Gallbladder Volvulus: Diagnosis and Management of a Rare Cause of Acalculous Cholecystitis
A B S T R A C T
Gallbladder volvulus is a rare cause of acalculous cholecystitis which clinically presents as acute abdomen and can rapidly evolve in a severe life-threatening sepsis. Awareness is crucial for differential diagnosis leading to the early and effective treatment. We present the case of an elderly woman who underwent laparoscopic cholecystectomy after pre-operative ultrasound diagnosis of gallbladder volvulus.
Keywords
Gallbladder, volvulus, acute cholecystitis, acalculous cholecystitis, acute abdomen, emergency surgery
Introduction
Gallbladder volvulus is a rare life-threatening condition which clinically presents as acute abdomen which can rapidly evolve in peritonitis and sepsis. Due to its rarity, gallbladder volvulus has been unfrequently reported in the literature, usually as case report or small case series. This disorder is generally associated to anatomical anomalies of the gallbladder’s attachment to the liver with the presence of a mobile cholecystic mesum. Gallbladder volvulus is usually observed in the elderly with more than 85% of the cases aged between 70 and 90 years. Despite imaging innovations, a precise diagnosis is made in less than 10% of the cases. Misdiagnosis of acalculous cholecystitis often leads to conservative treatment which is generally unsuccessful due to the underlying ischaemic necrotic degeneration. Thereafter, a correct diagnosis is generally made only during emergency cholecystectomy which represents the gold standard for treatment.
We present a case of gallbladder volvulus diagnosed pre-operatively, which was treated by laparoscopic cholecystectomy. We also report some indications for allowing an early diagnosis and attempting the prompt treatment of this rare condition.
Case Report
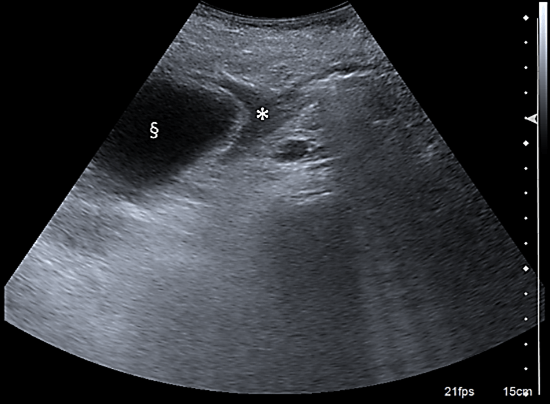
An 81-year-old woman was admitted to the Emergency Department for abdominal pain in the right hypochondrium. No fever or gastrointestinal symptoms were present and blood tests were normal. Abdominal ultrasound was non-diagnostic since the gallbladder presented no gallstones or signs of inflammation. The patient was then discharged with a diagnosis of biliary colic and indication for medical treatment. Due to persistence of abdominal pain, the patient referred again to the Emergency Department two days later. This time, blood tests showed an increase in white blood count (Neutrophils 9.38*109/L, n.v 2.00-7.00*109/L) and CRP (138 mg/L, n.v <5 mg/L), and a slight increase in direct bilirubin (0.97 mg/dL, n.v <0.35 mg/dL). Abdominal ultrasound showed free pericholecystic fluid, thickening of the wall of the gallbladder and no gallstones. Intrahepatic biliary ducts presented a slight dilatation with no clear signs of choledocholithiasis. A diagnosis of acalculous cholecystitis was made and surgical evaluation was requested. Clinical examination showed abdominal tenderness on palpation in right hypochondrium with positive Murphy and Blumberg’s signs. To exclude the presence of bile duct obstruction and further clarify the diagnosis of acute alithiasic cholecystitis, abdominal ultrasound was repeated. This second examination showed a clear “Phrygian cap” sign (Figure 1) which led to the diagnosis of gallbladder volvulus.
Figure 1: Ultrasound cross-section of the gallbladder (§) shows thickened walls due to acute inflammation. The “Phrygian cap” sign is pathognomonic for gallbladder volvulus (*) and led to the diagnosis in the case presented.
