Gallstone Ileus in the Absence of Gallbladder, Rare Etiology of Bowel Obstruction: A Case Report and Literature Review
A B S T R A C T
Background: Gallstone ileus post-cholecystectomy is extremely rare surgical emergency causing mechanical bowel obstruction. This condition is usually misdiagnosed due to its non-specific clinical features. Radiological investigations are essential to evaluate and diagnose gallstone ileus cases.
Case Presentation: A 92-year-old female patient, cholecystomized, presented to our hospital with a one-week history of an acute confusional state, generalized abdominal pain, and vomiting. The physical examination showed a disoriented patient with a distended abdomen and generalized tenderness, especially in the epigastric area. Hyperactive bowel sounds were audible. Laboratory investigations were non-specific. A plain abdominal X-ray was insignificant. The abdominal ultrasound showed marked abdominal gaseous distention. Then, an abdominal CT scan was performed, revealing an impression of gallstone ileus causing small bowel obstruction with no evidence of fistula formation. So, surgical intervention was decided, and an 8-gram gallstone was exteriorized through an enterolithotomy. The postoperative period was uneventful.
Discussion: Gallstone ileus is an unusual entity that often affects elderly females. The clinical features of gallstone ileus include abdominal pain, abdominal distension, nausea, and vomiting. Diagnosis of gallstone ileus relies on imaging and physical examination. Abdominal CT with contrast provides a definitive diagnostic tool. The surgical options to manage the gallstone ileus can be either one or two-staged enterolithotomy.
Conclusion: Due to the rare etiologic origin of the gallstone ileus in post-cholecystectomy cases, we report the case of a 92-year-old female with an acute confusional state and generalized abdominal pain, found to be caused by detected gallstone ileus, lacking evidence of fistula formation.
Keywords
Gallstone ileus, intestinal obstruction, abdominal pain, cholecystectomy, enterolithotomy, case report
Introduction
Ileus due to gallstones is a rare cause, accounting for 1-4% of all cases of mechanical intestinal obstruction [1, 2]. Moreover, this pathology is extremely rare in post-cholecystectomy cases. Only a few cases of GSI after cholecystectomy are documented in the literature [2-4]. Typically, elderly women with a prolonged history of comorbidities are mostly affected [1]. This condition is explained by various pathophysiological mechanisms ranging from adhesions, fistula formation, and diverticula phenomenon [4, 5]. Clinical and epidemiological pictures of gallstone ileus (GSI) are elusive [6]. Mortality from gallstone obstruction can be as high as 18% in elderly patients, this may be related to comorbidities and delayed presentation [7]. Classically, patients with gallstone ileus presented with non-specific symptoms and intermittent obstructive features [1, 7]. Due to its high sensitivity, Computed tomography (CT) scan is the main diagnostic tool for GSI cases [7]. A better prognosis is achieved through early diagnosis and properly-timed surgical intervention for such cases [7].
Here we report a 92-year-old female patient, cholecystomized, who presented with an acute confusional state in association with generalized abdominal pain found to be caused by GSI post-cholecystectomy with no evidence of fistula formation.
Case Presentation
A 92-year-old female patient, with an unremarkable medical history, presented to our hospital with a one-week history of an acute confusional state. Her drowsy state was followed by generalized abdominal pain was associated with multiple vomiting episodes. The patient’s vomitus was initially composed of yellowish secretions and progressed into the production of feculent material. There was no alteration of bowel habits, no fever, and no jaundice. The physical examination revealed a conscious and oriented patient to person and place but not to time and a distended abdomen with generalized tenderness, especially in the epigastric area. Tympanic and hyperactive bowel sounds were audible. Also, there was no evidence of organomegaly or abdominal mass was detected. Laboratory investigations showed leukocytes 6.4 × 109/L, HB 15.8 g/dL, platelets 226 × 109/L, creatinine 101 umol/l, and liver function test results were unremarkable. Patient’s past surgical history included cholecystectomy. A plain abdominal X-ray was insignificant (Figure 1).
Figure 1: A) plain abdominal X-ray, B) chest X-ray with insignificant findings.
In her previous hospital admission, an abdominal ultrasound was done, showing bilateral grade II nephropathy and marked abdominal gaseous distention. At this point, small bowel obstruction was suspected and an abdominal CT scan with IV and oral contrast were performed, revealing the following findings (Figure 2):
Figure 2: Abdominal CT scan with contrast. A) axial view and B) coronal view showing pneumobilia.
i) Atherosclerotic changes in the aorta and its branch.
ii) The celiac, superior mesenteric, and inferior mesenteric arteries showed normal caliber with no filling defects detected.
iii) Pneumobilia was noted.
iv) The jejunal bowel was seen located anterolateral to the right abdominal wall. There was associated dilatation of jejunal bowel loops air-fluid level up to 3.5cm with abrupt contrast after rounded marginal calcification ring-like appearance suspected calcified gallstone.
v) Normal appearance of liver, pancreas, spleen, both kidneys, adrenals, and urinary bladder.
vi) Bilateral few radiodense pelvic calcifications
vii) Impression was gallstone ileus with a causing small bowel obstruction.
