Journals
Dietary Magnesium Intake and Heart Health
A B S T R A C T
With magnesium being the second most common intracellular cation in the human body and the presence of hypomagnesemia in 10% of hospital admissions, magnesium deficiency has become a clinically significant nutritional deficiency in context of heart health. Magnesium has long been used as a treatment modality for cardiac arrhythmias as serum magnesium concentration of 1.44 mEq/L to 1.8 mEq/L has been found to have a statistically significant inverse association with cardiovascular disease events. Patients with the highest intake of magnesium were found to have incidents of sudden cardiac death reduced by 77% while hypomagnesemia is found to be associated with increased risk of congestive heart failure and cardiac arrhythmias. It has also been demonstrated that high dietary intake of serum magnesium is associated with decrease in systolic and diastolic blood pressure secondary to reduction in vascular tone and an increase in vasodilatory substances, like Prostaglandin E. Association of cardiovascular diseases with hypomagnesemia and the need for the fulfilment of RDA goals, authenticates the use of oral magnesium supplements, with established safety profile and lack of potential for toxicity.
K E Y W O R D S
Magnesium, recommended daily allowance, dietary intake, cation, hypomagnesemia, cardiovascular disease, hypertension, arrhythmia, atrial fibrillation, ventricular arrhythmia, heart failure
Abbreviations:
magnesium (Mg), cardiovascular disease events (CVDE), blood pressure (BP), hypertension (HTN), recommended daily allowances (RDAs), premature ventricular complex (PVC).
Introduction
Magnesium (Mg) is one of the top ten elements found on earth’s surface while high concentration of biologically active magnesium reserves are found in water bodies with concentrations as high as 198 mmol/L [1, 2]. Following calcium, sodium and potassium it is the most common mineral in the human body and the second most common cation that is present intracellularly [3]. Magnesium plays a vital role in the human enzymatic machinery as a cofactor in more than 300 enzymatic reactions [1, 4]. As a cation, it not only supports ATPases but also plays its role in transmembrane transport and anaerobic phosphorylation [5]. On a cellular level, reserves of Mg are found inside the mitochondria and it can potentially bind with 3571 human proteins [3]. In an average adult weighing 70 kg, total body stores of magnesium are equivalent to 24-25 grams with 53%, 27%, 19% and < 1% in bones, muscles, soft tissues and blood respectively with a half-life of 42 days [1, 3].
Method
This literature review is a study of previous peer reviewed articles on magnesium, its dietary intake and its association with cardiovascular diseases, specifically congestive heart failure, cardiac arrhythmias and hypertension. This review tries to compile the effects of magnesium on the above-mentioned cardiac pathologies. PubMed, google scholar, science direct and medicine textbook were utilized to gather contextual information on magnesium from peer reviewed sources, its effect on cardiovascular system and numerical and statistical data relating to clinical trials. Data was also collected from National Institutes of Health, Office for Dietary Supplements for analysis and was used to create figures 1 and 2.
Nutrition and Bioavailability
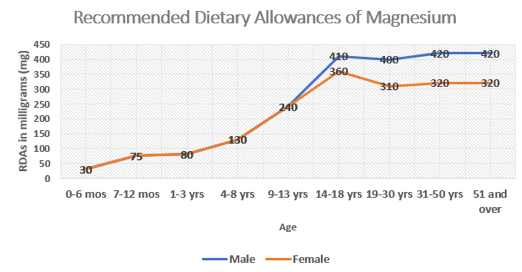
Being the fourth most copious mineral found in the human body, magnesium is naturally found or seen as an add-on in numerous food products [4, 6]. Magnesium deficiency, as defined as serum concentration < 1.5 mEq/L, is frequently seen in clinical practice with as high as 10% of patients presenting with magnesium deficiency [7]. Magnesium deficiency can be multifactorial, however, it has been demonstrated that decreased intake of foods fortified with Mg or Mg deficient natural food products play a significant role [8]. Dietary surveys in the United States indicate lower than recommended intake of magnesium in the general population [6]. While magnesium should be consumed on a daily basis to avoid deficiency, an exact intake value has been challenging to be established [1]. Reported recommended dosages are accustomed to age, sex and nutritional status, however, the Institute of Medicine suggests 310-360 mg and 400-420 mg for adult men and women with variations in Recommended Dietary Allowances (RDAs) for specific ages and for women during gestational and lactating periods [1, 6] (figure 1).