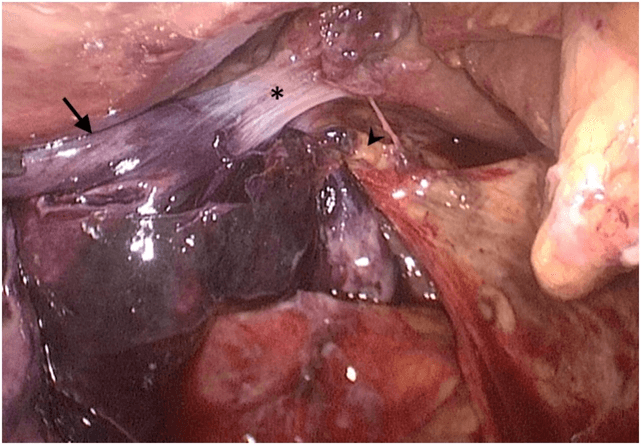
The patient underwent laparoscopic cholecystectomy on the same day of admission. Laparoscopic exploration confirmed the presence of acute peritonitis delimitated to the right hypochondrium by previous surgery adhesions. The gallbladder’s wall was interested by a necrotic process and the evacuated content was hematic in line with the suspected ischaemia due to vascular strangulation (Figure 2). A gallbladder torsion on its long axis was then confirmed and, after derotation, a wandering gallbladder was found. No connections to the liver were found except for a loose and thin band of peritoneum at the level of the infundibulum (cholecystic mesum). This thin connection was the pivot point which caused the organ torsion. After derotation, the identification of Calot’s triangle structures was easy and laparoscopic cholecystectomy was performed. Post-operative course was uneventful, and the patient was discharged on post-operative day two after inflammatory markers and bilirubin levels returned to normal range.
Figure 2: Intraoperative laparoscopic view after derotation of the gallbladder. The cholecystic mesum (*) is characteristic of a Type B anomaly of gallbladder fixation to the liver. It represented the pivot point for the torsion of the gallbladder. Strangulation of the cystic duct and artery (arrowhead) caused ischaemia and necrotic degeneration of the gallbladder wall (arrow).
Discussion
Since the first description of a gallbladder volvulus in 1898 by Wendel, more and more cases have been reported in literature [1]. A recent literature review by Moser et al. reported 477 cases of gallbladder volvulus [2]. Considering the great number of cholecystectomies performed every year all over the world it can be considered an extremely rare condition. It presents a peak of incidence in elderly patients (>70 years) with a male/female ratio of 5:1 [2-4]. These patients often come to physicians’ attention for an acute cholecystitis-like syndrome, but it is not uncommon a septic presentation with peritonitis [5].
According to anatomical and autoptic studies the most important causes of cholecystic torsion are anatomic anomalies in the connections with the liver deriving from an incomplete embryologic migration of the gallbladder [3]. There are two predisposing anatomical variations, reported in about 5% of the Western population, which can increase the risk of gallbladder torsion [6, 7]. In Type A anomaly the gallbladder is completely intraperitoneal and wanders free connected to the liver only by a long and large cholecystic mesum which can turn into a pivot point leading to malrotation. In Type B anomaly, the gallbladder is detached from the liver and the infundibulum and the cystic duct are connected to the lower face of the liver by a long peritoneal fold whose short implant base can lead to gallbladder torsion on its long axis. Other classifications have been reported since gallbladder rotation can be complete (more than 180º) or incomplete (less than 180º), clockwise or anti-clockwise [2, 5]. The higher incidence of gallbladder volvulus in the elderly can be explained by the association of predisposing anatomic anomalies with age-dependent tissue alteration such as reduction in body visceral fat and tissue elasticity, spinal deformations and visceral ptosis [8]. Increased colonic and gastric peristalsis, stypsis, abdominal traumas or visceral adhesions, can act as triggers for gallbladder torsion [2].
Independently from its pathophysiologic etiology, gallbladder volvulus often presents as an acute event characterized by a clinical presentation similar to acute lithiasic cholecystitis. Clinical history often shows previous episodes of abdominal pain, probably associated with torsion and spontaneous derotation. Physical examination is generally aspecific and blood tests may be normal except for an aspecific increase in inflammatory markers. Gallbladder volvulus should be considered whenever an acalculous acute cholecystitis is diagnosed in the elderly. Ultrasonography generally shows aspecific signs of inflammation (free pericholecystic fluid, wall thickening) but an accurate evaluation can highlight addressing signs such as a free wandering gallbladder, a "knot"-like hyperechoic nodular appearance of the coiled cystic duct, the body of the gallbladder with a pluriloculated aspect or the “Phrygian cap” aspect of the gallbladder [9-12].
