Entrapment of the Basilar Artery into the Sphenoid Sinus, With CSF Fistula, without Ischaemic Stroke: A Case Report
A B S T R A C T
The basilar artery herniation into the sphenoid sinus secondary to skull base fracture is a rare condition. There have been few cases described worldwide. This entity carries a potential risk of basilar artery stenosis or occlusion, resulting in ischaemia and infarction of the brainstem and cerebellum. Images study such as computed tomography (CT) and MRI plays a crucial role in diagnosing this condition. We report a rare case that shows entrapment of the basilar artery into the sphenoid sinus, after a traumatic skull base fracture, without infarction of the brainstem and cerebellum, with CSF fistula.
Keywords
Basilar artery herniation, basilar artery entrapment, skull base fracture, clivus, CSF fistula
Introduction
Fractures of the clivus are uncommon and usually result from high-impact cranial injury [1]. A rare consequence of this event is herniation of the basilar artery into the sphenoid sinus, which carries a potential risk of basilar artery stenosis or occlusion, resulting in ischaemia and infarction of the brainstem and cerebellum. The imaging studies: computed tomography (CT) and MRI play a crucial role in diagnosing this condition.
This report aims to present a rare case of traumatic skull base fracture with entrapment of the basilar artery into the sphenoid sinus, with CSF fistula, without infarction of the brainstem and cerebellum evidenced by CT-cisternography and MRI.
Case Report
A 40-year-old woman was referred to our department with a history of CSF rhinorrhea and severe postural headache. She related a history of severe head trauma with frontal bone fracture and hemorrhagic contusion in the frontal lobes, according to a brain CT performed at another institution a few years earlier.
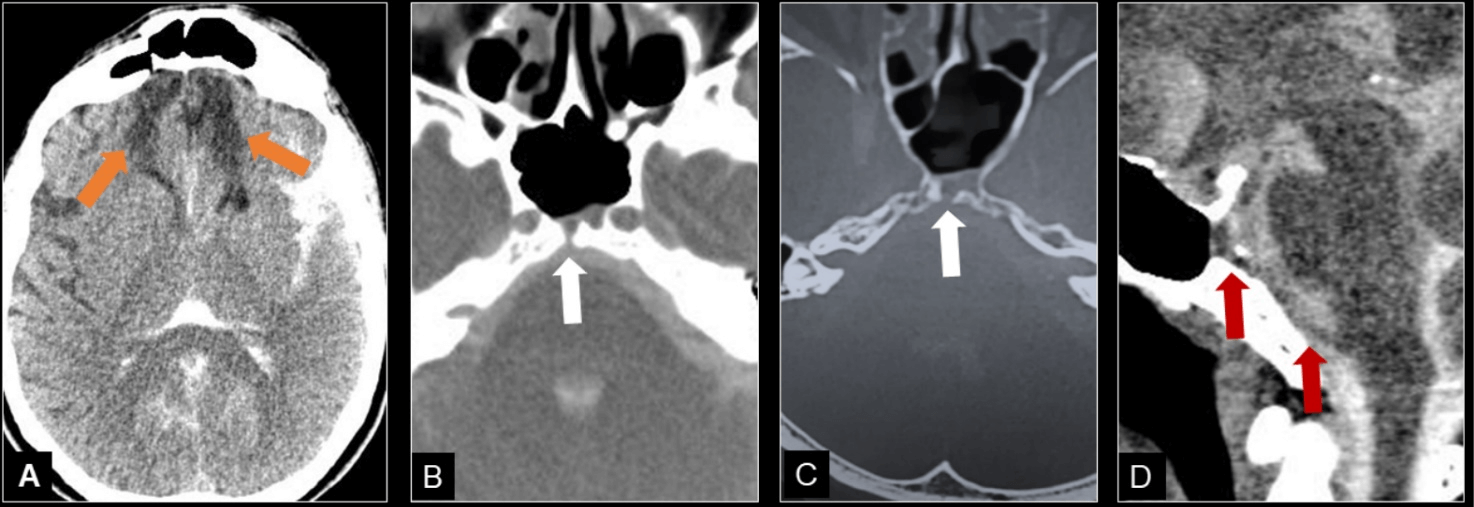
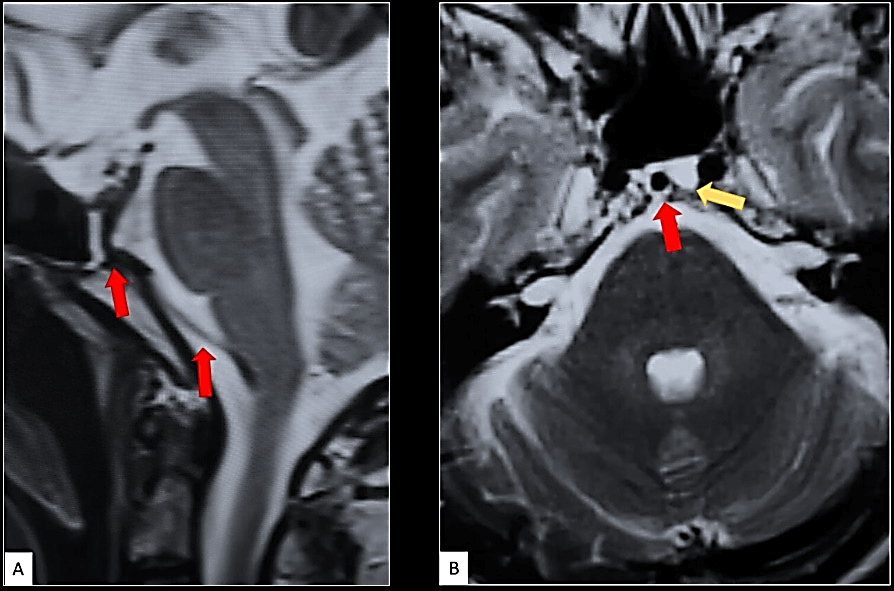
The patient underwent CT-cisternography and brain MRI. These imaging methods showed brain contusions sequelae (Figure 1A) and traumatic linear skull base fracture in the central portion of the clivus with direct communication between the sphenoid sinus and the prepontine cisterna (Figure 1B). These imaging modalities also showed entrapment of the basilar artery into the sphenoid sinus and CSF fistula (Figures 1 & 2). Despite the potential risk of occlusion or stenosis of the basilar artery, there were no signs of vascular injury such as ischaemic stroke.
