ultrasound the lesion was mostly hypoechoic. CT saw an over liquid lesion, confirmed on MRI as a lesion hypointense in T1 and hyperintense in T2. The patient underwent open surgery: the cyst was separated from the round ligament and excised in mass and the defect was repaired with a prolene mesh. The histopathological exam confirmed the hydrocoele (calretinin positive, mesothelial cells on the inner surface).
Discussion: The canal of Nuck is a small evagination of the parietal peritoneum that accompanies the round ligament into the inguinal canal during the first year of female development and is normally obliterated in the first year of life. Failure of obliteration of Nuck canal results in a hydrocoele that could develop intra-abdominal or extra – abdominal or both. Ultrasound shows a thin walled, well defined, echo free cystic structure but the perfect diagnosis is given by MRI. Therapy is surgical and it can be open or, more recently, laparoscopic, depending on the expertise of the surgeon.
Conclusion: A cyst of Nuck is a rare condition but it should always be considered in differential diagnosis of cystic inguinal lumps in women. Most of the reported cases concern children and young men. To our knowledge this is the only case regarding a more than 50-year-old.
Keywords
Canal of nuck, hydrocoele, inguinal hernia, female inguinal swelling, cyst of nuck canal
Introduction
Congenital hydrocoele is frequently seen in male child but it is uncommon in female [1]. Hydrocoele of the canal of Nuck is a rare development disorder corresponding to hydrocoele of the spermatic cord of males. Presentation in adult is limited due to very few cases reported. The rarity of this finding in women is described in only 400 cases [1]. Swelling of the inguinal region in a woman is a relatively frequent finding in daily clinical practice and the differential diagnosis should consider inguinal hernias, lymphadenopathy, Bartolini’s gland abscesses, post-traumatic hematoma, while a cyst of Nuck is a rare entity, seldom diagnosed [2]. We aimed to contribute to the literature by presenting a case of postmenopausal woman as there are only few examples of this benign pathology in literature and no one in a woman older than fifty.
Case Report
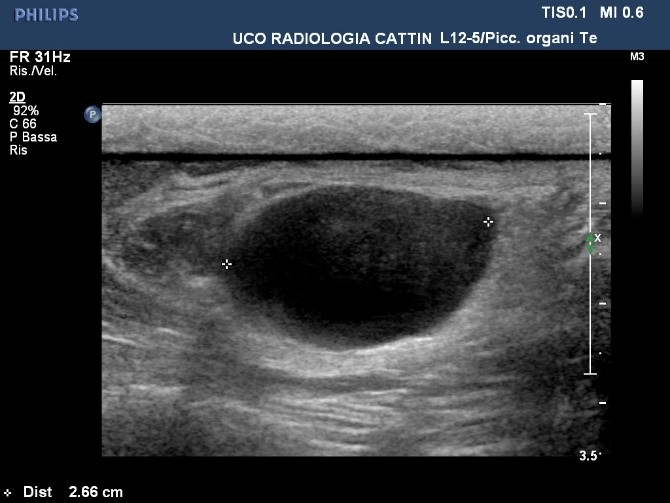
A 62-year-old woman was referred to our department of General Surgery as her physician suspected an inguinal hernia. She presented with right inguinal swelling, telling the mass was initially small but gradually increased, becoming more aching. The patient denied urinary and intestinal symptoms, a previous history of trauma or surgery, as well as gynecological diseases. She was a fit woman on medical treatment for hypothyroidism who never underwent surgery. On physical examination the mass was tense elastic, about 3 cm in diameter, with a smooth surface, soft consistency and tender on palpation. Cough impulse was absent. Transillumination test was negative. Lymph nodal examination was normal. Although the lesion was irreducible, there was no evidence of incarceration or strangulation, the overlying skin showed no sign of inflammation. The laboratory tests were within the limits. Then the patient was referred to the department of Radiology to undergo some radiological investigations. The ultrasound showed a lesion (about 2.6x3.2x1.6cm) near the external inguinal ring, with an heterogenous echogenicity, mostly hypoechoic, with some hyperechoic parts inside (Figure 1).
Figure 1: Ultrasound image of hydrocoele.
