Endoscopic Removal of A Nasogastric Tube Accidentally Stitched During Bariatric Surgery: A Case Report and Review of the Literature
A B S T R A C T
To mistakenly suture a nasogastric tube (NGT) at an anastomotic site is a rare surgical occurrence during gastrointestinal operations. Therapeutic options are substantially represented by endoscopic management or surgery.
Here we report our experience in the successful endoscopic removal of a NGT, sutured at the level of the gastrojejunal anastomosis after the performance of a mini-gastric bypass.
Keywords
Nasogastric tube, endoscopic removal, bariatric surgery
Introduction
To mistakenly suture a nasogastric tube (NGT) at an anastomotic site is a rare surgical occurrence during gastrointestinal operations. Therapeutic options are substantially represented by endoscopic management or surgery. No guidelines about how to manage this situation is to date available. Here we report our experience in the successful endoscopic removal of a NGT, sutured at the level of the gastrojejunal anastomosis after the performance of a mini-gastric bypass.
Case Report
A 41-year-old obese woman (BMI 39.7), without any other known disease, underwent a laparoscopic mini-gastric bypass. On the first postoperative day, an attempt to remove the 16-Fr NGT was made, without success. On the suspicion of a sutured extremity of the NGT, an endoscopic consultation was requested. A preliminary attempt to cut a similar NGT with a polyp snare was made before the procedure, but due to the diameter and the stiffness of the tube, it wasn’t successful.
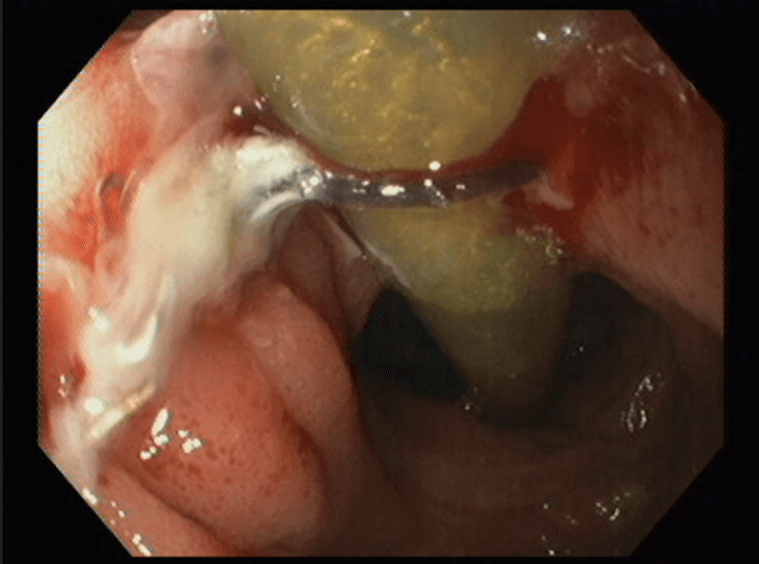
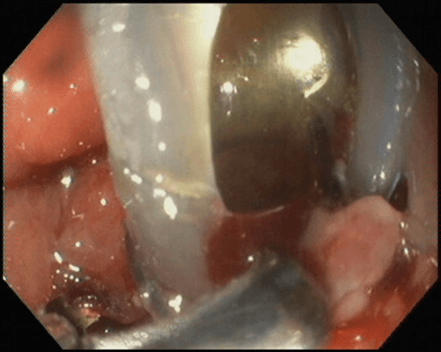
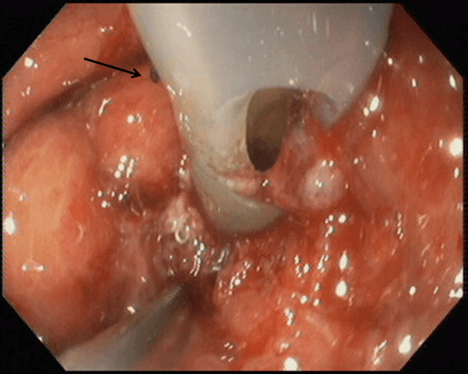
On the fifth day after surgery an upper endoscopy was performed, confirming that just below the oesophago-gastric junction, an absorbable suture of V-Lock 3/0 wire was tightly anchored to the distal extremity of the NGT (Figure 1). Due to the very narrow working space, the cautious use of air, and the hard and slick surface of the tube, it was impossible to grasp or cut the stitch with the use of rat tooth forceps and endoscopic scissors. An attempt with a coagrasper was also made, but without success. To expose the distal, lateral hole of the tube at the wire level, the proximal end of the NGT was slightly tractioned through the mouth of the patient (Figure 2). Taking advantage of the space through the hole, the stitch was cut with endoscopic scissors (Olympus Medical, Tokyo, Japan) and the NGT was removed (Figure 3). No immediate nor late complications occurred during the hospitalization, so the patient was discharged two days after the procedure. At the one-week outpatient follow-up, the patient was in good condition and on a free diet.
