Esophageal Involvement of Pemphigus Vulgaris
A B S T R A C T
Pemphigus is an autoimmune and life-threatening disease. Esophageal involvement of pemphigus vulgaris is rare. The most common presenting symptoms are odynophagia and dysphagia. Here, I present one cases of pemphigus vulgaris presenting with dysphagia because of esophageal involvement of the disease. In case, a 27-year-old female patient with a prior diagnosis of pemphigus vulgaris presented with dysphagia. Esophagogastroduodenoscopy showed diffuse mucosal exfoliation and oozing bleeding of the esophagus. The patient recovered after the administration of corticosteroids, pantoprazole and azathioprurine.
Keywords
Pemphigus vulgaris, esophageal involvement, dysphagia
Introduction
Pemphigus is an autoimmune and life-threatening disease characterized by acantholysis (loss of keratinocyte-keratinocyte adhesion) caused by acantholysis (loss of keratinocyte-keratinocyte adhesion) caused by the mucous membrane and skin, directed against keratinocyte cell surface [1]. The main subgroups of Pemphigus are Pemphigus Vulgaris (PV), Pemphigus Foliaseus and Paraneoplastic Pemphigus. The most common subtype of pemphigus is PV [2-5]. PV is seen equally in both sexes. Although it differs geographically, its incidence varies between 0.1 and 0.5 per 100.000 per year [6-10]. In almost all cases during the course of the disease, the multi-layer flat epithelial mucosa, especially the oral mucosa, is involved. Pharyngolaryngeal, conjunctival, genital, anorectal mucosa are less often involved.
Odynophagia and dysphagia are the most common symptoms of esophageal involvement. However, patients with esophageal involvement can sometimes be asymptomatic. It is thought that many esophageal involvement cannot be detected because endoscopy is not performed mostly in patients without esophageal complaints. Some immunohistopathological studies show that esophageal involvement is higher than previous reports [2-4].
Here, I present one cases of pemphigus vulgaris presenting with dysphagia because of esophageal involvement of the disease. In case , a 27-year-old female patient with a prior diagnosis of pemphigus vulgaris presented with dysphagia. Esophagogastroduodenoscopy showed diffuse mucosal exfoliation and oozing bleeding of the esophagus. The patient recovered after the administration of corticosteroids, pantoprazole and azathioprurine.
Case Report
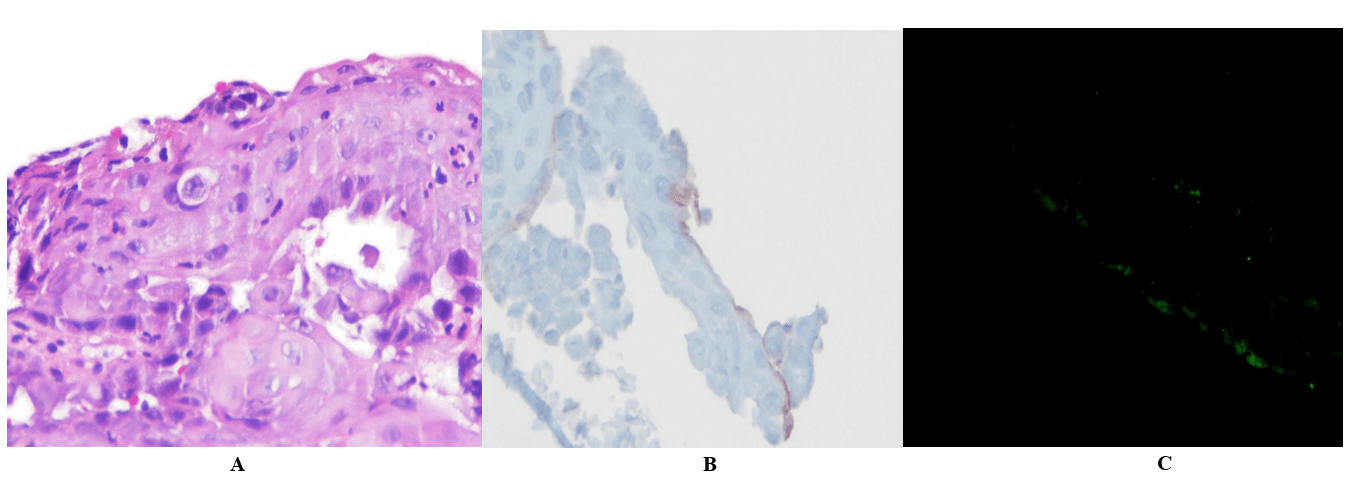
A 32-year-old woman complained about difficulty swallowing and pain in her chest about 3 months ago. The patient applied to our gastroenterology outpatient clinic with his current complaints and an upper gastrointestinal system endoscopy was performed. In the esophageal mucosa, an appearance that started around 20 cm, was circular, widespread, erosional, hemorrhagic and slightly narrowing in the lower region. Two biopsies were taken from here. The esophageal lumen was naturally observed. The Z line was crossed at 40.cm from the front incisors. At the pathology report, although no specific findings are seen in the DIF examination, it is rare with focal C3 accumulation and immunohistochemical examination. C4d positivity suggests an immunological mechanism. Intraepidermal suprabasal dissociation supports the diagnosis of pemphigus vulgaris.