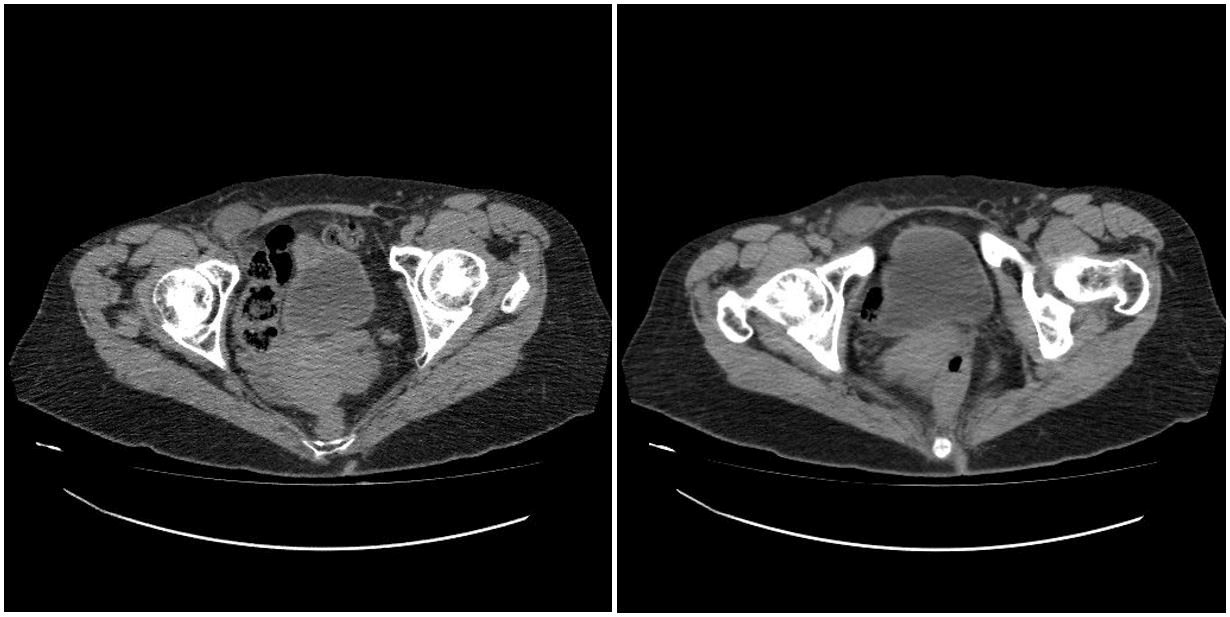
Figure 2: TC signs of hydrocoele.
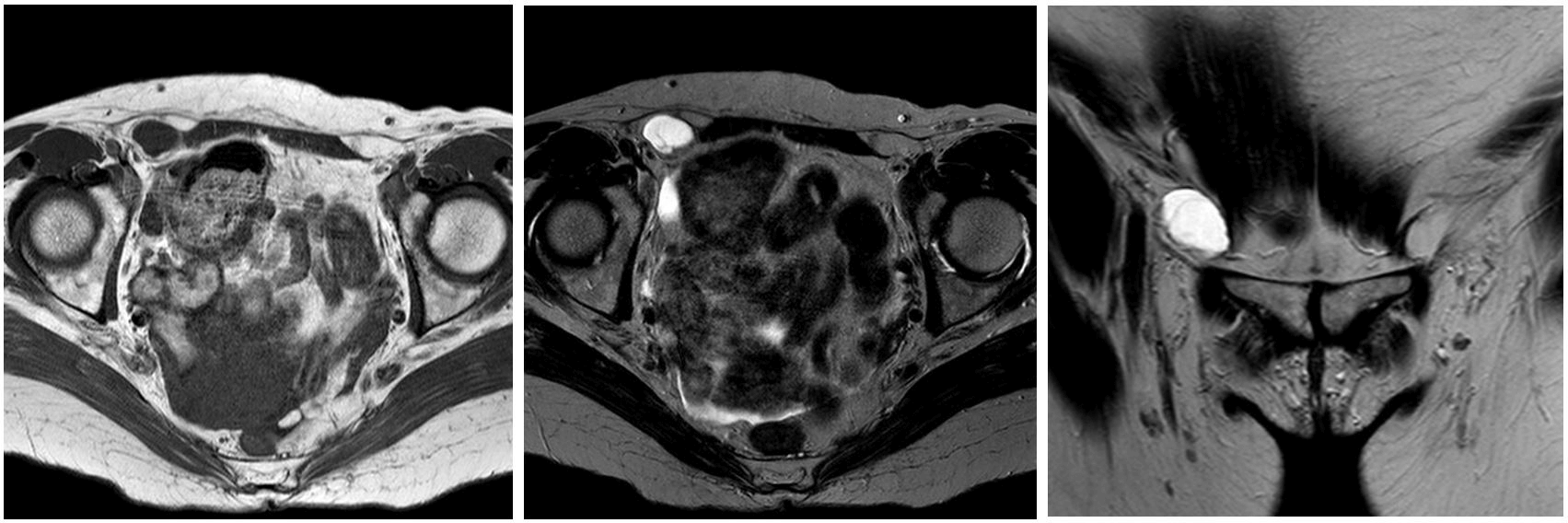
Figure 3: MRI images of hydrocoele of Nuck canal: Hypointense in T1 sequences; Hyperintense in T2 sequences.