Figure 1: An absorbable suture wire anchored to the distal extremity of the NGT.
Figure 2: The distal, lateral hole of the NGT at the wire level exposed by a slight traction through the mouth of the patient.
Figure 3: The stitch (arrow) cut with endoscopic scissors.
Discussion
The advancement of surgical techniques requires great attention to many operative details; moreover, the widespread use of staplers and robotic systems in gastrointestinal surgery can be burdened by a variety of technical complications, some related to the absence of direct handling of the anastomosis. That is the case for the fastened NGT, which rarely occurs with manual sutures during an operation [1]. Ensuring that the tube is positioned well above the anastomotic site and testing its mobility before the suture are useful suggestions to prevent such an occurrence [2].
We made a review of the literature to find all published reports of endoscopic removal of a NGT mistakenly sutured during surgery. Thirteen case reports have been described in several interventions, such as the Nissen fundoplication, Dor fundoplication, partial gastric resection total gastrectomy, oesophageal resection, oesophago-colon-gastroplasty, robotically assisted laparoscopic biliopancreatic diversion with duodenal switch, open abdominal surgery for primary repair of a gastro-duodenal perforation, laparorobotic pancreaticoduodenectomy [1-13]. Six of them were performed manually [1, 3, 4, 10, 11, 14]. Concerning the endoscopic device, the most used were mechanical modalities (rat-tooth forceps, snares, endoscopic scissors) and monopolar or bipolar electrocautery. Even Argon Plasma Coagulation (APC) was used to attempt to degrade or dislodge the tube [12]. Galasso and colleagues realized a homemade endoscopic guillotine, made by combining the metal sheath from a mechanical lithotriptor and a polypectomy snare to severe the tube [9]. Studies are summarized in (Table 1).
Table 1: Summary of the case reports.
