Journals
Endoprosthetic Total Scapula Replacement Versus Suspension Arthroplasty Following Tumor Resection
A B S T R A C T
The purpose of this study is to define the minimum requirements for total scapular replacement with metallic endoprosthesis and compare it to suspension arthroplasty. A retrospective analysis was performed of three musculoskeletal tumor registries for patients with scapulectomy for musculoskeletal tumors. Patients were divided into two groups: Group I included eleven patients who had endoprosthetic scapula replacement (Endotec, Bloomfield, NJ, Howmedica, Rutherford, NJ). Group II included nine patients with suspension arthroplasty. Overall MSTS scores were higher in group I than in Group II (23.5+2.5 versus 17+2.6; p=0.0001). Scores in Group I was significantly higher in all categories but dexterity. The lowest score in both groups was in the function category (3.6+0.8 versus 1.7+1.0; p < 0.001). The data shows that patients with endoprosthetic replacements have higher MSTS scores in emotional acceptance and function, compared to those with suspension arthroplasty. The greater motion found in group I (endo) was most evident in forward flexion, abduction and external rotation. This was thought to be a results of lateral positioning, scapulothoracic reconstruction and pseudoarthrosis.
Keywords
Scapula, Endoprosthetic, Musculoskeletal Oncology, Suspension Arthroplasty.
I N T R O D U C T I O N
Historically, complete resection of the scapula without reconstruction has been associated with significant loss in function and injuries to the neurovascular bundle [1-6]. In patients requiring total resection of the glenoid and rotator cuff, reconstructive methods, as well as MSTS (Musculoskeletal Tumor Society) functional scores, have been limited. Several methods of reconstruction have been proposed, including suspension arthroplasty [1, 4, 6-8], allograft replacement, and endoprosthetic reconstruction [2, 9-12]. The results have varied, and only two studies comparing endoprosthetic reconstruction to suspension arthroplasty have been reported [11].
The purpose of this study is to define the minimum requirements for total scapular replacement with metallic endoprosthesis and compare it to suspension arthroplasty. The hypothesis is that when total scapular excision must be performed, and the axillary nerve and deltoid muscle neuromuscular unit are able to be preserved, endoprosthetic scapula replacement is superior to suspension arthroplasty in overall active motion and MSTS upper extremity functional scores.
Materials & Methods
From 1986 through 2016, a retrospective analysis was performed of three musculoskeletal tumor registries for patients with scapulectomy for musculoskeletal tumors following IRB approval. Patients were included in our analysis if they met the following criteria: (1) Total scapulectomy for musculoskeletal tumor of the S1, S2 or S1 S 2 S 3 types according to the staging system of the MSTS (Figure 1), (2) Patients had to have had a limb-salvage surgery with preservation of the neurovascular bundle (brachial plexus and subclavian – axillary vessels). (3) Preservation of the deltoid-axillary nerve complex and (4) reconstruction with a total scapular endoprosthesis or resection arthroplasty suspension from clavicle of humeral head. Twenty-two patients had a total scapulectomy and twenty met the above criteria. One patient was excluded because the axillary nerve was resected, and one patient had an allograft scapula replacement.
Seventeen patients had an MSTS S12A (Malawar IIIA) resection and three patients had an S123A (Malawar/IVA) procedure (Figure 1). Patients were divided into two groups: Group I included eleven patients who had endoprosthetic scapula replacement (Endotec, Bloomfield, NJ, Howmedica, Rutherford, NJ). Group II included nine patients with suspension arthroplasty.
Figure 1: S12A (Malawar IIIA) and S123A (Malawar IVA).
Surgical Technique
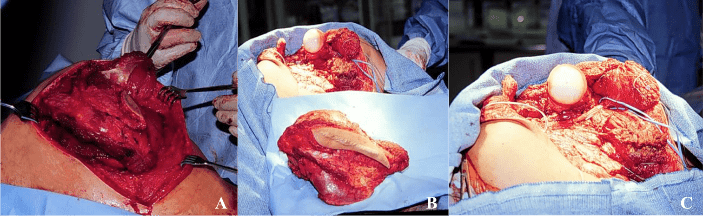
Patients had a posterior approach to their scapular tumors with removal of the biopsy tract, rotator cuff musculature and bony scapula en bloc, with the deltoid muscle and axillary nerve preserved in all cases (Figure 2). The chest wall was uninvolved in these cases and a cuff of muscle including trapezius, rhomboids, levator scapulae, and scalenus anterior were preserved. The latissimus dorsi muscles were preserved in all cases.
