Deep-Inspirational Breath-Hold (DIBH) Technique in Left-Sided Breast Cancer: An Institutional Review
A B S T R A C T
Purpose: The study of clinical effectiveness of deep-inspirational breath-hold (DIBH) in left breast cancer radiotherapy (RT) was aimed at focusing on dosimetry and organs at risk (OARs) evaluation. A retrospective study was conducted to assess the heart and ipsilateral lung V30 for DIBH technique and to compare with free breathing (FB) technique. Clinical data shows that by increasing the inhalation amplitude value (cm), the maximum heart distance decreases in the treatment field.
Materials and Methods: Thirty left-sided breast and chest wall patients were CT scanned on 4DCT with DIBH. These patients were chosen for the DIBH technique with the ability to hold their breath for more than 20 seconds. Radiotherapy of these patients was planned using field-in-field planning technique, and OAR doses were observed using the institutionally specified DIBH protocol.
Results: The mean heart dose was less than 3Gy. Whereas V2Gy and V10Gy were less than 30% and 5%. The mean ipsilateral lung dose was 7.59 Gy. Ipsilateral lung V30 was less than 25% with ±10% margins. It is found that by increasing the inhaling amplitude (cm) heart involvement in the tangential treatment field decreases.
Conclusion: DIBH is an easy and highly efficient treatment technique for reducing the mean dose of the heart and V30 of ipsilateral lung. The maximum heart distance decreases as the baseline of inhalation increases due to heart doses.
Keywords
Left breast radiotherapy, deep inspirational breath-hold (DIBH), heart protection, radiation lung damage
Introduction
Radiotherapy has played a vital role in the management of breast cancer for decades. Due to availability of the modern radiotherapy technologies, significant changes have occurred in radiotherapy practice focusing on optimized care on an individual basis [1, 2]. After breast-conserving surgery, most of the patients need postoperative whole breast irradiation (WBI) with or without a tumor bed boost, while in low-risk cases partial breast irradiation (PBI) is sufficient. Most of breast cancer patients become long-survivors; hence, therapeutic interventions should not compromise the patient’s general health and well-being. The main radiation-related hazards are radiogenic heart and lung damage resulting in significant morbidity for many years or decades after the radiotherapy [3-9]. Radiation-induced heart disease (RIHD) most frequently manifests in the damage of the coronary and capillary vessels of the heart, which induces a progressive fibrotic process leading to circulatory changes with potentially fatal ischaemic heart disease (IHD) [10]. The dose to the heart and hence RIHD incidence is higher in left-sided cases and the risk is more significant in young patients. It is estimated that every 1 Gy mean heart dose increases the incidence of IHD event by 7.4% that may be potentiated by pre-existing cardiovascular risk factors [11-14]. There are many approaches to protect the heart from radiation exposure. Prone positioning and the breath holding techniques operate by separating the heart and the radiation fields; the advanced IMRT and proton irradiation techniques are not widely applied, while the reduction of the volume to be irradiated during partial breast irradiation (PBI) or the emittance of radiotherapy are options in low-risk cases [15-23].
Previously, our institutional practice was to treat left-sided breast cancer patients with simple tangents while using enhanced dynamic wedges and this technique was not promising to reduce hotspot [24]. With the introduction of field-in-field technique, dosimetrists are able to reduce hotspot with homogenous coverage of target volume but the problem for the reduction of OAR’s doses was still there. Therefore, deep inspirational breath hold technique is introduced which is a promising method to reduce heart and lung doses with the homogenous coverage of target volume.