Figure 1: RDAs according to sex and age, reference 6
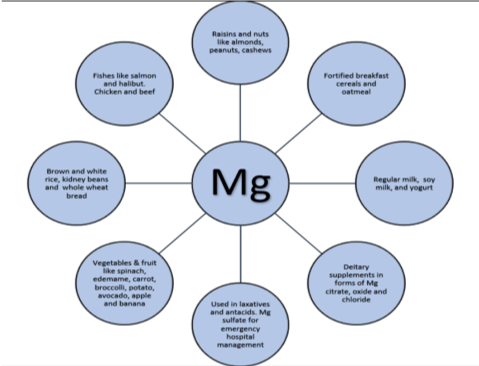
While magnesium is naturally consumed through fruits, vegetables, nuts, seeds and whole grains, it is also added to foods like cereals and several beverages [6]. Magnesium is also widely available in dietary supplements in three different forms, including, magnesium oxide, citrate and chloride [6]. Water solubility of magnesium is a strong indicator of absorption as magnesium aspartate, citrate, lactate and chloride have better absorption in gut mucosa with higher bioavailability as compared to that of magnesium oxide and sulphate [6]. Apart from being available as a dietary supplement, magnesium is also found to be a key ingredient in few medicines like laxatives and antacids, which aid in treating heartburn, indigestion and constipation [6]. Magnesium in sulphate form is used as a primary treatment agent to manage cases of preeclampsia and eclampsia [9] (figure 2). Magnesium has also been used as a therapeutic agent in cardiac arrhythmias while hypomagnesemia is also found to be associated with other cardiac pathologies [5, 8, 10]. American Medical Association recommendations for prevention of cardiovascular disease includes established targets of Mg intake to be met on a daily basis [11]. Magnesium intake either as a supplement to meet RDA requirements or as a preventive agent in oral form is generally considered quite safe without any major potential for toxicity [12].
Figure 2: RDAs according to sex and age, reference 6
Magnesium and cardiovascular disease
Among numerous physiological roles of Mg, its cardioprotective role is noteworthy and has been a matter of debate. A comprehensive literature review on Mg and risk of cardiovascular disease was carried out by Qu at el. Due to absence of randomized clinical trials a meta-analysis was conducted to ascertain association, if any exists, between risk of cardiovascular disease events (CVDE) and dietary intake and serum Mg levels [11]. Multiple variables were calculated to establish the validity of analysis. It was found that Mg dietary usage and serum levels were associated with 15% and 20% lower risk of cardiovascular events respectively [11]. Those with high intake of Mg had 15% less chance of CVDE with relative risk of 0.85 and 95% confidence interval (CI) between 0.78 to 0.92 with a statistically significant P value [11]. Similarly, those with higher blood levels of Mg had a 20% less chance of CVDE with relative risk of 0.77 and CI between 0.66 to 0.87 with a statistically significant P value [11]. Specifically, serum Mg value from 1.44 mEq/L to 1.8 mEq/L was found to have a linear decrease in CVDE [11].
Magnesium along with its numerous pivotal enzymatic functions on a cellular level plays a significant role on cardiac tissue. Congestive heart failure, arrhythmias and hypertension (HTN) are all associated with serum magnesium levels and its dietary intake. It has been observed that patients with highest intake of magnesium had a decrease in sudden cardiac death by 77% [13, 14].