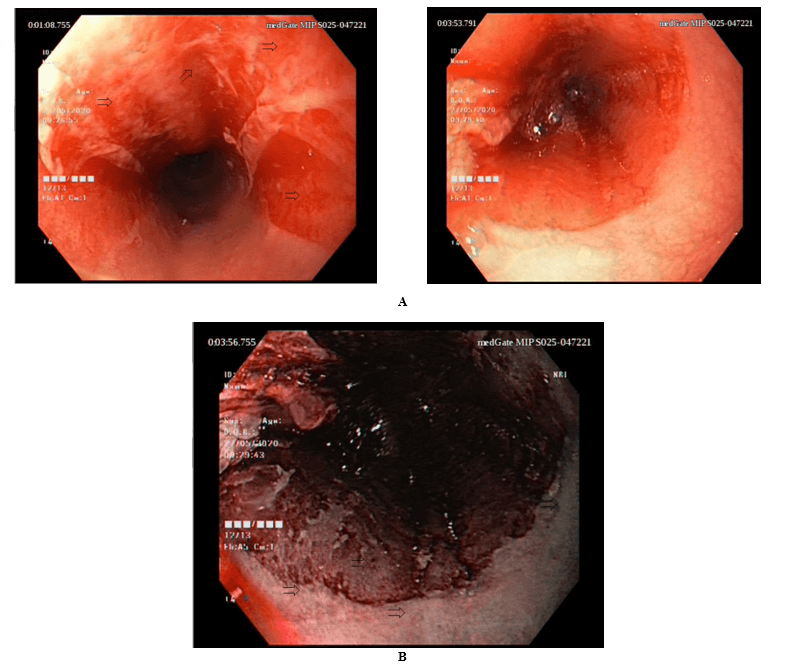
Figure 1: A) Endoscopic view of esophagus, showing erosions and sheets of sloughed mucosa (arrows). B) Endoscopic (Narrow Band Imaging-NBI) view of esophagus, showing erosions and sheets of sloughed mucosa (arrows).
Figure 2: A) Intraepithelial dissociation and acantholytic cells (H-E, x100). B) Accumulation surrounding squamous cells with anti-C4d antibody in immunohistochemical examination. C) C3 accumulation with DIF.
A biopsy was taken by monitoring vesicle-nodular lesions in the mid-esophagus (Figure 1a & 1b). Starting from the biopsy site, it was observed that the esophageal mucosa was separated from the underlying tissue enveloping the esophageal lumen all around (Figure 2). Pathology report: Although no specific findings are seen in the DIF examination, it is seen rare with focal C3 accumulation and immunohistochemical examination. C4d positivity suggests an immunological mechanism. Intraepidermal suprabasal dissociation evaluated in favor of pemhigus vulgaris.
Discussion
The incidence of PV varies from 0.5 to 3.2 cases per 100,000, with an approximately equal male-to-female ratio.6 PV is a potentially life-threatening disease, with a mortality rate of approximately 5–15%. Complications secondary to the use of high-dose corticosteroids contribute to the mortality rate. Morbidity and mortality are related to the extent of disease, the maximum dose of systemic steroids required, and the presence of other diseases. Prognosis is worse in older patients with extensive disease. The pharyngo-laryngeal, genital, anorectal, and conjunctival mucosa are less commonly involved. Odynophagia and dysphagia are the usual complaints in patients with esophageal pemphigus.
Systemic corticosteroid therapy is effective at reducing or eliminating the clinical manifestations of PV, with as high as 400 mg of prednisone being administrated daily for patients with severe involvement. Oral or intravenous administration of cyclophosphamide, azathioprine, cyclosporine, and methotrexate may allow the reduction of corticosteroid dosage. Even with immunosuppressive therapy, up to 10% of patients die from their disease, because of electrolyte loss, wound infection, or treatment complications [10-14].
