Journals
Decompression of Mandibular Odontogenic Keratocyst Using A Custom Drain: A Technical Note
A B S T R A C T
The odontogenic keratocyst (OKC) is a benign but locally aggressive cyst that has a potentially high recurrence rate and morbidity associated with different treatment approaches. Decompression of odontogenic cysts is a well-established technique that has been shown to decrease the size of the cyst and need for sacrificing local structures during ensuing definitive treatment. Multiple devices have been previously described for decompression of OKCs utilizing varying drain material and modes of fixation, but have been complicated by device malposition, soft tissue overgrowth, poor hygiene, and suture dehiscence. This paper describes the application of a custom titanium drain (Biomet ® Jacksonville, FL) secured using bone screws for decompression of an OKC in a 77-year-old male.
Keywords
Custom drain, odontogenic keratocyst, odontogenic cyst, decompression
Introduction
The odontogenic keratocyst (OKC) is a developmental cyst derived from dental lamina and most frequently occurs during the second and third decades of life [1]. It commonly presents in the mandibular third molar and ascending ramus region but has been described in all dentate portions of the maxilla and mandible [2]. OKCs are often associated with impacted third molars and comprise roughly 11% of jaw cysts. On plain radiographs, they appear as a unilocular or multilocular lesion with scalloped borders [3]. Since OKCs share radiologic features similar to many other odontogenic cysts, imaging alone is not sufficient for definitive diagnosis [2]. OKCs and are known for their locally aggressive nature. They can penetrate cortical bone, surrounding soft tissue, displace the inferior alveolar nerve, and extend from the mandible to involve the base of the skull [4-6]. The recurrence rate ranges from 3 to 60% depending on surgical management utilized with the initial treatment [7]. This recurrence is attributed to satellite cysts of the fibrous walls and incomplete removal of cyst secondary to the thin friable nature of the lesion [8]. The difficulty in treating this cyst and variable recurrence rates has led to some proposed aggressive treatments such as radical resection [9]. Other approaches may include enucleation with adjunctive peripheral ostectomy, application of Carnoy’s solution or cryotherapy [10, 11]. For smaller cysts, enucleation and application of Carnoy’s solution is the least invasive treatment with the lowest recurrence rate [12]. However, complete enucleation may not be practical in larger cysts and radical resection results in greater morbidity and requires secondary reconstruction. Therefore, in cases such as this, it may be prudent to decrease the size of the lesion via decompression or marsupialization prior to definitive surgical treatment. Marsupialization refers to the externalization of the cyst via creation of surgical window through the buccal mucosa and cystic wall, allowing the cystic cavity to directly communicate with the oral cavity. Decompression is a similar technique but uses a foreign object such as a nasal trumpet or surgical drain to prevent mucosal closure and allow irrigation by the patient [3]. Multiple devices have been utilized for the decompression of odontogenic cysts [13-16]. Unfortunately, they have been associated with the several negative outcomes: device malposition, dislodgement, soft tissue trauma, inappropriate sizing, soft tissue overgrowth, inability to clean the device, and suture dehiscence [14]. This case report describes the successful use of a custom titanium drain (Biomet® Jacksonville, FL) for decompression of an OKC and subsequent definitive enucleation.
Case Report
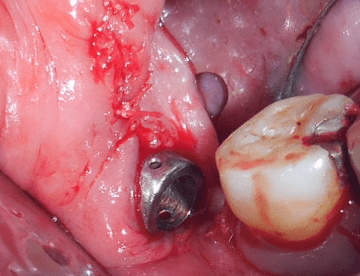
A 77-year-old male with medical history significant only for hypertension presented with an expansile and compressible lesion of the right ascending ramus not associated with teeth (Figure 1a). A panoramic radiograph was obtained and demonstrated a large expansile unilocular radiolucency extending from the angle of the right mandible to the coronoid process. Further imaging with computed tomography revealed a well-defined, expansile lesion of the right mandible 5.0x3.4x3.0cm in size at its greatest dimension with buccal and lingual dehiscence (Figure 1b). The lesion effaced the superior aspect of the inferior alveolar nerve canal at the angle of the mandible. Due to the size of the lesion and advanced age of the patient, he elected to undergo decompression of the lesion prior to subsequent enucleation and immediate reconstruction. Under general anesthesia, an incision was made to allow for exposure of the lesion in order to obtain incisional biopsy specimen and place the custom drain. During the exposure of the lesion, a significant amount of keratinous material was evacuated from the cyst (Figure 2a). A window was created on the superior aspect of the cyst to allow placement of the custom drain, which was designed using virtual surgical planning. The drain contained two arms to allow placement of bone screws on both buccal and lingual cortices. In this case, only one arm was utilized, and the second arm removed with plate cutters (Figure 2b and 2c). The proper position of the drain allowing access to all regions of the cyst was verified using an endoscope and incision closed in a tension free manner (Figure 2d). Histopathologic examination confirmed the diagnosis of an OKC.