Deep inspiration breath hold (DIBH) is a method in radiation therapy in which patients take a deep breath and hold their breath while radiation is transmitted during treatment. There is no other way that we can minimize the cardiac dosage or raise the heart distance from the breast or chest wall other than this procedure [25, 26]. Post-operative RT for breast cancer patients has been widely used since it was proven to reduce the risk of local recurrence and improve long term survival [27, 28]. Several advanced methods are used to minimize heart and lung exposures depending on institutional experience and equipment availability, e.g., Intensity-modulated radiation therapy, Rapid Arc, Prone breast therapy, or respiratory correlation radiation [27]. DIBH is the most promising technique yet. During intact breast or chest wall RT, deep inspiration breath-hold (DIBH) increases the physical separation between the heart and the chest wall and thus decreases cardiac exposure. The heart moves away from the treatment area while patients taking a deep breath. However, not all patients benefit from DIBH equally. Several studies have examined DIBH cardiac gain predictors with several candidate steps, such as maximum heart distance and the distance from cardiac contact [2]. In this study, in patients with left-sided breast cancer undergoing irradiation, we aimed to test patient-related non-dosimetric cardiac sparing predictors using DIBH.
Materials and Methods
The institutional ethics review board had approved this retrospective study and all the enrolled patients gave their written informed consent to participation. Inclusion criteria was left-sided breast cancer needing postoperative WBI/PMI and informed consent, while the exclusion criteria were the presence of chronic obstructive pulmonary disease, bronchial asthma or other severe comorbidity that would hinder cooperation during DIBH (extreme obesity, mental disorder, hypacusis). Left-sided Breast Cancer patients that were selected for 4DCT DIBH scan were advised to hold their breath for 20 seconds during the scan. This study included 30 consecutive patients treated in 2020. At our hospital, all patients with left-sided BC undergo with only 4D getting CT scans, except for patients that are not clinically eligible for DIBH.
I CT Simulation and DIB
4DCT scanner, Aquilion LB (Toshiba Medical Systems Corporation, Otawara, Japan) was used for the time of simulation, these patients, using the Real-Time Role Control System and a visual coaching unit, were educated in the DIBH technique and respiratory gating devices. Respiratory gating is the advance method to capture the breathing cycles of the patient with the help of advanced gadgets. Real time position management (RPM) was placed on the abdominal surface. Reflector reflects the light from infrared laminator to charged coupled device (CCD). This is the camera, which is placed on fixed position relative to patient and connect to the computer. The real time software analyses the movement of reflector induced by the breathing. 4DCT scan was done on patients with Deep Inspiration Breath Hold. 4D CT uses a new technology that captures the location and movement of patient tumor and the movement of body’s organs over time. This is valuable for accurately treating tumors located on or near organs that move, such as those in the chest and the abdomen [29-33].
II Dosimetry and Treatment Planning
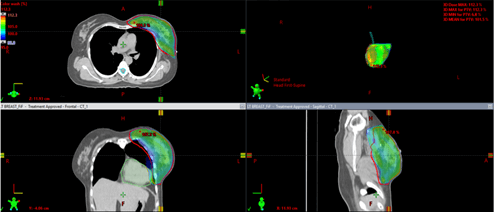
4D scanned patients were planned on Eclipse treatment planning system Aria 15.6 version (Varian Medical Systems, Palo Alto, CA, USA). Images imported to the treatment planning system with DIBH label scan. Oncologist contoured patient's breast and supraclavicular contour along with OAR's. After completing this process, the physicist proceeded to make a plan. Physicists placed beam angle to cover the target volume with minimum OARs in the treated fields using Field-in-Field technique. After completing the 90%-95% coverage of total dose to the target volume, physicist applied patches of low weightage in the plan, or field-in-field technique, and gradually reducing the hotpot while maintaining the coverage as shown in (Figure 1). When we achieved 110% of total doses within the target volume, coverage, and OAR doses, we merge all patches into one field. After that, the DIBH curve was attached to the plan that had been transferred from 4DCT. This breathing curve helped the patient to re-produce the required breathing pattern [10-16].
Figure 1: This figure is representing 95% coverage of target volume in all planes.