Congestive Heart Failure
Decreased levels of serum magnesium may be responsible for lack of a favourable prognosis in heart failure. Hypomagnesemia causes decrease in cardiac contractility and increased vascular tone, both of which can result in worsening of clinically established heart failure [5]. Based on various studies the relationship of hypomagnesemia with congestive heart failure is quite evident with hypomagnesemia ranging from 19% to as high as 55% of heart failure cases [5]. Pharmacologic interventions in heart failure are primarily directed towards decreasing volume overload and sometimes increasing cardiac contractility, which by default is achieved by the decrease in volume overload [15-17]. The primary modality used in decreasing overall volume overload as well as improving pulmonary edema secondary to congestive heart failure is a diuretic named furosemide [16, 17]. Furosemide is also found to increase magnesium loss through increasing renal excretion of magnesium, which in turn would worsen already established hypomagnesaemia in congestive heart failure [5, 18]. Cohen et al. carried out a study to evaluate hypomagnesemia and hypermagnesemia in heart failure patients in context of various pre-pathology variables relating to heart failure and treatment with furosemide. Study demographics comprised of 404 patients with congestive heart failure class II-IV as per New York Heart Association (NYHA) guidelines [5]. All 404 patients were receiving furosemide 40mg or more for a duration of more than 3 months. Hypomagnesemia, hypermagnesemia and normal serum Mg levels were found in 12.3%, 4.9% and 82.6% respectively [5]. Although most patients had normal serum Mg levels, a significant proportion of patients also had hypomagnesemia, which on its own was a concerning finding. Hypomagnesemia was found to be associated with other abnormalities including female gender, diabetes, low serum sodium, high fever and hypocalcemia [5]. The finding of hypocalcemia was an outlier as Mg replaces calcium and lower serum Mg should be associated with hypercalcemia [18]. Overall it was demonstrated that hypomagnesemia plays an inhibitory function on cardiac contractility, catecholamine release and vascular resistance, hence playing an important prognostic role [5]. Electrolyte abnormalities secondary to heart failure or treatment of heart failure with furosemide or other medications such as digitalis or ACE inhibitors are a common occurrence in clinical medicine and Mg supplementation can play a significant role in protecting from hemodynamic instability [19, 20]. Various other studies have also demonstrated that low serum magnesium and intake of < 2.3 mg/kg is associated with increased risk of heart failure [21-23]. There is a further need to evaluate whether hypomagnesemia in heart failure patients is secondary to the underlying pathology or its treatment or hypomagnesemia itself is a contributing etiology.
Arrhythmias
Cardiac rhythm disorders are a common finding in clinical practice and can be secondary to various etiologies including conduction defects, disorders of impulse generation, genetic causes, endocrine pathology, previous cardiac pathology, like coronary artery disease or heart failure and electrolyte abnormalities [24-26]. Numerous studies have evaluated the role of magnesium in maintaining cardiac rhythm and preventing arrhythmias. Magnesium’s effect on heart rhythm is most likely secondary to its physiological function by inhibiting calcium channels in the atrioventricular (AV) node, which serves as the midway point of the cardiac conduction pathway, whereas hypomagnesemia decreases potassium levels in cardiac muscle intracellularly, which can result in arrhythmia [27]. A significant number of patients with arrhythmias have decreased serum magnesium levels [28]. Gobbo et al. conducted a study of 750 diabetic adult participants to evaluate an association, if any exists, between serum magnesium levels and the presence of premature ventricular complex (PVC) on Holter monitoring. PVCs are common in general population and can be secondary to cardiac rhythm disorder or present as a benign occurrence [29]. Although PVCs are not usually treated aggressively in clinical practice as some of the other arrhythmias, it is still considered an arrhythmia by definition i.e. irregular heart rhythm. The study concluded that patients with hypomagnesemia, as defined by magnesium levels below ≤ 0.70 mmol/L, had 2x occurrence of PVCs as compared to adults with normal serum magnesium levels [27]. Magnesium supplementation has also been shown to reduce the incidence of arrhythmias that arise after cardiac surgeries including coronary artery bypass graft [30-32].
Role of magnesium is already established and utilized as a treatment modality in ventricular arrhythmia referred to as torsade de pointes [8, 10]. Similarly, magnesium also has a role in management of atrial fibrillation, as a therapeutic option [33, 34]. Besides for the therapeutic role of magnesium in acute arrhythmias, the role of oral magnesium supplementation as preventive modality for arrhythmia need to be further analyzed in context of hypomagnesemia as a cause of irregular rhythm. Khan et al. carried out a cohort study of 3530 participants from the Framingham Offspring Study, a derivative of Framingham Heart Study of 1948. The study found a statistically significant association with low serum magnesium levels and the development of atrial fibrillation [35]. Although a linear relationship was not observed between hypomagnesemia and atrial fibrillation, it was observed that below a certain cutoff limit of serum magnesium level, there was an association of hypomagnesemia and atrial fibrillation [35]. In light of Khan et al. and Del Gobbo et al. studies it is quite evident that hypomagnesemia should be corrected by oral magnesium supplementation to prevent cardiac rhythm disorders. According to recommendations made by German Society of Magnesium Research, supplementation of Mg can be used as a modality with or without other agents in management and prevention of rhythm disorders [12].