Based on clinical and ultrasound findings, an hydrocoele of the canal of Nuck was suspected. In order to confirm the diagnosis, the patient underwent a CT and MRI. The CT of the lower abdomen showed an over liquid lesion in the right external inguinal ring, medially the pubic symphysis, posteriorly the external oblique muscle, laterally the femoral vessels, without any sign of crural herniation (Figure 2).
The MRI described an oval lesion of 16x25 mm, hyperintense in T2 sequence and hypointense in T1, near another cystic lesion along the round ligament. All these radiological findings confirmed the suspect of cyst of the canal of Nuck (Figure 3).
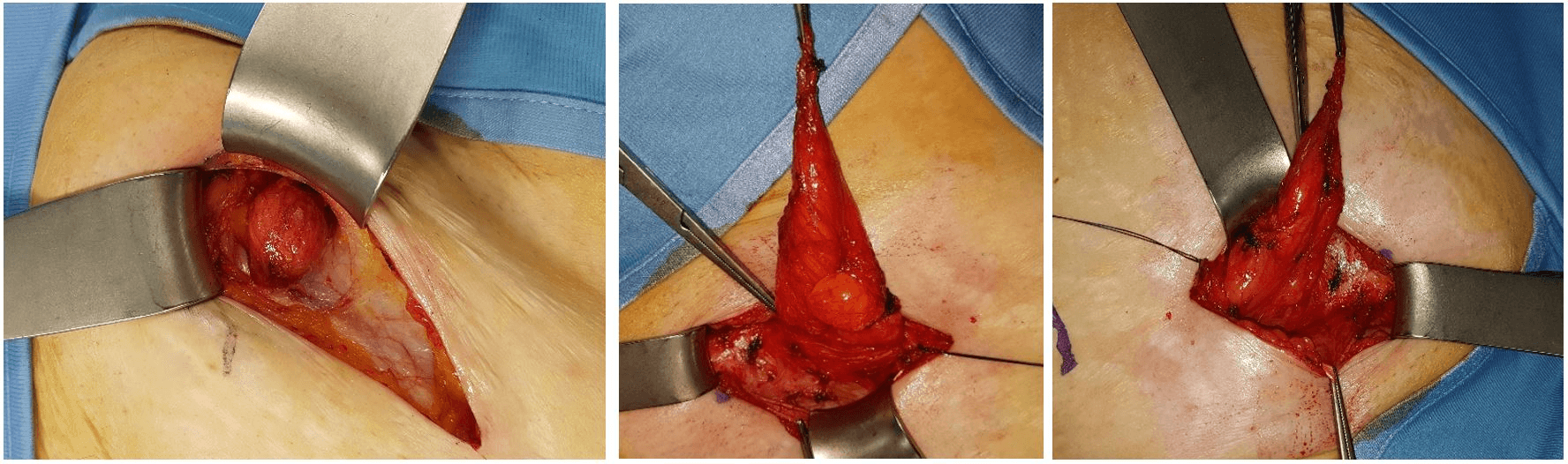
Few weeks after the diagnosis, the patient underwent surgery. We performed an open surgery under local anesthesia and conscious sedation: incision over the right inguinal skin extended through subcutaneous tissues, the fascia of external oblique muscle opening the inguinal canal. Here, the cystic lesion was seen to be originated from the external opening of inguinal canal (Figure 4). The cyst was separated from the round ligament excised in mass and sent for histopathological examination. The defect was repaired with a prolene mesh after high ligation of the sac, using Lichtenstein technique. The fascia of external oblique muscle, subcutaneous tissue and skin were closed in layers. The patient was discharged six hours after the end of operation. Postoperatively the patient was relieved of all her symptoms. Histopathological examination confirmed that the specimen was an hydrocoele of the canal of Nuck.