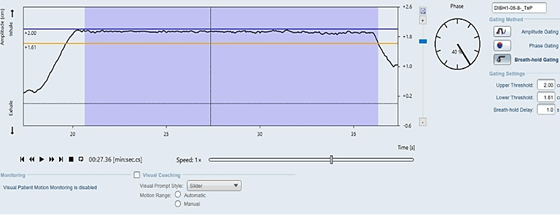
III DIBH Curve
All patients were instructed to hold their breath at least for 20 seconds during the CT scan as well as on the treatment couch, which is according to our hospital standard. Over the 40 seconds of run time, we calculated the baseline value for all patients. The upper threshold limit of the baseline value in this process was 2.00 whereas the lower threshold limit was 1.61 as shown in (Figure 2). About 70% of the data, collected in this study was consistent with threshold limits. At the 80% maximum inhale level, mean ratio of 1.80 was the best fit between the two systems, which was somewhat larger than the 1.37 ratio found for horizontal surfaces. However, lung expansion in anterior correlated to reduction in heart dose, which indicated, that the breathing pattern might be relevant for heart sparing, i.e., chest breathing for DIBH seems to be more beneficial than abdominal breathing.
Figure 2: Correlation between reduction in heart dose and breathing pattern.
Results
According to the inclusion and exclusion criteria, 30 patients were selected in the dosimetry analysis of DIBH cases. According to Bergom et al., DIBH technique could significantly reduce the Mean Heart dose in the patient [1]. H M Lu et al., showed that cardiac volume reduced in the tangential field when the patient held their breathe [2]. Vincent M Remouchamps discussed a comparison of free breathing treatment planning and deep inspirational breath hold (DIBH) treatment planning, and it clearly showed the reduction of 3.6% heart volume receiving V30 [3]. For greater homogeneity and target dose coverage, modern radiation techniques are used including intensity modulated radiation therapy (IMRT), prone positioning, Deep inspiration Breath Hold (DIBH) and respiratory gating can be used to minimize the dose to lung and heart by pulling the chest or breast away from the heart [10].
In order to make accuracy in the plan, oncologist have to put an eye on organ at risk of Deep Inspiration Breath Hold (DIBH) scan in which it included how much volume of the heart receiving 2Gy and 10Gy. According to our institute practice, heart V10Gy<5% and V2Gy<30%. Another important factor of heart is Mean heart dose, which should be less than 3Gy. Another important Organ at risk is Lung, V30% <25% and Mean Ipsilateral Lung Dose is 15%. Contralateral Breast Dose should not exceed mean 4Gy. Below given (Table 1) represents the OAR doses of each patient, which are taken from the Dose volume histogram.
Table 1: OAR doses to each patient.
|
No. of Patients |
IPSILATERAL LUNG V30%
|
Mean Ipsilateral lung dose (Gy) |
Mean Heart dose (Gy) |
Heart V2 (%) |
Heart V10 (%) |
|
1 |
18.4 |
7.39 |
1.5 |
12.6 |
2 |
|
2 |
15.5 |
7.48 |
3.12 |
29.8 |
6 |
|
3 |
7.5 |
4.53 |
1.08 |
14.6 |
0.4 |
|
4 |
19.6 |
7.83 |
2.76 |
16.6 |
6 |
|
5 |
18.1 |
7.5 |
2.04 |
16.6 |
3.8 |
|
6 |
20.7 |
8.46 |
3.1 |
19.1 |
6.8 |
|
7 |
15.7 |
7.03 |
1.39 |
10 |
2 |
|
8 |
19.5 |
9.58 |
1.28 |
15.7 |
0.7 |
|
9 |
21.7 |
8.74 |
2.45 |
24.3 |
5.4 |
|
10 |
18.8 |
8.16 |
2.92 |
24 |
5 |
|
11 |
13.9 |
6.08 |
1.9 |
17.2 |
3.2 |
|
12 |
19.6 |
8.2 |
2.62 |
23.8 |
4.8 |
|
13 |
14.7 |
6.42 |
0.91 |
10.4 |
0 |
|
14 |
15.1 |
7.36 |
1.57 |
21 |
1.5 |
|
15 |
23.4 |
10.49 |
1.7 |
24.2 |
1.29 |
|
16 |
10.4 |
5.53 |
2.53 |
21.5 |
5.96 |
|
17 |
14.1 |
6.62 |
2.81 |
23.5 |
6.78 |
|
18 |
17.2 |
7.7 |
2.6 |
20 |
5.2 |
|
19 |
20.3 |
8.3 |
2.6 |
20.9 |
5.2 |
|
20 |
25.9 |
10.44 |
2.7 |
29.4 |
5.5 |
|
21 |
11 |
11 |
1.25 |
12.3 |
1.3 |
|
22 |
11 |
5.05 |
1.32 |
13 |
1.5 |
|
23 |
10.5 |
5.6 |
2.89 |
23.2 |
5.78 |
|
24 |
21.2 |
8.5 |
1.05 |
12.1 |