Hypertension
Clinically, hypertension (HTN) is defined as a rise in blood pressure (BP) to a level that requires therapeutic intervention. Stage 1 hypertension occurs when systolic pressure rises above 139 mm Hg and diastolic pressure rises above 89 mm Hg [36]. Besides from affecting over a billion people worldwide and causing approximately 9.4 million deaths per year, hypertension is a major contributing factor in the pathogenesis of other cardiovascular diseases [36]. There is an obvious association of genetics to hypertension, as well as many environmental factors are found to have an effect [37]. While majority of these factors play a role in causing hypertension, magnesium is found to have beneficial effect in maintaining vascular hemodynamics. According to studies with relevant experimental and statistically significant data, magnesium is found to have a regulatory effect on the blood pressure. Magnesium helps in lowering the blood pressure through different mechanisms. Physiologically magnesium inhibits calcium channels similarly to therapeutic agents used for hypertension and decreases intracellular calcium levels. It also aids in the release and synthesis of Prostaglandin E, which is responsible for decreasing vascular tone and vasodilation [38].
One of the earliest collected clinical data on a trial of low dose magnesium supplement and its effect on HTN was reported by Dyckner and Wester [39]. As per Sun Ha Jee et al., since than many other clinical trials have demonstrated inconsistent data due to the use of relatively smaller dose of magnesium [39]. Experimental trials consisting of magnesium administration of 10 -15 mmol/day did not produce substantial effects [39]. According to Houston 2011, magnesium in larger quantities ranging from 500 mg/d to 1000 mg/d resulted in blood pressure reduction of 5.6/2.8 mm Hg [38]. A meta-analysis clinical trial by Sun Ha Jee et al conducted 20 studies with a total of 1220 participants consisting of both hypertensive and normotensive subjects [39]. The dose of Mg used for the clinical trial was 10 to 40 mmol/d, which produced only a minor decrease in the blood pressure, which they hypothesized, was due to the use of low dose of Mg [39].
A study by Witteman et al. demonstrated a substantial decrease in systolic BP by 2.7 mm Hg and diastolic BP by 3.4 mm Hg with the use of 20 mmol/d (485 mg) of magnesium aspartate, likewise, similar study of 40 participants with 600 mg/d of magnesium intake showed a vital reduction in systolic and diastolic BP by 5.6/2.8 mmHg [38]. A study by Atherosclerosis Risk in Communities (ARIC) found a positive association of decreased prevalence of HTN, diabetes mellitus and ischemic cerebrovascular accident to a higher level of serum magnesium and its consumption in people [38]. Taking in consideration the past clinical studies it is quite evident that higher magnesium supplementation results in more pronounced reduction in both systolic and diastolic blood pressure reductions as compared to those studies that used smaller quantities of magnesium, which had none to insignificant results. While through various studies magnesium is found to be influential in higher doses in patients with conditions strongly relating to vascular hypertension, i.e. preeclampsia and glomerulonephritis and has shown to help increase the efficacy of antihypertensive drugs, but it is yet to be proven whether or not it can effectively treat or aid in prevention of CVDE secondary to HTN [38, 39].
Conclusion
Hypomagnesemia is a clinically significant nutritional deficiency that needs to be addressed to promote heart health. Hypomagnesemia is found to be associated with cardiac arrhythmias and congestive heart failure, whereas supplementary oral dietary intake of magnesium has been proven to lower systolic vascular and diastolic pressure. American Medical Association recommends fulfilment of dietary intake of magnesium as a preventive measure for cardiovascular diseases. With good safety profile of oral magnesium supplementation and low risk of toxicity, further research comprising of clinical trials utilizing higher quantities of Mg are required to analyze daily intake goals and use of magnesium supplementation as a treatment modality, as well as a dietary supplement.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 10, Sep 2018Accepted: Tue 02, Oct 2018
Published: Tue 06, Nov 2018
Copyright
© 2023 David O. Carpenter. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JFNM.2018.01.001
Author Info
David O. Carpenter Rija Zehra Syed S. Fatmi
Corresponding Author
David O. CarpenterInstitute for Health and the Environment; University at Albany, SUNY, Rensselaer, NY, USA
Figures & Tables
References
1. Jahnen-Dechent W, Ketteler M (2012) Magnesium basics. Clin Kidney J 5: 3-14. [Crossref]
2. Bodaker I, Sharon I, Suzuki MT, Feingersch R, Shmoish M, et al. (2010) Comparative community genomics in the Dead Sea: an increasingly extreme environment. ISME J 4: 399-407. [Crossref]
3. Schwalfenberg GK, Genuis SJ (2017) The Importance of Magnesium in Clinical Healthcare. Scientifica (Cairo) 2017: 4179326. [Crossref]
4. Swaminathan R (2003) Magnesium metabolism and its disorders. Clin Biochem Rev 24: 47-66. [Crossref]
5. Cohen N, Almoznino-Sarafian D, Zaidenstein R, Alon I, Gorelik O, et al. (2003) Serum magnesium aberrations in furosemide (frusemide) treated patients with congestive heart failure: pathophysiological correlates and prognostic evaluation. Heart 89: 411-416. [Crossref]
6. National Institutes of Health, Office of Dietary Supplements, Magnesium — Health Professional Fact Sheet [Internet]. [cited 2018 Sep 8].