Figure 1: CT-cisternography. A, B & C) Axial and D) Sagittal Images with bone and soft tissue windows show frontobasal contusions sequelae (orange arrows), clival fracture with communication between the sphenoid sinus and the prepontine cistern (white arrows) and basilar artery entering the sphenoid sinus (red arrows), CSF fistula (C & D).
Figure 2: MRI. A) Sagittal and B) Axial T2WI Images show clival fracture with stretching and entrapment of the basilar artery into the sphenoid sinus (red arrows) and CSF fistula (yellow arrow). There were no signs of stroke in the vertebrobasilar territory.
Discussion
Clivus bone fractures are uncommon and usually result from high-impact cranial injury [1]. The majority of clivus bone fractures appear as linear fractures on CT and can be classified into three types: longitudinal, transverse and oblique [2]. Longitudinal fractures are associated with 70 to 80% mortality secondary to vertebrobasilar and brainstem injury [3].
Herniation of the vertebrobasilar vessels is rare, with only a few reported cases. Almost all of these patients died, and autopsy demonstrated occlusion or thrombosis of the trapped vessel [4]. Herniation of the basilar artery may be associated with clivus bone fractures. Rare cases have been reported in which the basilar artery becomes incarcerated within a fractured clivus [5-7]. Among the reported cases of clivus fracture associated with basilar artery entrapment, all evolved with brainstem and cerebellar infarction [1, 2, 4, 8].
In our case, the basilar artery herniated into the sphenoid sinus through a longitudinal clivus bone fracture, without infarction of the brainstem and cerebellum, as demonstrated in the CT and MRI images. Another complication associated with skull base fracture is CSF fistula. In previous reports, CSF fistula occurred in 7.7% of patients with fractured clivus [9]. Our patient presented with a history of rhinorrhea and severe postural headache, with CSF fistula evidenced by CT- Cisternography and MRI (Figures 1 & 2).