|
Study
-year |
Intervention |
Timing |
Endoscopi
device |
|
Urschel et
al. 1990 [2]s |
Partial gastrectomy (Billroth II) |
20 days |
Endoscopic snare |
|
Reissman
et al. 1994 [3] |
Nissen
fundoplication and gastrostomy |
n.a. |
Laparoscopic scissors under endoscopic view |
|
Chen et
al. 1997 [1] |
Gastrojejunostomy |
2 weeks |
Biopsy forceps |
|
Han
et al. 1999 [6] |
Antrectomy with Billorth II and Roux-En-Y
jejunostomy |
12 days |
Endoscopic suture cutter (Olympus FS-3L) |
|
Mahmood et
al. 2007 [8] |
Distal esophagectomy |
7 days |
n.a. |
|
Shaaban
et al. 2009 [4] |
Dor
fundoplication |
1
day |
Diathermic
snare |
|
Wilkinson et al. 2011 [12] |
Pancreaticoduodenectomy |
2 days |
Endoscopic
scissors (after failing with rat-tooth forceps, loop wire cutters, snares,
endoscopic scissors, monopolar/bipolar electrocautery) |
|
Sucandy
et al. 2011 [10] |
Robotically assisted laparoscopic biliopancreatic
diversion with duodenal switch |
1 day |
Endoscopic cutter through sideview
ERCP scope |
|
Galasso et
al. 2013 [9] |
Surgery on a
proximal colon–gastric anastomosis |
3 weeks |
Homemade
endoscopic guillotine: combination of the metal sheath of a mechanical
lithotriptor and a polypectomy snare |
|
Knežević
et al. 2013 [5] |
Gastric resection, with Billroth II |
7 days |
Precut papilliotome needle and alligator jaw
foreign body forceps |
|
Kim et
al. 2016 [11] |
Repair of a
duodenal perforation |
6 days |
Endoscopic loop cutter |
|
Morais
et al. 2017 [14] |
Gastric
ulcer suture |
7
days |
Hot
biopsy forceps |
|
Azzam et
al. 2018 [7] |
Total gastrectomy with a Roux-en-Y
oesophagojejunostomy |
6 weeks |
Endoscopic snare |
In no one of such reports, complications were described after the procedure. As with most of surgical complications, reoperation is not considered the best choice both for the surgeon and for the patient; laparoscopic management of post-surgical complications can be technically challenging with a high rate of morbidity as well as conversion to laparotomy, moreover, prolonged hospitalizations and further, serious complications should be taken into account [14].
Endoscopy has the advantage of being minimally invasive, it prevents potential general anaesthetic complications, it doesn’t need a sterile environment, it is able to exactly determine the site of the foreign body entrapment and, if feasible, it permits the preservation of the created suture. Performing endoscopy in the immediate postoperative period, however, is controversial as it entails the risk of anastomotic dehiscence due to the insufflation of air during the exam.
Some authors suggested performing endoscopy only after the healing time for gastrointestinal anastomosis, estimated to be of 2-3 weeks, but we also found a report of endoscopic removal of NGT performed after 6 weeks, after a temporary measure [1, 2, 6, 7, 9]. More recently, earlier endoscopic attempts have been described, from 6-7 days after surgery, up to 1-2 days postoperative [4, 5, 10-13].
A combined laparoscopic and endoscopic management was also proposed by Reissman and colleagues [3]. Although there is no consensus on the optimal timing, the safety of early endoscopic intervention after surgery seems to be established. It emerges also by the therapeutic algorithm proposed by García- García for post-operative early gastrointestinal bleeding occurring between the first and the sixth day after bariatric surgery. The authors conclude by recommending endoscopic examination with minimal air insufflation and caution in cases of bleeding [15].
We can conclude that endoscopy represents a safe and possible solution to manage NGTs accidentally sutured, even when the procedure is performed early after surgery, cautiously, with minimal air insufflation or, with the use of CO2 if possible. A laparoscopic approach with possible repair/re-creation of the anastomosis should be reserved as the next option only when the endoscopic approach fails.
Article Guarantor
Giada Di Donato.
Author Contributions
Giada Di Donato: design and drafting of the work, acquisition of data; Annalisa Capannolo: drafting and revising of the work; Marco Valvano: design and drafting of the work; Giovanni Cianca: critical revision of the work, final approval; Loreto Lombardi: critical revision of the work, final approval.
Conflicts of Interest
None.
Funding
None.