Figure 1A: Preoperative clinical photograph of expansile right mandibular lesion
Figure 1B: Sagittal cut of computed tomogram showing extent of lesion and continuity with the inferior alveolar nerve canal
Figure 2A: Clinical photograph of cystic contents.
Figure 2B: Custom drain
Figure 2C: Custom drain secured with bone screws
Figure 2D: Clinical appearance of custom drain after intraoral wound closure
The patient was instructed to self-irrigate the drain with normal saline on a daily basis while the lesion was monitored by serial radiographs every several months to confirm the reduction in cyst size (Figure 3a). One year following drain placement, the greatest extension of the lesion measured 4.1x2.0x1.8 cm on computed tomography and the lesion no longer involved the inferior alveolar nerve (Figure 3b). Following successful decompression of the cyst, the patient was brought back to the operating room for definitive treatment including removal of the drain, enucleation of the cyst, peripheral ostectomy using rotary instrumentation and application of Carnoy’s solution to the bony cavity for three minutes. The Carnoy solution utilized at our facility does not contain formalin. The bony defect was reconstructed at that time using allogeneic bone graft mixed with platelet rich plasma secured with a collagen membrane. The patient’s postoperative course was uneventful, and his only complaint was mild right inferior alveolar nerve distribution hypoesthesia at his one-week postoperative visit, which resolved prior to his three-month visit. Decompression of the cyst allowed for bony regeneration and preservation of the inferior alveolar nerve as well as definitive treatment with minimal morbidity (Figure 4). The patient has been followed for three years with no signs of recurrence.
Figure 3A: Panoramic radiograph of decompressed right mandibular cyst with custom drain in place
Figure 3B: Sagittal cut of computed tomogram of decompressed right mandibular cyst
Figure 4: Panoramic radiograph of mandible after definitive treatment of OKC and reconstruction
Discussion
Treatment of odontogenic cysts remains a topic of debate due to the diversity of their features. OKCs are more locally aggressive and recur frequently compared to other odontogenic cysts [7]. Simple curettage will result in the highest recurrence rate. It is generally accepted that cysts less 3cm in diameter can be treated by primary enucleation, however, larger lesions present a treatment dilemma due to high risk of recurrence with limited accessibility to some regions and morbidity associated with primary resection [17]. Some authors recommend biopsy of all larger lesions prior to definitive treatment or alternatively applying Carnoy’s solution as adjunctive therapy for cyst enucleation without previous histopathologic examination [12]. Decompression of any large odontogenic cyst allows for preservation and regeneration of bone and surrounding vital structures. This can decrease the morbidity associated with definitive treatment by decreasing proximity to local vital structures and enhancing the structural integrity of the jaw. Less invasive reconstruction approaches, such as allogeneic bone grafting instead of autogenous grafting are then possible leading to decreased patient discomfort, cost of treatment, and recovery time [3]. Although the decompression technique can be used for any large odontogenic cyst, it is particularly beneficial for OKCs, which can be especially difficult to enucleate entirely and are prone to recurrence due to thin epithelial lining and presence of daughter cysts. Furthermore, decompression has been shown to alter the histopathology of OKC epithelial lining resulting in more normal epithelium [18]. The drawback is the need for two separate procedures, although drain application may be implemented as an in-office procedure during the initial biopsy.
A variety of decompression devices have been described in the literature. The devices are often made of malleable materials such as rubber cylinders, polyethylene stents, urethral catheters and nasopharyngeal tubing [19]. The devices are frequently secured in the cystic cavity via sutures or wires and are prone to failure. Suturing the device does not provide adequate security and devices often dislodge from the cystic cavity or advance into soft tissue. Wiring the device requires adjacent teeth and can cause local soft tissue trauma.