7. Abbott LG, Rude RK (1993) Clinical manifestations of magnesium deficiency. Miner Electrolyte Metab 195: 314-22. [Crossref]
8. Guerrera MP, Volpe SL, Mao JJ (2009) Therapeutic uses of magnesium. Am Fam Physician 80: 157-162.
9. Thapa K, Jha R. Magnesium sulphate: a lifesaving drug. JNMA J Nepal Med Assoc 47: 104-108. [Crossref]
10. Tzivoni D, Keren A (1990) Suppression of ventricular arrhythmias by magnesium. Am J Cardiol 65: 1397-1399. [Crossref]
11. Qu X, Jin F, Hao Y, Li H, Tang T, et al. (2013) Magnesium and the Risk of Cardiovascular Events: A Meta-Analysis of Prospective Cohort Studies. PLoS One 8: e57720. [Crossref]
12. Vierling W, Liebscher D-H, Micke O, von Ehrlich B, Kisters K (2013) Magnesiummangel und Magnesiumtherapie bei Herzrhythmusstörungen. DMW - Dtsch Medizinische Wochenschrift 138: 1165-1171.
13. Chiuve SE, Korngold EC, Januzzi JL, Gantzer M Lou, Albert CM (2011) Plasma and dietary magnesium and risk of sudden cardiac death in women. Am J Clin Nutr 93: 253-260. [Crossref]
14. Chiuve SE, Sun Q, Curhan GC, Taylor EN, Spiegelman D, et al. (2013) Dietary and Plasma Magnesium and Risk of Coronary Heart Disease Among Women. J Am Heart Assoc 2: e000114-e000114. [Crossref]
15. Jameson JL, Kasper D, Longo D, Fauci A, Hauser S, et al. (2018) Disorders of the Cardiovascular System, Heart Failure: Managment. In: HARRISON’S PRINCIPLES OF INTERNAL MEDICINE. 20th ed. McGraw-Hill Education 1769-1778.
16. Jameson JL, Kasper D, Longo D, Fauci A, Hauser S, et al. (2018) Disorders of the Cardiovascular System, ST-Segment Elevation Myocardial Infarction. In: HARRISON’S PRINCIPLES OF INTERNAL MEDICINE. 20th ed. McGraw-Hill Education 1881-1882.
17. Jameson JL, Kasper D, Longo D, Fauci A, Hauser S, et al. (2018) Critical Care Medicine. In: HARRISON’S PRINCIPLES OF INTERNAL MEDICINE. 20th ed. McGraw-Hill Education 2057.
18. Jameson JL, Kasper D, Longo D, Fauci A, Hauser S, et al. (2018) Endocrinology and Metabolism, Magnesium Metabolism. In: HARRISON’S PRINCIPLES OF INTERNAL MEDICINE. 20th ed. McGraw-Hill Education 2916-2918.