Figure 4: Intraoperative findings of hydrocoele of Nuck canal.
Microscopic findings of the cyst showed cystic walls, sclerotic in some parts, consisted of mesothelial cells (calretinin +) on the inner surface, surrounded by fibroadipose and muscular tissues with vascular structures. The patient returned to a control visit one week after surgery: there was no sign left of the previous swelling and she confirmed the end of all previous pain. At 8 months’ phone control the Patient was fine and asymptomatic.
Discussion
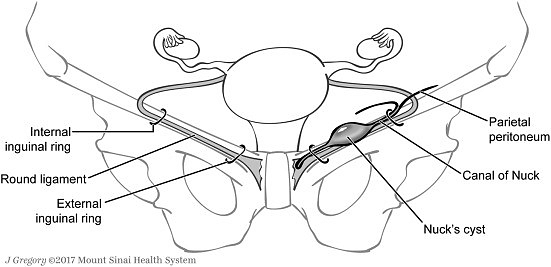
The canal of Nuck was first described by the Dutch anatomist Anton Nuck in 1691 in ‘Adenographia Curiosa et uteri foeminei anatomenova’ and the first report of a hydrocoele of Nuck was attributed to Aetius in 543 by Coley [3, 4]. The canal of Nuck is a small evagination of the parietal peritoneum that accompanies the round ligament into the inguinal canal during the first year of female development [5, 6]. The canal of Nuck is the processus vaginalis within the inguinal canal in women [7]. This canal is normally obliterated in the first year of life (Figure 5) [7, 8].
Failure of obliteration of Nuck canal results in a hydrocoele. The aetiological factors are idiophatic, inflammatory, traumatic or impairment or lymphatic drainage [5]. Counseller and Black classified hydrocoele of the canal of Nuck into 3 types [5]. The first and most common is a hydrocoele that can be anywhere along the course of the round ligament, without communication with the peritoneal cavity. The second is similar to the hydrocoele in males, as it presents communication with the peritoneal cavity, and the third type presents a constriction at the internal ring, so the upper sac is intra-abdominal, but outside the peritoneum, the lower sac is in the inguinal canal [5].
Figure 5: Canal of Nuck anatomy.
In 1892, Coley described 14 cases of hydrocoele in women, but he stated that this affection was “too rare as abnormality to deserve consideration” [1]. Most of the cases were reported in neonates and infants [4]. The cyst of Nuck is a rare condition in adult patients: Block reported 5 cases in 1975, only 400 cases of hydrocoele of the Nuck canal are described nowadays in literature [4, 9]. Topal et al. reported a case in a 42-year-old woman, as Lombardo et al. and Cavilzel et al. described a case of Nuck cyst in a 28-year-old; Manenti et al. in a 37-year-old one, Patman et al., Walter H et al., Ozel et al. in a 38-year-old woman. Only Riquard L et al. referred a case in a 44-year-old, the oldest one reported in literature.
Pathologically, the cyst of the canal of Nuck is a thin, walled, clear fluid-containing cyst, lined by a single layer of mesothelial cells [5]. In literature, the majority of reported cases of hydrocoele of the canal of Nuck was diagnosed in the surgical specimen obtained after surgery performed for a suspected inguinal hernia [1]. Palpable masses of the inguinal region may give rise-up to a several differential diagnoses, where the most frequent is an inguinal hernia [9]. However, other causes should be considered such as: nodal enlargements, soft tissue neoplasm, cyst of ganglia, perineal abscesses, Bartholin’s cyst and endometriosis of the round ligament [5, 9].
