Endodontic Treatment of a Mandibular Molar with Radix Paramolaris: A Case Report
A B S T R A C T
Anatomical variations of the root canal system of mandibular molars are common and often present challenges for endodontic treatment. In some cases, an additional root is located in the distolingual, radix entomolaris (RE), or more rarely in the buccal, radix paramolaris (RP). This case report illustrates rare nonsurgical retreatment of the complex root canal morphology of a RP and demonstrates the utility of cone-beam computed tomography (CBCT) and 3D printing in managing such a case. Underscored is the need for clinicians to understand the possible variations of root canal morphology of mandibular molars and the role CBCT imaging can play in addition to periapical radiographs in order to successfully treat a tooth with radix paramolaris.
Keywords
Radix paramolaris, 3D printing, root canal anatomy, cone-beam computed tomography
Introduction
Efficient and effective root canal treatment obviously requires an understanding of root canal anatomy. Typically, mandibular molars have two roots, and they most commonly present with two canals in the mesial root and one or 2 canals in the distal root [1]. However, other root canal morphologies have been reported in the literature [2, 3]. As first mentioned by Carabelli, additional roots may be located in the distolingual, termed radix entomolaris (RE), or in the buccal, termed radix paramolaris (RP) [4, 5]. The classic study by Carlsen and Alexandersen found just 2 cases with separate RP in their collection of mandibular molars with extra root (n=203 total), collected in Denmark over almost 30 years [6].
A more frequent occurrence of RE has been linked to Chinese ethnic groups, while RE has been found in less than 5% Caucasian, Eurasian, and Indian populations. In populations with Mongoloid traits, there is an occurrence RE of 5-30%. In contrast, RP is much less frequent. For example, Visser had found the occurrence to be 0% in the first mandibular molars, 0.5% in the second, and 2% in the third [7].
Similarly, a more recent study based on cone-beam image acquisition in an Indian population found RP in first and second molars in 2/299 and 5/322 cases, respectively [8]. Another recent study described the prevalence in an Iranian population as 1.2% in first and 0.8% in second molars [9]. While there is a growing body of evidence on the prevalence of 3-rooted canal configuration in mandibular molars, only scarce information is available to describe the clinical management of radix paramolaris cases. This case report illustrates the utility of cone-beam computed tomography (CBCT) and 3D printing in the nonsurgical retreatment of a case with RP and a failing root canal treatment.
Report
A 43-year-old woman visiting from Egypt was referred in May 2016 for evaluation and treatment of a left mandibular second molar (tooth #18). The patient had a chief complaint of pain in chewing on tooth #18 since the completion of previous root canal therapy; her medical history was non-contributory. The tooth had been root canal-treated by another endodontist 5 months prior. After the initial root canal treatment, the patient continued to experience pain in chewing. According to the patient, the pain had increased in intensity during the last 3 weeks. The referring general dentist was reluctant to proceed with placing the final restoration and further treatment by an endodontist (SE) was initiated.
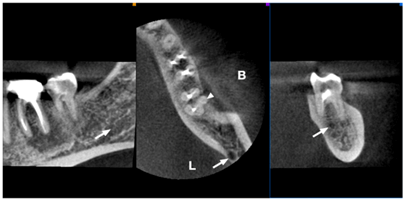
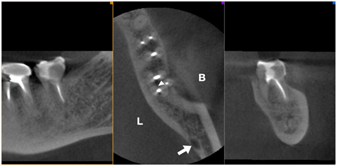
The consultation included a periapical radiograph, a bitewing radiograph of tooth #18, and a small field CBCT (Carestream 9000, Kodak, Rochester, NY). The CBCT imaging revealed an untreated buccal root canal system in tooth #18 (Figure 1) that was not evident in the periapical radiograph (Figure 2A). Nonsurgical root canal retreatment was initiated and completed during the same visit. Under magnification and guided by the CBCT image, 3 canal orifices were located. Gutta-percha root canal fillings were removed using both hand and nickel-titanium rotary files. The canal orifice associated with the buccal radix was located and instrumented along with the previously treated mesial and distal root canals. Irrigation was performed with 5.25% sodium hypochlorite solution. Gutta-percha cones were fitted and obturation was completed using Kerr EWT root canal sealer (Kerr, Brea, CA) using the warm vertical compaction technique. A composite buildup was placed using a dual-cure composite (Rock Core, Danville Materials, San Ramon, CA).