This case report demonstrates the use of a custom drain for the decompression of an OKC in a 77 year-old male. Over the course of a year, the size of the cyst drastically decreased resulting in marked bony regeneration around the inferior alveolar nerve canal to allow for preservation of the nerve and maintenance of mandibular continuity. The custom drain has many key elements of an ideal decompression device: fixated in place, avoided dislodgement into the bony cavity, small enough not to interfere with mastication, provided an accessible port to irrigate the cystic cavity, and was hygienic and easily cleansed by the patient [20]. As such, the custom drain is a promising device to have in the surgeon’s armamentarium for decompression of large OKCs and other odontogenic cysts.
Declaration of interest
None
Article Info
Article Type
Research ArticlePublication history
Received: Mon 15, Apr 2019Accepted: Fri 24, May 2019
Published: Tue 18, Jun 2019
Copyright
© 2023 Michael T. Jungwirth. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2019.03.03
Author Info
Michael T. Jungwirth Vincent B. Ziccardi
Corresponding Author
Michael T. JungwirthRutgers School of Dental Medicine, Department of Oral and Maxillofacial Surgery, Newark, NJ, USA
Figures & Tables







References
- Brannon RB (1976) The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part I. Clinical features. Oral Surg Oral Med Oral Pathol 42: 54-72. [Crossref]
- Stoelinga PJ (2001) Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg 30: 14-25. [Crossref]
- Maurette PE, Jorge J, de Moraes M (2006) Conservative treatment protocol of odontogenic keratocyst: a preliminary study. J Oral Maxillofac Surg 64: 379-383. [Crossref]
- Emerson TG, Whitlock RI, Jones JH (1972) Involvement of soft tissue by odontogenic keratocysts (primordial cysts). Br J Oral Surg 9: 181-185. [Crossref]
- Partridge M, Towers JF (1987) The primordial cyst (odontogenic keratocyst): its tumour-like characteristics and behaviour. Br J Oral Maxillofac Surg 25: 271-279. [Crossref]
- Jackson IT, Potparic Z, Fasching M, Schievink WI, Tidstrom K et al. (1993) Penetration of the skull base by dissecting keratocyst. J Craniomaxillofac Surg 21: 319-325. [Crossref]
- Shear M (2002) The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 1. Clinical and early experimental evidence of aggressive behaviour. Oral Oncol 38: 219-226. [Crossref]
- Bataineh AB, al Qudah M (1998) Treatment of mandibular odontogenic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 86: 42-47. [Crossref]
- Bramley P (1974) The odontogenic keratocyst--an approach to treatment. Int J Oral Surg 3: 337-341. [Crossref]
- Voorsmit RA (1985) The incredible keratocyst: a new approach to treatment. Dtsch Zahnarztl Z 40: 641-644. [Crossref]
- Jensen J, Sindet-Pedersen S, Simonsen EK (1988) A comparative study of treatment of keratocysts by enucleation or enucleation combined with cryotherapy. A preliminary report. J Craniomaxillofac Surg 16: 362-365. [Crossref]
- Blanas N, Freund B, Schwartz M, Furst IM (2000) Systematic review of the treatment and prognosis of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90: 553-558. [Crossref]
- Kolokythas A, Schlieve T, Miloro M (2011) Simple method for securing a decompression tube for odontogenic cysts and tumors: a technical note. J Oral Maxillofac Surg 69: 2392-2395. [Crossref]
- Costa FW, Carvalho FS, Chaves FN, Soares EC (2014) A suitable device for cystic lesions close to the tooth-bearing areas of the jaws. J Oral Maxillofac Surg 72: 96-98. [Crossref]
- Shakib K, Heliotis M, Gilhooly M (2010) The nasopharyngeal airway: reliable and effective tool for marsupialisation. Br J Oral Maxillofac Surg 48: 386-387. [Crossref]
- Carter LM, Carr P, Wales CJ, Whitifield PH (2007) Customised stents for marsupialisation of jaw cysts. Br J Oral Maxillofac Surg 45: 429-431. [Crossref]
- Enislidis G, Fock N, Sulzbacher I, Ewers R (2004) Conservative treatment of large cystic lesions of the mandible: a prospective study of the effect of decompression. Br J Oral Maxillofac Surg 42: 546-550. [Crossref]
- Pogrel MA, Jordan RC (2004) Marsupialization as a definitive treatment for the odontogenic keratocyst. J Oral Maxillofac Surg 62: 651-655. [Crossref]
- Anavi Y, Gal G, Miron H, Calderon S, Allon DM (2011) Decompression of odontogenic cystic lesions: clinical long-term study of 73 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112: 164-169. [Crossref]
- Tolstunov L (2008) Marsupialization catheter. J Oral Maxillofac Surg 66: 1077-1079. [Crossref]