0 |
|
25 |
16.4 |
6.47 |
1.76 |
19.2 |
2.4 |
|
26 |
10.3 |
5.87 |
1.5 |
17 |
1.2 |
|
27 |
20.8 |
8.67 |
1.73 |
15.6 |
2.1 |
|
28 |
13.5 |
6.64 |
1.88 |
23.5 |
2.58 |
|
29 |
18.4 |
7.97 |
1.85 |
20 |
2.4 |
|
30 |
19.3 |
8.04 |
1.03 |
10.6 |
1 |
I Maximum Heart Distance vs Inhalation
For each of the patient, we also calculated the average value of the maximum heart distance and inhale threshold values of DIBH curve. Data shows that only three patients does not gain any advantage due to anatomy while the majority of patients find advantage from this treatment. The maximum heart distance was measured in cm. It was determined by multiple examination that the upper threshold decreased as the maximum heart distance increased. For both threshold values, we have presented a graph, maximum heart distance against threshold values. By using the line of trends, it has been shown that both threshold values decreased as maximum heart distance increased as shown in (Figure 3). The difference between upper and lower threshold values should be at least 0.5 cm.
Figure 3: The relation between maximum heart distance to inhale baseline.
II Mean Heart Dose
We have calculated Mean Heart Dose for each patient and below mentioned graph shows that there are only two patients whose mean heart dose goes above 3 Gy and all other patients are below 3Gy according to RTOG 1005 trail, which is very low as compared to free breathing scan as shown in (Figure 4) [34]. Pitchaya Sakyanum et al. indicates that Mean heart dose for deep inspirational breath hold technique is 2.95±2.3 Gy [35].
Figure 4: Mean Heart Dose.
III Ipsilateral Lung Dose
According to RTOG 1005 protocol, 30% of the total dose should be less than 25% of the total structure volume. In addition, our data which is represented in the form of line chart clearly represents that lung dose of all patients is in the Range of 25Gy ±10% as shown in (Figure 5) [36].
Figure 5: V30% of the left lung.
Discussion
DIBH could not be implemented for all patients. We found that even among patients seemingly appropriate for the technique, about 20% could not practice DIBH, and 15% of the rest due to dosimetry concerns had to receive RT using an alternative technique. Furthermore, although in the remaining cases the DIBH maneuver resulted in reduced heart and LAD and lung doses in most, still, in some cases FB or prone positioning yielded superior or equal dosimetry results. Tanguturi et al. found that among 146 patients deemed potential candidates for breast radiotherapy with DIBH, the DIBH technique provided a neutral change in 25 (17%) or even increased MHD in 14 (10%) cases [37]. A beneficial effect was favoured by the young age, greater body mass index (BMI) and larger inspirational lung volume changes [37]. Dell’Oro et al. demonstrated that the benefit provided by DIBH in OAR doses individually differs. Notably, 3 out of 20 patients had higher heart, 4 had increased LAD and 6 had increased lung doses under DIBH as compared to FB [22].
Previously due to lack of resources in our institute, we used to plan and treat the patients on free breathing scans by using enhanced dynamic wedge technique. With this method, we reduced hotspot as well as the OAR doses to some limit. Later on, our institute changed the method of planning from enhanced dynamic wedges to Field-in-Field technique on free breathing scans. Field-in-field technique is, however, that was still not good enough to achieve as low as mean heart dose in the patients with the good coverage of target volume. Because to control the heart dose with at least 90% coverage of the target tumor was very difficult.