Figure 1: Selected axial views of a preoperative CBCT scan of the left mandible. B and L denote buccal and lingual aspects, respectively and the location of the mandibular canal is identified by the arrow. Note the presence of the unfilled canal associated with the radix paramolaris (arrowhead).
Figure 2: Radiographic assessment of the posterior left mandible and tooth #18. A) Preoperative periapical radiograph of #18. Radix paramolaris (RP) is not evident on conventional periapical radiograph. B) Sagittal preoperative CBCT slice demonstrating bifurcation of the inferior alveolar canal with the accessory canal in intimate proximity to the distal-lingual root in sagittal view. C) Postoperative radiograph of #18 showing obturated canal in RP (radix paramolaris).
A postoperative periapical radiograph (Figure 2B) and a postoperative CBCT (Figure 3) were taken to evaluate the quality of the root canal retreatment. The patient was contacted by phone 24 hours postoperatively and reported decreased pain to chew. At a 2-week follow-up appointment, the patient’s symptoms had completely resolved. The patient was instructed to return to her dentist for a cuspal coverage restoration. The patient returned to Egypt and was unavailable for additional follow-up.
Figure 3: Selected axial views of a postoperative CBCT scan of the left mandible. B and L denote buccal and lingual aspects. Note the now filled canal in the radix paramolaris (arrowhead).
Discussion
Radix paramolaris (RP) is a rare anatomical variant for mandibular molar anatomy [4]. Indeed, a current literature search revealed only two case reports [10, 11]. On the other hand, additional roots are found in mandibular molars. Radix entomolaris (RE) occurs most often in mandibular first molars and while a few cases of RP are found in mandibular second molars. Practicing dentists should be aware of these morphologies when treating mandibular molars. The additional root is often difficult to identify on periapical radiographs. There is clinical evidence that untreated canals such as those in a RE may result in reduced outcomes [12, 13]. The mandibular second molar is most often two-rooted with three to four canals [14]. Using the Vertucci classification, the type IV configuration is seen most often in mesial roots, followed by type II configuration [15]. Vertucci type I is the most frequent canal configuration of the distal root [16]. The locations of the canal orifices of the typical mandibular first molar dictate a trapezoidal access preparation [17].
It is noteworthy that out of the reports in the literature detailing the variants of molar root canal anatomy, the vast majority of which were published after 2011 and were based on CBCT data. The complexity of mandibular molars and the location of vital structures make CBCT imaging essential for safe, successful treatment. The AAE/Oral Maxillofacial Radiologists’ recommendations advise taking CBCTs in this circumstance [18]. An additional CBCT finding, underlining the utility of CBCT data for assessing craniofacial anatomy, was the bifurcation of the inferior alveolar canal with accessory canals near the apex of the distal root (Figure 2C). The clinical management approach to root canal treatment may be altered based on the complexity of the canal system [19]. The lingual root of radix entomolaris is most frequently Vertucci type I [20]. The extra distolingual orifice is located an average of 2.93mm lingual to the distobuccal orifice and is often hidden by a dentinal shelf [21].
It appears that no comparable metric information is available regarding RP because of its rarity. The usual trapezoidal access preparation needs to be extended in both RE and RP to locate and clean and shape the additional root. In the case presented here, the initial root canal treatment left the buccal canal of the radix paramolaris untreated. The value of small field CBCT imaging is clearly shown in (Figures 1 & 3). The preoperative periapical film of tooth #18 did not disclose the presence of an extra buccal root (Figure 2A), because the third dimension, or mesiodistal plane, is unseen on periapical radiographs [22]. The CBCT showed the buccal root curved in a buccal-lingual direction and enabled the endodontist to fully appreciate the root canal system of tooth #18 in three dimensions and provided a more detailed understanding of the root canal anatomy [23].