Figure 2: 2a (posterior approach), 2b (scapula, biopsy tract, and rotator cuff muscles), 2c (axillary nerve preservation).
Suspension Arthroplasty
Patients who underwent suspension arthroplasty had the humeral head suspended from the clavicle with gortex and mersilene tapes medializing the humeral head (Figure 3). The deltoid was anchored to the chest wall posteriorly.
Figure 3: Suspension arthroplasty.
Endoprosthetic Total Scapula Replacement
Patients who underwent endoprosthetic scapula replacement had a custom scapula (Endotec, Bloomfield, NJ, Howmedica, Rutherford, NJ) placed in the resection bed. The humerus was resurfaced in six patients (Endotec, Bloomfield, NJ,) and hemiarthroplasty was performed in five (Howmedica, Rutherford, NJ). Following humeral implantation, a pseudocapsule was created using Dacron and gortex material (Figure 4). Soft-tissue reconstructions were performed using the levator scapulae, rhomboids, serratus anterior, and distal teres major as deep envelope and trapezius, deltoid and latissimus pedicle flap as the superficial soft-tissue coverage of the metallic implant (Figure 4).
Figure 4: 4a (Pseudocapsule reconstruction), 4b (attachment of deep muscular envelope).
All patients had suction drains placed and those with endoprosthesis were placed in an airplane abduction brace for six weeks. Patients had progressive mobilization with muscle strengthening therapy for an additional six to twelve weeks. Patients were evaluated using the system of the Musculoskeletal Tumor Society when rehabilitation was complete. In additions to the functional scoring system, range of motion was recorded in all planes of motion, including forward flexion, abduction, extension, internal, and external rotation both actively and passively. Radiographs were taken at the initial postoperative visit and following brace removal and completion of physical therapy. In addition, patients had plain radiographs taken every six months. In patients with osteosaroma, Ewing’s sarcoma and MFH, postoperative chemotherapy was resumed four weeks following surgery. No patients received radiation therapy postoperatively. Patients had postoperative metastatic surveillance at regular intervals both for sarcoma and secondary lesions.
Results
Patients were evaluated for disease status at the last follow up. Nine patients have been continuously disease free, five have no evidence of disease, two are alive with disease, four patients died of disease. Patients in Group I had a mean follow-up of 85 months (range, 24-163 months). Patients in Group II had a mean follow-up of 59 months (range, 5-154 months). Functional results, including range of motion in all planes, are shown in (Figure 2). The patients were graded according to the functional evaluation system of the MSTS. Overall MSTS scores were higher in group I than in Group II (23.5+2.5 versus 17+2.6; p=0.0001). Scores in Group I was significantly higher in all categories but dexterity. The lowest score in both groups was in the function category (3.6+0.8 versus 1.7+1.0; p < 0.001).
|
Table 1. Post-operative active-shoulder range of motion |
|||
|
|
Group I |
Group II |
P value |
|
Forward Flexion |
74 |
18 |
<0.0001 |
|
Abduction |
70 |
28 |
<0.0001 |
|
Extension |
33 |
13 |
0.0014 |
|
Internal Rotation |
50 |
59 |
0.44 |
|
External Rotation |
34 |
4 |
0.001 |
|
Total |
268 |
113 |
<0.0001 |
Group I: Endoprosthesis, Group II: Suspension Arthroplasty
The results of active shoulder motion were significantly higher in Group I in all planes and motion. These results were particularly increased in scores of forward flexion, with an average of 74 degrees compared to an average of 18 degrees in patients with a suspension procedure (P < 0.0001). The total motion for patients in Group I averaged 260 degrees compared to 113 degrees of patient in group II (P < 0.0001).
Complications that have occurred included a teenage patient with chondrosarcoma of the scapula who had a functional reconstruction yet requested an amputation for recurrent disease. O and radiation were utilized in group 1 (endo) patients without any appreciable difference in ROM or MST scores. Two group II patients had postoperative radiation of (palliative dose) without any appreciable effects. The range of motion in these two patients did not differ from those in group II who did not receive radiotherapy.