Therefore, institute introduced a deep inspiration breath hold scan with field-in-field technique. However, radiotherapy has also late treatment side effects, especially on the heart and coronary arteries in left-sided breast cancer patients. Therefore, recent studies have focused on techniques, especially the DIBH technique, that can reduce radiation doses to the heart and LAD [18].
Planning technique remain same while the method of scan change from free breathing to deep inspiration. Before these scans, patients are educated to hold their breath for at least 20secs during the scan. This helps patients to move their heart away from chest. So, the heart moves away from the treatment field and it reduces the heart mean doses. Advanced radiation technologies have contributed to better treatment outcomes. The DIBH technique for radiation therapy of left-sided BC has been evaluated by several dosimetric studies. Our data is consistent with other published reports demonstrating a significant reduction in cardiac doses [6]. Our findings suggest that at least patients with left-sided BC benefited from the DIBH technique in terms of potentially clinically relevant dose reductions to cardiac structures. Our results consistently indicated that the inhale baseline of DIBH breathing curve decreased as the average maximum heart distance increased. Hsiao-Ming Lu et al. represented that deep inspiration minimizes the cardiac dose in the tangential treatment field, whereas absolute volume of lung in the treatment fields increases [34]. On the other hand, we found that most patients achieved relative dosimetric benefits above 50% in MHD, V20 Heart, which justifies the use of the technique. In UK, Heart Spare study, in which this technique was implemented at the national level, the referral for DIBH was dedicated to patients with any heart inside the 50% isodose in FB planning CT with standard tangential fields [5]. Such an approach would exclude patients with favourable anatomy and quite good heart and Lung sparing on FB from the use of this costly and time-consuming technique. Even a small dose decrease given to these critical structures may reduce late cardiac and vascular morbidity.
Our data represent that there is clear reduction in the cardiac doses than the doses which are treated on free breathing previously. Above-mentioned table showed that V10Gy < 5% was hardly achieved in many patients and this is soft constraint while V2Gy < 30% was achieved in all patients. Moreover, the lung dose has equal importance as the heart dose. According to institutional practice and protocol, V30 of the total dose of ipsilateral lung should be less than 25% of the total volume with (±10% margin) and our data clearly satisfy this constraint. In our practice, heart and LAD exposure clearly depended on the size and location of the tumor bed. Recently, the use of DIBH occasionally, in cases with relatively high heart or LAD doses in PBI plans, the DIBH method provided prompt solution.
Conclusion
DIBH is one of the powerful heart sparing techniques in breast cancer RT. According to our retrospective study, it is very clear from the data that deep inspiration breath hold scans are better to reduce OAR’s doses instead of free breathing scan. With DIBH, it’s possible that mean heart dose is less than 3 Gy while as deep as patient hold his breath, heart moves away from the chest which reduce the involvement of heart in the treatment field.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 25, Aug 2021Accepted: Thu 30, Sep 2021
Published: Wed 13, Oct 2021
Copyright
© 2023 Khalid Iqbal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2021.09.06
Author Info
Noreen Amjad Sumera Butt Fajar Rafi Ranjha Sajid Anees Minhas Qurat ul Ain Shamsi Khalid Iqbal
Corresponding Author
Khalid IqbalDepartment of Medical Physics, Shaukat Khanum Memorial Cancer Hospital and Research Center, Lahore, Pakistan
Figures & Tables
Table 1: OAR doses to each patient.