In the case presented in this report we were able to highlight a “Phrygian cap” aspect of the gallbladder which led us to the diagnosis of gallbladder volvulus. A fast and specific diagnosis allowed us to perform surgical intervention within few hours from admission. Cholecystectomy is indeed the gold standard for treatment. Medical treatment is generally unsuccessful and surgery delay is associated to a high rate of septic complications (16%) and mortality (4.9-6%) [2, 13]. When a volvulus occurs, blood supply is compromised by cystic artery torsion, resulting in ischaemia and necrotic cholecystitis. A good differential diagnosis should then be made between alithiasic cholecystitis and gallbladder volvulus since a conservative approach could be effective in the former while it often delays resolutive surgery in the latter. In addition, some authors suggest considering elective surgery in presence of a cholecystic mesum or other predisposing anatomical anomalies in order to avoid gallbladder volvulus [2, 6]. As for other causes of acute cholecystitis, cholecystectomy can be safely performed both by open and laparoscopic surgery. No comparisons have been made in gallbladder volvulus series, but the evidence of the benefits associated with laparoscopic cholecystectomy could be reasonably referred to this infrequent condition.
Conclusion
Gallbladder volvulus is a rare but life-threatening condition. There are well-defined risk factors (advanced age, female gender, anatomical anomalies) that should be considered for a correct differential diagnosis in a patient with acute abdominal pain and a suspect of acute alithiasic cholecystitis. Detailed evaluation of ultrasonographic imaging in search for pathognomonic signs of torsion is fundamental for avoiding an unsuccessful non-operative treatment. Emergency cholecystectomy is the gold standard for treatment.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 26, Apr 2021Accepted: Tue 11, May 2021
Published: Wed 09, Jun 2021
Copyright
© 2023 Corrado Pedrazzani. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2021.01.04
Author Info
Cristian Conti Jacopo Graziosi Tommaso Valigi Maria Vittoria d’Addetta Andrea Ciangherotti Tommaso Campagnaro Corrado Pedrazzani Alfredo Guglielmi
Corresponding Author
Corrado PedrazzaniDepartment of Surgical Sciences, Dentistry, Gynecology and Pediatrics, Unit of General and Hepatobiliary Surgery, University of Verona, Verona, Italy
Figures & Tables
References
1.
Wendel AV (1898)
VI. A Case of Floating Gall-Bladder and Kidney complicated by Cholelithiasis,
with Perforation of the Gall-Bladder. Ann Surg 27: 199-202. [Crossref]
2.
Moser L, Joliat GR, Tabrizian P, Di Mare L, Petermann D
et al. (2021) Gallbladder volvulus. Hepatobiliary
Surg Nutr 10: 249-253. [Crossref]
3.
Caliskan K,
Parlakgumus A, Koc Z, Nursal TZ (2009) Acute torsion of the gallbladder: a case
report. Cases J 2: 6641. [Crossref]
4.
Coquaz S, Bruant
P, Regenet N, Lermite E, Pessaux P et al. (2005) Gallbladder volvulus: two
cases report. Ann Chir 130: 252-253. [Crossref]
5.
Amrani Y, Ounani M, Beavogui L, Sedki N, Elabsi M et al. (2006) Gallbladder volvulus: Two cases. Press Med 35:
1479-1481. [Crossref]
6.
Nakao A, Matsuda
T, Funabiki S, Mori T, Koguchi K et al. (1999) Gallbladder torsion: case report
and review of 245 cases reported in the Japanese literature. J Hepatobiliary
Pancreat Surg 6: 418-421. [Crossref]
7.
CORCORAN DB, WALLACE
KK (1954) Congenital anomalies of the gallbladder. Am Surg 20: 709-725.
[Crossref]
8.
Desmaizières FC,
Montemagno S, de Lavernette XB, Magdaleinat P (2002) Torsion of the gallbladder
in an adult: a rare case of acute cholecystitis. Int Surg 87: 87-89. [Crossref]
9.
Regner JL, Lomas
A (2016) Gallbladder Volvulus: A Rare Emergent Cause of Acute Cholecystitis, if
Untreated, Progresses to Necrosis and Perforation. Int J Clin Med Imaging
3: 1000439.
10. Dasyam AK, Koo J, Miller MS, Sell HW Jr, Tublin ME
(2015) The cystic duct knot sign: case report with description of a new
ultrasound sign of gallbladder torsion. Emerg Radiol 22: 445-447. [Crossref]
11. Maeda M, Ishida Y, Okamoto K (1994) Ultrasound
diagnosis of gangrenous cholecystitis due to gallbladder torsion. Rofo
161: 465-467. [Crossref]
12. de Csepel J, Carroccio A, Pomp A (2003) Soft-tissue
images. "Phrygian cap" gallbladder. Can J Surg 46: 50-51. [Crossref]
13. Drubay V, Vanwest
L, Tchanderli R, Van Agt CE (2015) Gallbladder volvulus. Press Med 44:
478-480. [Crossref]