Discussion
Partial scapulectomy was described in 1820 by Liston and later James Syme reported total scapulectomy for chondrosarcoma in 1864 [13, 14]. Around the turn of the century, two surgeons, Tikkor and later Lindberg described an internal amputation of the shoulder preserving the arm, forearm and hand that bears their name [15]. At the same time, De Nancrede reported on a series of scapulectomies and concluded that it was inadequate in preventing local recurrence for tumors when compared to forequarter amputation [16].
After the advent of chemotherapy, George Pack at memorial hospital in New York City (1955) re-established the Tikkor–Linberg resection as a technique for preservation of hand function. He maintained that adequate margins must be obtained to prevent recurrence. In an isolated report, Papaionnow[6] described the functional results of non-implant partial and total scapulectomies in 1965. In 1987, Eckhart reported on eight patients with S12 resections and endoprosthetic reconstruction [17]. Average forward flexion and abduction was 30° and 25° respectively. The average MSTS score was 76%. There were no specific guidelines or reports of structures removed in each case or any detail of the indications.
To the author’s knowledge, this is only the third report comparing endoprosthetic replacement and suspension arthroplasty. In 2007, Pritsch et al reported improved functional results in patients with scapular replacement compared to suspension arthroplasty (23.5 versus 17.5) [11]. In that same study, nearly half of patients with scapular replacement had greater than 40 degrees of abduction and forward flexion. In 2017, Hayashi et al mirrored those results in a multicenter study preformed at Eastern Asian Musculoskeletal Oncology Group [18]. Based on Ennekin functional scores, prothesis resulted in improved functional outcomes compared to suspension (23.6 versus 21.4). Additionally, prosthetic ROM allowed for an average flexion of 57° and abduction of 40°, compared to suspensions 30° and 22.3° respectively. Our results showed similar benefit to endoprosthetic replacement as the prior studies, with mean MSTS scores of 23.5 compared to 17. Additionally, all patients with scapular replacement had greater than 40 degrees of abduction and forward flexion, while no patients with suspension arthroplasty did. In our study, cosmesis was not specifically scored, but patients with scapular replacement lacked the degree of concavity and neckline abnormalities present in patients with suspension arthroplasty. Though our study is similar in nature, our results support findings in the prior reports comparing these two treatments groups and add to the current literature. It is however, the only paper to report ROM including forward flexion as well as the importance of preservation of the deltoid-axillary nerve complex.
Potential shortcomings of this study include its retrospective nature and three multi-institutional databases. However, the authors used the same surgical technique for endoprosthetic and suspension procedures. Also, while minimum follow-up was 2 years, the burden of metastatic disease resulted in the loss of 2 patients prior to 2 years follow-up, and loss of 5 patients prior to 3 years follow-up. Although these patients were lost to disease progression, they had completed physical therapy and functional scores were able to be obtained.
Figure 5: 5a (Resection-arthroplasty suspension, medial displacement shown), Figure 5b (Total scapula replacement, lateral position maintained).
In this report, the hypothesis entertained was that medial displacement of the humeral head with decreased soft-tissue tension and working length of muscle in resection arthroplasty suspension patients would result in inferior outcomes compared to patients with total scapular replacement, where there would be a maintenance of the lateral position of the humeral head with adequate soft-tissue tension and working length of muscle (Figure 5). The data shows that patients with endoprosthetic replacements have higher MSTS scores in emotional acceptance and function, compared to those with suspension arthroplasty. The acceptance criteria were thought to be higher due to the cosmetic improvement and body contour associated with endoprosthetic replacements the function category was thought to be higher overall due to the greater motion of those in group I (endo) compared to suspension arthroplasty (group II). The greater motion found in group I (endo) was most evident in forward flexion, abduction, and external rotation was thought to be a result of lateral positioning and scapulothoracic reconstruction and pseudoarthrosis.