|
No. of Patients |
IPSILATERAL LUNG V30%
|
Mean Ipsilateral lung dose (Gy) |
Mean Heart dose (Gy) |
Heart V2 (%) |
Heart V10 (%) |
|
1 |
18.4 |
7.39 |
1.5 |
12.6 |
2 |
|
2 |
15.5 |
7.48 |
3.12 |
29.8 |
6 |
|
3 |
7.5 |
4.53 |
1.08 |
14.6 |
0.4 |
|
4 |
19.6 |
7.83 |
2.76 |
16.6 |
6 |
|
5 |
18.1 |
7.5 |
2.04 |
16.6 |
3.8 |
|
6 |
20.7 |
8.46 |
3.1 |
19.1 |
6.8 |
|
7 |
15.7 |
7.03 |
1.39 |
10 |
2 |
|
8 |
19.5 |
9.58 |
1.28 |
15.7 |
0.7 |
|
9 |
21.7 |
8.74 |
2.45 |
24.3 |
5.4 |
|
10 |
18.8 |
8.16 |
2.92 |
24 |
5 |
|
11 |
13.9 |
6.08 |
1.9 |
17.2 |
3.2 |
|
12 |
19.6 |
8.2 |
2.62 |
23.8 |
4.8 |
|
13 |
14.7 |
6.42 |
0.91 |
10.4 |
0 |
|
14 |
15.1 |
7.36 |
1.57 |
21 |
1.5 |
|
15 |
23.4 |
10.49 |
1.7 |
24.2 |
1.29 |
|
16 |
10.4 |
5.53 |
2.53 |
21.5 |
5.96 |
|
17 |
14.1 |
6.62 |
2.81 |
23.5 |
6.78 |
|
18 |
17.2 |
7.7 |
2.6 |
20 |
5.2 |
|
19 |
20.3 |
8.3 |
2.6 |
20.9 |
5.2 |
|
20 |
25.9 |
10.44 |
2.7 |
29.4 |
5.5 |
|
21 |
11 |
11 |
1.25 |
12.3 |
1.3 |
|
22 |
11 |
5.05 |
1.32 |
13 |
1.5 |
|
23 |
10.5 |
5.6 |
2.89 |
23.2 |
5.78 |
|
24 |
21.2 |
8.5 |
1.05 |
12.1 |
0 |
|
25 |
16.4 |
6.47 |
1.76 |
19.2 |
2.4 |
|
26 |
10.3 |
5.87 |
1.5 |
17 |
1.2 |
|
27 |
20.8 |
8.67 |
1.73 |
15.6 |
2.1 |
|
28 |
13.5 |
6.64 |
1.88 |
23.5 |
2.58 |
|
29 |
18.4 |
7.97 |
1.85 |
20 |
2.4 |
|
30 |
19.3 |
8.04 |
1.03 |
10.6 |
1 |



References
1. Bergom C,
Currey A, Desai N, Tai A, Strauss JB et al. (2018) Deep Inspiration Breath Hold: Techniques and
Advantages for Cardiac Sparing During Breast Cancer Irradiation. Front Oncol
8: 87. [Crossref]
2. H M Lu, E Cash, M H Chen, L Chin, W
J Manning et al. (2000) Reduction of cardiac volume in left breast treatment
fields by respiratory maneuvers: a CT study. Int J radiat Oncol Biol Phys
47: 895-904. [Crossref]
3. Remouchamps VM, Letts N, Vicini FA,
Sharpe MB, Kestin LL et al. (2003) Initial Clinical experience with moderate
deep inspiration breath hold using an active breathing control device in the
treatment of patients with left sided breast cancer using external beam
radiation therapy. Int J radiat Oncol Biol Phy 56: 704-715. [Crossref]
4. Taylor CW, Kirby AM
(2015) Cardiac side-efects from breast cancer radiotherapy. Clin Oncol (R
Coll Radiol) 27: 621-629. [Crossref]
5. Shah C, Tendulkar
R, Smile T, Nanavati A, Manyam B et al. (2016) Adjuvant radiotherapy in
early-stage breast cancer: evidence-based options. Ann Surg Oncol 12:
3880-3890. [Crossref]
6. Bartelink H (2019)
Regional nodal irradiation for early breast cancer; clinical benefit according
to risk stratification. Breast 48: S65-S68. [Crossref]
7. Whelan TJ, Olivotto
IA, Parulekar WR, Ackerman I, Chua BH et al. (2015) Regional Nodal Irradiation
in Early-Stage Breast Cancer. New Engl J Med 373: 307-316. [Crossref]
8. Darby SC, McGale P,
Taylor CW, Peto R (2005) Long-term mortality from heart disease and lung cancer
after radiotherapy for early breast cancer: prospective cohort study of about
300,000 women in US SEER cancer registries. Lancet Oncol 6: 557-565. [Crossref]
9. Darby SC, Ewertz M,
McGale P, Bennet AM, Blom Goldman U et al. (2013) Risk of ischemic heart
disease in women after radiotherapy for breast cancer. N Engl J Med 368:
987-998. [Crossref]
10. Taylor C, McGale P,
Brønnum D, Correa C, Cutter D et al. (2018) Cardiac structure injury after