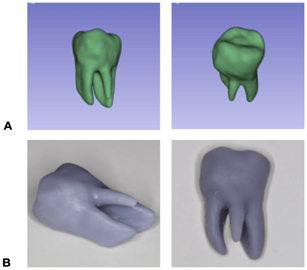
Another more recent use of CBCT data, beyond visualization of 2D and 3D renderings, is the ability to generate 3D models from DICOM files. CBCT data was then converted to a stereolithography (.stl) file (3D Slicer 4.10.02, National Alliance for Medical Image Computing, Boston, MA). This model clearly depicts the unique anatomy of this tooth (Figure 4A). The 3D printed models (Figure 4B) demonstrate the true angulation and dimensions of the RP in this case. Another benefit of the 3D printed model is the appreciation of the narrow diameter and comparatively short length of the RP root. Accurate diagnosis and treatment depend on the practitioner’s ability to treat the entire root canal system [24-27]. Endodontists should be mindful that additional roots may vary greatly in dimensions stressing the importance of recording accurate working lengths and selecting appropriate instrumentation taper. The ability to obtain 3D data and rapidly create models can help clinicians to manage such rare conditions with more confidence.
Figure 4: Post-processing of CBCT data for further analysis. A) Angulated three-dimensional (.stl) (stereolithography) images of radix paramolaris. B) 3D printed models from (.stl) files demonstrating buccal curvature of radix paramolaris.
Conclusion
Clinicians need to understand the possible variations of root canal morphology of mandibular molars in order to successfully treat these teeth. CBCT imaging can be used in addition to periapical radiographs to better understand the root canal anatomy and treat a tooth with radix paramolaris.
Article Info
Article Type
Case ReportPublication history
Received: Mon 03, May 2021Accepted: Mon 17, May 2021
Published: Tue 01, Jun 2021
Copyright
© 2023 Ove Peters. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ORD.2021.01.01
Author Info
Samer Ebeid Raymond Scott Shreyas Oza Julian Shen Gordon Lai Ove Peters
Corresponding Author
Ove PetersDepartment of Endodontics, University of the Pacific, Arthur A. Dugoni School of Dentistry, San Francisco, California, USA
Figures & Tables

References
1.
Ballullaya SV, Vemuri S, Kumar PR (2013) Variable
permanent mandibular first molar: Review of literature. J Conserv Dent 16:
99-110. [Crossref]
2.
Kerekes K, Tronstad L (1977) Morphometric observations on
the root canals of human molars. J Endod 3: 114-118. [Crossref]
3.
Sperber GH, Moreau JL (1998) Study of the number of roots
and canals in Senegalese first permanent mandibular molars. Int Endod J
31: 117-122. [Crossref]
4.
Carabelli G, Carabelli G, von Lunkaszprie GC, Carabelli
Edl G (1985) Systematisches Handbuch der Zahnheilkunde. Georg Olms Verlag.
5.
Calberson FL, De Moor RJ, Deroose CA (2007) The radix
entomolaris and paramolaris: clinical approach in endodontics. J Endod
33: 58-63. [Crossref]
6.
Carlsen O, Alexandersen V (1991) Radix paramolaris in
permanent mandibular molars: identification and morphology. Scand J Dent Res 99: 189-195. [Crossref]
7.
Visser JB (1948) Beitrag zur Kenntnis der menschlichen
Zahnwurzelformen. Buchdruckerei Rotting.
8.
Felsypremila G, Vinothkumar TS, Kandaswamy D (2015)
Anatomic symmetry of root and root canal morphology of posterior teeth in
Indian subpopulation using cone beam computed tomography: A retrospective
study. Eur J Dent 9: 500-507. [Crossref]
9.