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 19, Oct 2018Accepted: Sat 03, Nov 2018
Published: Fri 28, Dec 2018
Copyright
© 2023 Joseph Benevenia. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2018.01.002
Author Info
Albert Aboulafia David K. Monson Jennifer Thomson Joseph A. Ippolito Joseph Benevenia Mark C. Leeson
Corresponding Author
Joseph BeneveniaRutgers New Jersey Medical School Department of Orthopaedics, NJ
Figures & Tables




|
Table 1. Post-operative active-shoulder range of motion |
|||
|
|
Group I |
Group II |
P value |
|
Forward Flexion |
74 |
18 |
<0.0001 |
|
Abduction |
70 |
28 |
<0.0001 |
|
Extension |
33 |
13 |
0.0014 |
|
Internal Rotation |
50 |
59 |
0.44 |
|
External Rotation |
34 |
4 |
0.001 |
|
Total |
268 |
113 |
<0.0001 |
Group I: Endoprosthesis, Group II: Suspension Arthroplasty
References
1. Badhwar, R (1990) Reconstruction following limb-sparing en bloc resection of the shoulder girdle--Tikhoff-Linberg procedure. Indian J Cancer 27: 31-37. [Crossref]
2. Bickels J, Wittig JC, Kollender Y, Kellar-Graney K, Meller I, et al. (2002) Limb-sparing resections of the shoulder girdle. J Am Coll Surg 2002 194: 422-435. [Crossref]
3. FRANCIS KC, WORCESTER JN Jr (1962) Radical resection for tumors of the shoulder with preservation of a functional extremity. J Bone Joint Surg Am 1962. 44: 1423-1430. [Crossref]
4. Marcove RC, Lewis MM, Huvos AG (1977) En bloc upper humeral interscapulo-thoracic resection. The Tikhoff-Linberg procedure. Clin Orthop Relat Res 124: 219-228. [Crossref]
5. O'Connor MI1, Sim FH, Chao EY (1996) Limb salvage for neoplasms of the shoulder girdle. Intermediate reconstructive and functional results. J Bone Joint Surg Am 78: 1872-1888. [Crossref]
6. Papaioannou AN, Francis KC (1965) Scapulectomy for the treatment of primary malignant tumors of the scapula. Clin Orthop Relat Res 41: 125-132. [Crossref]
7. Ham SJ, Hoekstra HJ, Eisma WH, Schraffordt Koops H, Oldhoff J (1993) The Tikhoff-Linberg procedure in the treatment of sarcomas of the shoulder girdle. J Surg Oncol 53: 71-77. [Crossref]
8. Kumar VP, Satku SK, Mitra AK, Pho RW (1994) Function following limb salvage for primary tumors of the shoulder girdle. 10 patients followed 4 (1-11) years. Acta Orthop Scand 65: 55-61. [Crossref]
9. Mnaymneh WA, Temple HT, Malinin TI (2002) Allograft reconstruction after resection of malignant tumors of the scapula. Clin Orthop Relat Res 405: 223-229. [Crossref]
10. Asavamongkolkul A, Eckardt JJ, Eilber FR, Dorey FJ, Ward WG, et al. (1999) Endoprosthetic reconstruction for malignant upper extremity tumors. Clin Orthop Relat Res 360: 207-20. [Crossref]
11. Pritsch T, Bickels J, Wu CC, Squires MH, Malawer MM (2007) Is scapular endoprosthesis functionally superior to humeral suspension? Clin Orthop Relat Res 456: 188-95. [Crossref]
12. Wittig JC, Bickels J, Wodajo F, Kellar-Graney KL, Malawer MM (2002) Constrained total scapula reconstruction after resection of a high-grade sarcoma. Clin Orthop Relat Res 397: 143-55. [Crossref]
13. Liston, R (1820) Ossified aneurysmal tumor of the subscapular artery. Ediul Med J 16: 66-70.
14. Syme J (1864) Excision of the Scapula. Edinburgh: Edmonston & Douglas.
15. Lindberg BE (1928) Interscapulo-thoracic resection formalignant tumors of the shoulder girdle region. J Bone Joint Surg10: 344-349.
16. Charles B. G. De Nancrede (1909) The end results after total excision of the scapula for sarcoma. Ann Surg 50: 1. [Crossref]
17. Eckardt JJ (1987) Orthopedics: endoprosthetic limb salvage operation for malignant bone tumors. West J Med 146: 470. [Crossref]
18. Hayashi K, et al. (2017) Experience of total scapular excision for musculoskeletal tumor and reconstruction in eastern Asian countries. J Bone Oncol 9: 55-58.