The patient was started on proton pump inhibitor and sucralfate therapy. Steroid and azathiopurine treatment was started with the recommendation of the dermatology clinic. The patient's complaints of swallowing difficulties disappeared, the patient is under pemphigus and his treatment is still ongoing. The patient recovered after the administration of corticosteroids, pantoprazole and azathioprurine.
As conclusion; pemphigus is an autoimmune and life-threatening disease. Esophageal involvement of pemphigus vulgaris is rare. The most common presenting symptoms are odynophagia and dysphagia. If the patient with pemphigus has dysphagia, endoscopy should be done.
Article Info
Article Type
Case ReportPublication history
Received: Wed 19, Aug 2020Accepted: Mon 31, Aug 2020
Published: Mon 07, Sep 2020
Copyright
© 2023 Vedat Goral. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.03.12
Author Info
Vedat Goral Ali Balevi Sevilay Aligulu Rukiye Nilgun Erdogan
Corresponding Author
Vedat GoralDepartment of Gastroenterology, Istanbul Medipol University School of Medicine, Istanbul, Turkey
Figures & Tables
References
- Lili L, Morris T, Laura B, Cristina H (2012) Isolated Pemphigus Vulgaris to the Esophagus: A Case Report With Literature Review. Am J Clin Pathol 138: A111.
- Sandra Faias, Pedro Lage, Fernanda Sachse, Anabela Pinto, Paulo Fidalgo et al. (2004) Pemphigus vulgaris with exclusive involvement of the esophagus: case report and review. Gastrointest Endosc 60: 312-315. [Crossref]
- N S Goldberg, S S Weiss (1989) Pemphigus vulgaris of the esophagus in women. J Am Acad Dermatol 21: 1115-1118. [Crossref]
- Kanataki K, Kimura K (1975) Pemphigus vulgaris involving the esophagus. Rinsho Hifuka 29: 6-7.
- L M Barnes, M L Clark, S A Estes, G L Bongiovanni (1987) Pemphigus vulgaris involving the esophagus. A case report and review of the literature. Dig Dis Sci 32: 655-659. [Crossref]
- G M Palleschi, E M Cipollini, T Lotti (2002) Development of oesophageal involvement in a subject with pemphigus vulgaris: a case report and review of the literature. J Eur Acad Dermatol Venereol 16: 405-408. [Crossref]
- Angelo Gualberto de Macedo, Erika Ruback Bertges, Luiz Carlos Bertges, Renata Alvim Mendes, Thais Abranches Bueno Sabino Bertges (2018) Pemphigus Vulgaris in the Mouth and Esophageal Mucosa. Case Rep Gastroenterol 12: 260-265. [Crossref]
- P Narasimha Rao, Aruna Samarth, Sanjeev J Aurangabadkar, Bajrang Pratap, T S S Lakshmi (2006) Study of upper gastrointestinal tract involvement in pemphigus by esophago-gastro-duodenoscopy. Indian J Dermatol Venereol Leprol 72: 421-424. [Crossref]
- Sooyun Chang, Soo Jung Park, Sun Wook Kim, Moo Nyun Jin, Jung Hee Lee et al. (2014) Esophageal involvement of pemphigus vulgaris associated with upper gastrointestinal bleeding. Clin Endosc 47: 452-454. [Crossref]
- Rana Muhammad Usman, Qasim Jehangir 1, Muhammad Bilal (2019) Recurrent Esophageal Stricture Secondary to Pemphigus Vulgaris: A Rare Diagnostic and Therapeutic Challenge. ACG Case Rep J 6: e00022. [Crossref]
- Wafae Raffas, Badreddine Hassam (2014) Esophageal involvement during pemphigus vulgaris. Pan Afr Med J 17: 118. [Crossref]
- Paolo Cecinato, Liboria Laterza, Loredana De Marco, Annamaria Casali, Magda Zanelli et al. (2015) Esophageal involvement by pemphigus vulgaris resulting in dysphagia. Endoscopy 47: E271- E272. [Crossref]
- Katharine A Ozeki, Thomas A Zikos, John O Clarke, Irene Sonu (2020) Esophagogastroduodenoscopy and Esophageal Involvement in Patients with Pemphigus Vulgaris. Dysphagia 35: 503-508. [Crossref]
- M Fukuchi, S Otake, H Naitoh, H Shoji, J Yamagishi et al. (2011) A case of exfoliative esophagitis with pemphigus vulgaris. Dis Esophagus 24: E23-E25. [Crossref]