Informed Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Thu 15, Jun 2023Accepted: Mon 10, Jul 2023
Published: Mon 24, Jul 2023
Copyright
© 2023 Annalisa Capannolo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2023.05.01
Author Info
Giada Di Donato Annalisa Capannolo Marco Valvano Giovanni Cianca Loreto Lombardi
Corresponding Author
Annalisa CapannoloDiagnostic and Surgical Endoscopy Unit, S. Salvatore Hospital, Via L. Natali, L'Aquila, Italy
Figures & Tables
References
1. Chen CN, Lee WJ, Cheng TJ,
Chang KJ (1997) Endoscopic removal of nasogastric tube sutured unintentionally
to gastrojejunostomy. Surg Laparosc Endosc 7: 359-360. [Crossref]
2. Urschel JD, Stockburger HJ
(1990) Endoscopic extraction of an entrapped nasogastric tube. Am Surg
56: 730-732. [Crossref]
3. Reissman P, Udassin R,
Goldin E, Durst AL (1994) Management of an inadvertently sutured nasogastric
tube after Nissen fundoplication. Gastrointest Endosc 40: 260-261. [Crossref]
4. Shaaban H, Armstrong C
(2009) Nasogastric tube accidentally stitched to the stomach during
laparoscopic antireflux surgery. Endoscopy 41 Suppl 2: E61. [Crossref]
5. Knežević A, Knežević V, Jovanović I, Gvozdenović
L et al. (2013) Successful
endoscopic management of an entrapped nasogastric tube after a surgical
procedure. Surg Laparosc Endosc Percutan Tech 23: 233. [Crossref]
6. Han HF, Perng CL, Hung HC,
Lin HJ, Chang FY et al. (1999) Iatrogenic entrapped nasogastric tube with
endoscopic removal. J Clin Gastroenterol 29: 103-104. [Crossref]
7. Azzam AZ, Azzam KA, Amin T
(2018) Removal of Nasogastric Tube Accidentally Stitched to Roux-en-Y
Oesophagojejunostomy Following a Radical Gastrectomy for Stomach Cancer: Case
report and review of the literature. Sultan Qaboos Univ Med J 18:
e110-e111. [Crossref]
8. Mahmood A, Joseph E,
Robinson RB, Akhras J, McKany M et al. (2007) The role of endoscopy in
nasogastric tube removal following esophageal surgery: a case report. Int J
Surg 5: 342-344. [Crossref]
9. Galasso D, Tringali A, Riccioni ME, Costamagna G
(2013) Use of a homemade endoscopic
guillotine to cut through a nasogastric tube inadvertently sutured to a
colon-gastric anastomosis. Endoscopy 45 Suppl 2 UCTN: E413-E414. [Crossref]
10. Sucandy I, Antanavicius G
(2011) A novel use of endoscopic cutter: Endoscopic retrieval of a retained
nasogastric tube following a robotically assisted laparoscopic biliopancreatic
diversion with duodenal switch. N Am J Med Sci 3: 486-488. [Crossref]
11. Kim SY, Chung JW, Yang JY
(2016) Endoscopic removal of a nasogastric tube accidentally ligated to the
duodenum after open abdominal surgery. Endoscopy 48 Suppl 1 UCTN: E18. [Crossref]
12. Wilkinson MN, Jayaraman V,
Watkins K, Bao P, Buscaglia (2011) Newly developed flexible endoscopic scissors
for removal of a nasogastric tube trapped within a gastrojejunal anastomotic
staple line. Endoscopy 43 Suppl 2 UCTN: E234-E235. [Crossref]
13. Heneghan HM, Meron-Eldar S, Yenumula P, Rogula T,
Brethauer SA et al. (2012) Incidence and management of bleeding complications
after gastric bypass surgery in the morbidly obese. Surg Obes Relat Dis
8: 729-735. [Crossref]
14. Morais R, Marques M, Rodrigues S, Macedo G (2017) An immobile postsurgical nasojejunal tube: a case for King Arthur! Rev Esp Enferm Dig 109: 222. [Crossref]
15. García García ML, Martín Lorenzo JG, Torralba Martínez JA, Lirón-Ruiz R, Perelló JM et al. (2015) Emergency endoscopy for gastrointestinal bleeding after bariatric surgery. Therapeutic algorithm. Cir Esp 93: 97-104. [Crossref]