radiotherapy for breast cancer: cross-sectional study with individual patient
data. J Clin Oncol 36: 2288-2296. [Crossref]
11. Taylor C, Correa C,
Duane FK, Aznar MC, Anderson SJ et al. (2017) Estimating the Risks of Breast
Cancer Radiotherapy: Evidence from Modern Radiation Doses to the Lungs and
Heart and From Previous Randomized Trials. J Clin Oncol 35: 1641-1649. [Crossref]
12. Aznar MC, Duane FK,
Darby SC, Wang Z, Taylor CW (2018) Exposure of the lungs in breast cancer
radiotherapy: a systematic review of lung doses published 2010-2015. Radiother
Oncol 126: 148-154. [Crossref]
13. Andratschke N,
Maurer J, Molls M, Trott KR (2011) Late radiation-induced heart disease after
radiotherapy. Clinical importance, radiobiological mechanisms and strategies of
prevention. Radiother Oncol 100: 160-166. [Crossref]
14. van den Bogaard VA,
Ta BD, van der Schaaf A, Bouma AB, Middag AM et al. (2017) Validation and modification
of prediction model for acute cardiac events in patients with breast cancer
treated with radiotherapy based on three-dimensional dose distributions to
cardiac substructures. J Clin Oncol 35: 1171-1178. [Crossref]
15. Jacobse JN, Duane
FK, Boekel NB, Schaapveld M, Hauptmann M et al. (2019) Radiation dose-response
for risk of myocardial infarction in breast cancer survivors. Int J Radiat
Oncol Biol Phys 103: 595-604. [Crossref]
16. Varga Z, Hideghéty
K, Mező T, Nikolényi A, Thurzó L et al. (2009) Individual positioning: a
comparative study of adjuvant breast radiotherapy in the prone versus supine
position. Int J Radiat Oncol Biol Phys 75: 94-100. [Crossref]
17. Varga Z, Cserháti
A, Rárosi F, Boda K, Gulyás G et al. (2014) Individualized positioning for
maximum heart protection during breast irradiation. Acta Oncol 53:
58-64. [Crossref]
18. Kahán Z, Rárosi F,
Gaál S, Cserháti A, Boda K et al. (2018) A simple clinical method for
predicting the benefit of prone vs supine positioning in reducing heart
exposure during left breast radiotherapy. Radiother Oncol 126: 487-492. [Crossref]
19. Sixel KE, Aznar MC,
Ung YC (2001) Deep inspiration breath hold to reduce irradiated heart volume in
breast cancer patients. Int J Radiat Oncol Biol Phys 49: 199-204. [Crossref]
20. Lai J, Hu S, Luo Y,
Zheng R, Zhu Q et al. (2020) Meta-analysis of deep inspiration breath hold
(DIBH) versus free breathing (FB) in postoperative radiotherapy for left-side
breast cancer. Breast Cancer 27: 299-307. [Crossref]
21. Latty D, Stuart KE,
Wang W, Ahern V (2015) Review of deep inspiration breath-hold techniques for
the treatment of breast cancer. J Med Radiat Sci 62: 74-81. [Crossref]
22. Dell’Oro M, Giles
E, Sharkey A, Borg M, Connell C et al. (2019) A retrospective dosimetric study
of radiotherapy patients with left-sided breast cancer; patient selection
criteria for deep inspiration breath hold technique. Cancers (Basel) 11:
259. [Crossref]
23. Bartlett FR, Colgan
RM, Carr K, Donovan EM, McNair HA et al. (2013) The UK HeartSpare study:
randomised evaluation of voluntary deep-inspiratory breath-hold in women
undergoing breast radiotherapy. Radiother Oncol 108: 242-247. [Crossref]
24. Akram M, Iqbal K, Isa M, Afzal M, Buzdar S (2014) Optimum
reckoning of contra lateral breast dose using physical wedge and enhanced
dynamic wedge in radiotherapy treatment planning system. Int J Radiat Res
12: 295-302.