The presence of CSF fistula represents a risk to the patient because it can be a gateway for infections in the central nervous system. Its recognition in imaging studies, as well as in the presence of rhinorrhea, is essential for the adequate management of these patients.
Conclusion
The entrapment of the basilar artery into the sphenoid sinus secondary to traumatic clivus fractures carries a potential risk of basilar artery stenosis or occlusion, resulting in significant morbidity and mortality, due to ischaemia and infarction of the brainstem and cerebellum. Despite the potential risk of occlusion or stenosis of the basilar artery, our patient surprisingly did not show any signs of ischaemic stroke. To our knowledge, this is the first case in the literature showing basilar artery herniation into the sphenoid sinus without signs of brain infarction.
The imaging studies such as computed tomography and MRI play a crucial role in diagnosing this condition, that although uncommon, require an accurate diagnosis and early intervention to avoid possible neurological sequelae.
Financial Disclosure
None.
Author Contributions
Laíse Ramos Neri: Conception, organization and execution of the case report project, writing of the first draft and review and critique of the manuscript. Bruno Siqueira Campos Lopes: Conception, organization and execution of the case report project. Review and critique of the manuscript. Jorge Luís Wollstein Moritz: Conception, organization and execution of the case report project, writing of the first draft and review and critique of the manuscript. Lázaro Luís Faria do Amaral: Conception, organization and execution of the case report project, writing of the first draft and review and critique of the manuscript. Christiane Monteiro de Siqueira Campos: Conception, organization and execution of the case report project. Review and critique of the manuscript.
Article Info
Article Type
Case ReportPublication history
Received: Mon 13, Jul 2020Accepted: Wed 29, Jul 2020
Published: Fri 07, Aug 2020
Copyright
© 2023 Laíse Ramos Neri. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2020.03.01
Author Info
Laíse Ramos Neri Bruno Siqueira Campos Lopes Jorge Luís Wollstein Moritz Lázaro Luís Faria do Amaral Christiane Monteiro de Siqueira Campos
Corresponding Author
Laíse Ramos NeriNeuroradiology Department, BP Medicina Diagnóstica - Hospital da Beneficência Portuguesa de São Paulo, São Paulo, Brazil
Figures & Tables
References
- Pavan Khanna, Matthew Bobinski (2010) Computed Tomography and Magnetic Resonance Imaging of a Basilar Artery Herniation into the Sphenoid Sinus. Skull Base 20: 269-273. [Crossref]
- Arthur Wang, John Wainwright, Jared Cooper, Michael S Tenner, Adesh Tandon (2017) Basilar Artery Herniation into the Sphenoid Sinus Secondary to Traumatic Skull Base Fractures: Case Report and Review of the Literature. World Neurosurg 98: 878.e7-878.e10. [Crossref]
- G Corradino, A L Wolf, S Mirvis, J Joslyn (1990) Fractures of the clivus: classification and clinical features. Neurosurgery 27: 592-596. [Crossref]
- A Bala, N Knuckey, G Wong, G Y F Lee (2004) Longitudinal clivus fracture associated with trapped basilar artery: unusual survival with good neurological recovery. J Clin Neurosci 11: 660-663. [Crossref]
- D C Anthony, S K Atwater, M P Rozear, P C Burger (1987) Occlusion of the basilar artery within a fracture of the clivus. J Neurosurg 66: 929-931. [Crossref]
- J W Loop, L E White Jr, C M Shaw (1964) Traumatic occlusion of the basilar artery within a clivus fracture. Radiology 83: 36-40. [Crossref]
- W P Sights Jr (1968) Incarceration of the basilar artery in a fracture of the clivus. J Neurosurg 28: 588-591. [Crossref]
- Rami Kaakaji, Eric J Russell (2004) Basilar Artery Herniation into the Sphenoid Sinus Resulting in Pontine and Cerebellar Infarction: Demonstration by Three-Dimensional Time of-Flight MR Angiography. AJNR Am J Neuroradiol 25: 1348-1350. [Crossref]
- Alexander Winkler Schwartz, José A Correa, Judith Marcoux (2015) Clival fractures in a level I trauma center. J Neurosurg 122: 227-235. [Crossref]