Kuzekanani M, Najafipour R (2018) Prevalence and
Distribution of Radix Paramolaris in the Mandibular First and Second Molars of
an Iranian Population. J Int Soc Prev Community Dent 8: 240-244. [Crossref]
10.
Arun J, Mayuri BS, Nandini TN, Goud KM (2015) Radix
entomolaris and paramolaris: A case series. Int J Oral Health Sci 5:
57-62.
11.
Mitra M, Rao MA, Grewal MS, Singla M, Arya A (2020) Radix
Entomolaris and Paramolaris: A Case Series. Ind J Health Sci Care 7:
35-39.
12.
Ng YL, Mann V, Gulabivala K (2011) A prospective study of
the factors affecting outcomes of nonsurgical root canal treatment: part 1:
periapical health. Int Endod J 44: 583-609. [Crossref]
13.
Siqueira Jr JF, Rôças IN (2008) Clinical implications and
microbiology of bacterial persistence after treatment procedures. J Endod
34: 1291-1301. [Crossref]
14.
Skidmore AE, Bjorndal AM (1971) Root canal morphology of
the human mandibular first molar. Oral Surg Oral Med Oral Pathol 32:
778-784. [Crossref]
15.
Vertucci FJ (2005) Root canal morphology and its relationship
to endodontic procedures. Endod Topics 10: 3-29.
16.
de Pablo OV, Estevez R, Sánchez MP, Heilborn C, Cohenca N
(2010) Root anatomy and canal configuration of the permanent mandibular first
molar: a systematic review. J Endod 36: 1919-1931. [Crossref]
17.
Wilcox LR, Walton RE, Case WB (1989) Molar access: shape
and outline according to orifice locations. J Endod 15: 315-318. [Crossref]
18.
Fayad MI, Nair M, Levin MD, Benavides E, Rubinstein RA et
al. (2015) AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed
Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral
Radiol 120: 508-512. [Crossref]
19.
Gulabivala K, Patel B, Evans G, Ng YL (2005) Effects of
mechanical and chemical procedures on root canal surfaces. Endod Topics
10: 103-122.
20.
Gu Y, Lu Q, Wang H, Ding Y, Wang P et al. (2010) Root
canal morphology of permanent three-rooted mandibular first molars--part I:
pulp floor and root canal system. J Endod 36: 990-994. [Crossref]
21.
Zhang R, Wang H, Tian YY, Yu X, Hu T et al. (2011) Use of
cone-beam computed tomography to evaluate root and canal morphology of
mandibular molars in Chinese individuals. Int Endod J 44: 990-999. [Crossref]
22.
Patel S (2009) New dimensions in endodontic imaging: Part
2. Cone beam computed tomography. Int Endod J 42: 463-475. [Crossref]
23.
Abella F, Mercadé M, Duran Sindreu F, Roig M (2011)
Managing severe curvature of radix entomolaris: three-dimensional analysis with
cone beam computed tomography. Int Endod J 44: 876-885. [Crossref]
24.
Baruwa AO, Martins JNR, Meirinhos J, Pereira B, Gouveia J
et al. (2020) The Influence of Missed Canals on the Prevalence of Periapical
Lesions in Endodontically Treated Teeth: A Cross-sectional Study. J Endod
46: 34-39. [Crossref]
25.
Tabassum S, Khan FR (2016) Failure of endodontic
treatment: The usual suspects. Eur J Dent 10: 144-147. [Crossref]
26.
Iqbal A (2016) The Factors Responsible for Endodontic
Treatment Failure in the Permanent Dentitions of the Patients Reported to the
College of Dentistry, the University of Aljouf, Kingdom of Saudi Arabia. J
Clin Diagn Res 10: ZC146 -ZC148. [Crossref]
27. Sjogren U, Hagglund
B, Sundqvist G, Wing K (1990) Factors affecting the long-term results of
endodontic treatment. J Endod 16: 498-504. [Crossref]