The clinical presentation of all these pathological findings is different from that of the hydrocoele of the canal of Nuck, which typical presentation consists of a persistent, translucent, mobile and irreducible swelling in the inguinal-labial region [5]. The cyst is located along the line of the round ligament and can extent to the labium majus [5]. Because of these characteristics, a cyst of the Nuck canal is frequently misdiagnosed for an inguinal hernia, particularly for a strangulated one., even if an inguinal hernia is rare in women.
Another key difference is that a cyst of Nuck canal is painless even if irreducible and during dynamic evaluation on Valsalva it shows no change in size or shape [5]. The size of the lesion is usually small, about 3 cm in length and 0.3-0.5 cm in diameter [7]. Imaging studies can help in diagnosis. The most useful radiological exams are ultrasound and magnetic resonance [10].
Ultrasound is preferred due to the superficiality of the lesion and is well visualised with high frequency linear array transducer [7]. The mass lies superficially and medial to the pubic bone in the inguinal canal, with enhanced posterior through translucency [3]. Sonographic appearance of hydrocoele of the canal of Nuck shows a thin walled, well defined, echo free cystic structure, varying from an anechoic, tubular, sausage or comma shaped to a multi-cystic appearance [1]. It can be seen as an anechoic or hypoechoic unilocular or multilocular structure, with no internal vascularity on colour-doppler [5]. High resolution ultrasonography offers an efficient non-invasive investigation for diagnosis, it is easy, quick and it gives a higher accurate imaging modality [5, 11].
However, the gold standard for diagnosis is magnetic resonance [5]. It gives a more precise image, including septation and communication between cystic lesions and peritoneal cavity, information on the anatomical relation with adjacent structures [7]. The cyst of the canal of Nuck is frequently seen as a cystic thin walled structure in the inguinal area with hypointense T1 signal and hyperintense T2 signal characteristic [11]. The cyst doesn’t enhance after injection of contrast medium (gadolinium) which is considered as a sign of benignancy [4]. Although MRI gives the diagnosis, if a confirmation can be made with ultrasonography alone, MRI should be avoided as it is more expensive [5].
Therapy of a cyst of Nuck canal is surgical. Ultrasound-guided aspiration has been proposed only for a temporary symptomatic relief, but it has no place in treatment [1, 12]. The classic surgical approach is open, but recently have been published four cases who described a laparoscopic access [13, 14]. Open surgery consists of a small transverse incision, preparation of the hydrocoele, ligation of the neck of the processus vaginalis and cut of the round ligament [12]. The use of synthetic polypropylene mesh will prevent surgical failure, due to the fact that cyst may be associated with inguinal hernia in about 30-40% of cases [1, 4].
In only four cases a laparoscopic approach has been reported: Nafees J Quareshi et al. report a case of a 28-year-old female which underwent laparoscopic excision of cyst of Nuck with TAAP repair (Transabdominal preperitoneal), as the other more recent [5, 13, 14]. Only one TEP (Totally extraperitoneal) repair has been reported [15]. The major limit for the laparoscopic technique is the necessity of general anesthesia. On pathological examination the cyst of the canal of Nuck shows to be made of fibrovascular tissue with a single layer of cuboidal mesothelial cells on the inner surface, and it is filled with light colored fluid [1, 5].
Conclusion
Even if a cyst of the Nuck canal is a rare condition, it should always be considered in differential diagnosis of cystic inguinal lumps in women. The clinical suspect must be followed by a radiological examination with ultrasound and, if possible, with MRI. Surgery is the treatment of choice, open or laparoscopic depending on the expertise of surgical team. Minimal access surgery could permit to avoid performing MR pre-operatively, except if pelvic endometriosis is suspected [16]. In literature are reported few cases, most of them concerning children and young men. Cases considering women talks about 28 and 44-year-old women, but we demonstrated that this affection can be diagnosed also in post-menopausal women with a silent history for inguinal swelling. To our knowledge this is the only case reported in literature of a cyst of the canal of Nuck in a woman older than 50-year-old.
Conflicts of Interest
None.
Ethical Approval
I certify that this kind of manuscript does not require ethical approval.