19. Douban S, Brodsky MA, Whang DD, Whang R (1996) Significance of magnesium in congestive heart failure. Am Heart J 132: 664-671. [Crossref]
20. Gottlieb SS (1989) Importance of magnesium in congestive heart failure. Am J Cardiol 63: 39-42. [Crossref]
21. Taveira TH, Ouellette D, Gulum A, Choudhary G, Eaton CB, et al. (2016) Relation of Magnesium Intake with Cardiac Function and Heart Failure Hospitalizations in Black AdultsCLINICAL PERSPECTIVE. Circ Hear Fail 9: e002698. [Crossref]
22. Shaikh S, Karira KA (2011) Magnesium deficiency in heart failure patients with diabetes mellitus. J Pak Med Assoc 61: 901-903.
23. Lutsey PL, Alonso A, Michos ED, Loehr LR, Astor BC, et al. (2014) Serum magnesium, phosphorus, and calcium are associated with risk of incident heart failure: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Clin Nutr 100: 756-764. [Crossref]
24. Jameson JL, Kasper D, Longo D, Fauci A, Hauser S, et al. Principles of Electrophysiology. In: HARRISON’S PRINCIPLES OF INTERNAL MEDICINE. 20th ed. McGraw-Hill Education 1716-1762.
25. Parmley WW (1987) Factors causing arrhythmias in chronic congestive heart failure. Am Heart J 114: 1267-1272. [Crossref]
26. Antzelevitch C, Burashnikov A (2011) Overview of Basic Mechanisms of Cardiac Arrhythmia. Card Electrophysiol Clin 3: 23-45. [Crossref]
27. Del Gobbo LC, Song Y, Poirier P, Dewailly E, Elin RJ, et al. (2012) Low serum magnesium concentrations are associated with a high prevalence of premature ventricular complexes in obese adults with type 2 diabetes. Cardiovasc Diabetol 11: 23. [Crossref]
28. Ganga HV, Noyes A, White CM, Kluger J (2013) Magnesium Adjunctive Therapy in Atrial Arrhythmias. Pacing Clin Electrophysiol 36. [Crossref]
29. Latchamsetty R (2017) Clinical Significance of Idiopathic Frequent Premature Ventricular Complexes. US Cardiol Rev 11: 95.
30. Lee HY, Ghimire S, Kim EY (2013) Magnesium Supplementation Reduces Postoperative Arrhythmias After Cardiopulmonary Bypass in Pediatrics: A Metaanalysis of Randomized Controlled Trials. Pediatr Cardiol 34: 1396-403. [Crossref]
31. Shiga T, Wajima Z, Inoue T, Ogawa R (2004) Magnesium prophylaxis for arrhythmias after cardiac surgery: A meta-analysis of randomized controlled trials. Am J Med 117: 325-333. [Crossref]
32. Wilkes NJ, Mallett S V, Peachey T, Di Salvo C, Walesby R (2002) Correction of ionized plasma magnesium during cardiopulmonary bypass reduces the risk of postoperative cardiac arrhythmia. Anesth Analg 95: 828-834. [Crossref]
33. Kotecha D (2016) Magnesium for Atrial Fibrillation, Myth or Magic? Circ Arrhythmia Electrophysiol 9: e004521. [Crossref]
34. Abdel-Massih TE, Sarkis A, Sleilaty G, El Rassi I, Chamandi C, et al. (2012) Myocardial extraction of intracellular magnesium and atrial fibrillation after coronary surgery. Int J Cardiol 160: 114-118. [Crossref]
35. Khan AM, Lubitz SA, Sullivan LM, Sun JX, Levy D, et al. (2013) Low serum magnesium and the development of atrial fibrillation in the community: the Framingham Heart Study. Circulation 127: 33-38. [Crossref]
36. Jameson JL, Kasper D, Longo D, Fauci A, Hauser S, et al. (2018) Hypertensive Vascular Disease. In: HARRISON’S PRINCIPLES OF INTERNAL MEDICINE. 20th ed. McGraw-Hill Education 1890-1895.
37. Williams RR, Hunt SC, Hasstedt SJ, Hopkins PN, Wu LL, et al. (1991) Are there interactions and relations between genetic and environmental factors predisposing to high blood pressure? Hypertension 18: I29–I29. [Crossref]
38. Houston M (2011) The Role of Magnesium in Hypertension and Cardiovascular Disease. J Clin Hypertens 13: 843-847. [Crossref]
39. Jee SH, Miller ER, Guallar E, Singh VK, Appel LJ, et al. (2002) The effect of magnesium supplementation on blood pressure: a meta-analysis of randomized clinical trials. Am J Hypertens 15: 691-696. [Crossref]