25. Ofersen BV, Boersma
LJ, Kirkove C, Hol S, Aznar MC et al. (2015) ESTRO consensus guideline on target
volume delineation for elective radiation therapy of early stage breast cancer.
Radiother Oncol 114: 3-10. [Crossref]
26. Shaw E, Kline R,
Gillin M, Souhami L, Hirschfeld A et al. (1993) Radiation therapy oncology
group: radiosurgery quality assurance guidelines. Int J Radiat Oncol Biol
Phys 27: 1231-1239. [Crossref]
27. Csenki M, Újhidy D,
Cserháti A, Kahán Z, Varga Z (2014) Radiation dose to the nodal regions during
prone versus supine breast irradiation. Ther Clin Risk Manag 10:
367-372. [Crossref]
28. Lin H, Liu T, Shi
C, Petillion S, Kindts I et al. (2018) Feasibility study of individualized optimal
positioning selection for left-sided whole breast radiotherapy: DIBH or prone. J
Appl Clin Med Phys 19: 218-229. [Crossref]
29. Tanna N, McLauchlan
R, Karis S, Welgemoed C, Gujral DM et al. (2017) Assessment of upfront
selection criteria to prioritise patients for breath-hold left-sided breast
radiotherapy. Clin Oncol (R Coll Radiol) 29: 356-361. [Crossref]
30. Wikström K,
Isacsson U, Nilsson K, Ahnesjö A (2018) Reproducibility of heart and thoracic
wall position in repeated deep inspiration breath holds for radiotherapy of
left-sided breast cancer patients. Acta Oncol 57: 1318-1324. [Crossref]
31. Zhao F, Shen J, Lu
Z, Luo Y, Yao G et al. (2018) Abdominal DIBH reduces the cardiac dose even
further: a prospective analysis. Radiat Oncol 13: 116. [Crossref]
32. Piroth MD, Baumann
R, Budach W, Dunst J, Feyer P et al. (2019) Heart toxicity from breast cancer
radiotherapy. Current findings, assessment, and prevention. Strahlenther
Onkol 195: 1-2. [Crossref]
33. Zurl B, Stranzl H,
Winkler P, Kapp KS (2010) Quantitative assessment of irradiated lung volume and
lung mass in breast cancer patients treated with tangential fields in
combination with deep inspiration breath hold (DIBH). Strahlenther Onkol
186: 157-162.
[Crossref]
34. Lu HM, Cash E, Chen MH, Chin L,
Manning WJ et al. (2000) Reduction of cardiac
volume in left breast treatment fields by respiratory maneuvers: a CT study. Int J Radiat Oncol Biol Phys 47: 895-904. [Crossref]
35. Sakyanun P, Saksornchai K,
Nantavithya C, Chakkabat C, Shotelersuk K (2020) The effect of deep inspiration
breath hold technique on left anterior descending coronary artery and heart
dose in left breast irradiation. Radiat Oncol J 38:181-188. [Crossref]
36. Chen GP, Liu F, White J, Vicini FA, Freedman GM et al. (2015) A planning comparison of 7 irradiation options allowed in RTOG 1005 for early-stage breast cancer. Med Dosim 40: 21-25. [Crossref]
37. Tanguturi SK, Lyatskaya Y, Chen Y, Catalano PJ, Chen MH et al. (2015) Prospective assessment of deep inspiration breath hold using 3-dimensional surface tracking for irradiation of left-sided breast cancer. Pract Radiat Oncol 5: 358-365. [Crossref]