Article Info
Article Type
Case ReportPublication history
Received: Tue 21, Apr 2020Accepted: Tue 05, May 2020
Published: Tue 12, May 2020
Copyright
© 2023 Livia Bressan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.02.03
Author Info
Barbara Pozzetto Bussani Rossana Livia Bressan Marina Bortul Pizzolato Riccardo
Corresponding Author
Livia BressanDoctor Resident in General Surgery, Surgery specialization school of Trieste Academic Hospital, Department of General Surgery, Azienda Ospedaliera Universitaria Giuliano Isontina, Ospedale di Cattinara, Strada Di Fiume, Trieste, Italy
Figures & Tables
References
- Topal U, Sarıtaş AG, Ülkü A, Akçam AT, Doran F (2018) Cyst of the canal of Nuck mimicking inguinal hernia. Int J Surg Case Rep 52: 117-119. [Crossref]
- Hensgens RL, Breek JK (2016) A woman with a painful swelling in the groin: The cyst of Nuck, a forgotten diagnosis. Ned Tijdschr Geneeskd 160: A9476. [Crossref]
- Lombardo V (2017) Surgical treatment of cyst of the canal of Nuck: report of a case. World J Surg Res 8.
- Caviezel A, Montet X, Schwartz J, Egger JF, Iselin CE (2009) Female hydrocele: the cyst of Nuck. Urol Int 82: 242-245. [Crossref]
- Patnam V, Narayanan R, Kudva A (2016) A cautionary approach to adult female groin swelling: hydrocoele of the canal of Nuck with a review of the literature. BMJ Case Report pii: bcr2015212547. [Crossref]
- Sala P, Palmeri A, Costantini S (2018) Giant cyst of the Nuck canal: a worrisome trouble for a girl. Am J Obstet Gynecol 218: 530-531. [Crossref]
- Quareshi NJ, Lakshman K (2014) Laparoscopic excision of cyst of canal of Nuck. J Minim Access Surg 10: 87-89. [Crossref]
- Hensgens RL, Breek JK (2016) A woman with a painful swelling in the groin: The cyst of Nuck, a forgotten diagnosis. Ned Tijdschr Geneeskd 160: A9476. [Crossref]
- Manenti G, D'Amato D, Ranalli T, Marsico S, Castellani F et al. (2019) Cyst of canal of Nuck in a young woman affected by kniest syndrome: ultrasound and MRI features. Radiol Case Rep 14: 217-220. [Crossref]
- Stickel WH, Manner M (2004) Female hydrocele (cyst of the canal of Nuck): sonographic appearance of a rare and little-known disorder. J Ultrasound Med 23: 429-432. [Crossref]
- Ozel A, Kirdar O, Halefoglu AM, Erturk SM, Karpat Z et al. (2009) Cysts of the canal of Nuck: ultrasound and magnetic resonance imaging findings. J Ultrasound 12: 125-127. [Crossref]
- Zawaideh JP, Trambaiolo Antonelli C, Massarotti C, Remorgida V, Derchi LE (2017) Cyst of Nuck: A Disregarded Pathology. J Minim Invasive Gynecol 25: 376-377. [Crossref]
- Bunting D, Szczebiot L, Cota A (2013) Laparoscopic hernia repair-- when is a hernia not a hernia? JSLS 17: 654-656. [Crossref]
- Shahid F, El Ansari W, Ben Gashir M, Abdelaai A (2020) Laparoscopic hydrocelectomy of the canal of Nuck in adult female: case report and literature review. Int J Surg Case Rep 66: 338-341. [Crossref]
- Matsumoto T, Hara T, Hirashita T, Kubo N, Hiroshige S et al. (2014) Laparoscopic diagnosis and treatment of a hydrocele of the canal of Nuck extending in a retroperitoneal space: A case report. Int J Surg Case Rep 5: 861-864. [Crossref]
- Chihara N, Taniai N, Suzuki H, Nakata R, Shioda M et al. (2020) Use of a Novel Open Posterior Wall Technique for Laparoscopic Excision of Hydrocele of the Canal of Nuck in an Adult Female: Case Report. J Nippon Med Sch 86: 345-348. [Crossref]