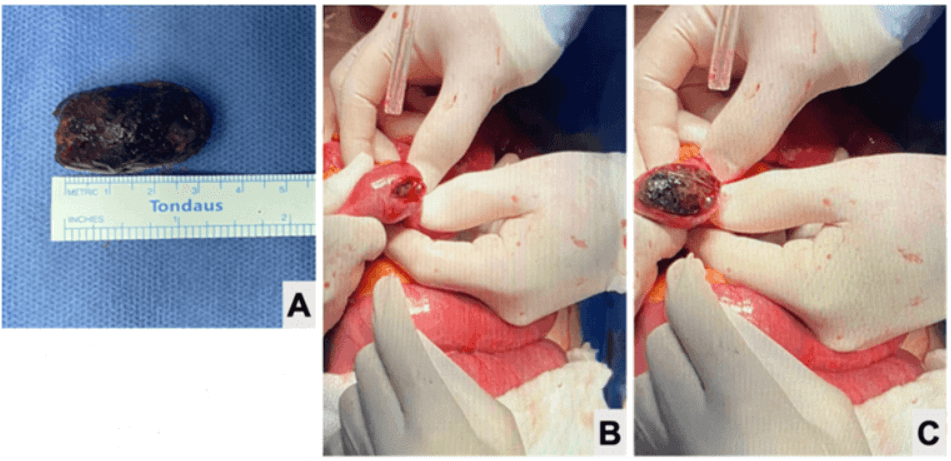
At this point, an emergency laparotomy was planned as the patient was disoriented and haemodynamically unstable. During the procedure, a 10 cm midline incision was made, and the subcutaneous fat and sheath were dissected using diathermy. The bowel exploration was done to identify the structure causing the obstruction. The structure was identified at 125 cm from the ileocecal junction and enterotomy was performed proximally. Through enterotomy, milking was done and an 8-gram gallstone was discovered (Figure 3).
Figure 3: A) 1.7 × 1.7 × 3.2 cm gallstone, weighing 8 grams, and obstructing 125 cm from the ileocecal valve. B & C) Milking the bowel during enterolithotomy.
After that, bowel running and exploration of the remaining bowel were also performed in order to ensure the absence of residual stones. The enterotomy closure and bowel anastomosis were done with a vertical diamond stapled closure and the bowel was milked again to check for any leakage. Abdominal sheath and skin closure were done. The postoperative period was uneventful from a surgical point of view, and the patient was discharged on the twelfth postoperative day.
Discussion
Although gallstone Ileus (GSI) is a rare etiology of mechanical intestinal obstruction, its formation post-cholecystectomy is even rarer [4, 8]. In 1951, the first case of GSI was reported 15 years post-cholecystectomy [9]. According to Sachin et al. and Helmy et al., there were only 17 reported cases of GSI post-cholecystectomy in the literature [2, 5, 7].
GSI is usually preceded by multiple episodes of acute or chronic cholecystitis. Pathophysiologically, multiple inflammatory episodes of the gallbladder with stone lead to adhesion formation with the surrounding structures such as the duodenum, causing mucosa inflammation, erosion, and ischaemia to the GB wall forming a fistula through which a stone may slip causing an obstruction [4, 5]. The obstruction can occur at different gastrointestinal tract levels but more commonly at the terminal ileum and the ileocecal valve [5, 8, 9]. Other mechanisms of GSI involve the passage of gallstone through the Vater papilla following an ERCP and sphincterotomy, and gallstone dislodged from a diverticulum, causing obstruction and Fistula between the bile ducts and intestine [4, 10, 11]. In 2021, Sequndo et al. reported different mechanisms and extraordinary clinical presentation of GSI in cholecystoectomized patients [4]. In our case, the patient was cholecystomized years ago with no evidence of a fistula.
The gallstone’s size and the lumen’s diameter are essential determinants of the stone’s impaction. Gallstones smaller or equal to 2cm usually pass through the bowel through natural processes [4, 5, 8, 9, 12]. In contrast, gallstones> 2-2.5 cm cause an intestinal obstruction with an average size of 4 cm [4, 8]. The current case demonstrated a 1.7 × 1.7 × 3.2 cm gallstone, weighing 8 grams, and obstructing 125 cm from the ileocecal valve. The clinical manifestations of GSI are classically non-specific, including abdominal pain, nausea, vomiting, and abdominal distension, delaying the diagnosis [9, 10, 13, 14]. In the reported case, the patient presented with an acute confusional state in association with generalized abdominal pain and vomiting.
Plain abdominal radiography and Computed Tomography (CT) play an important role in the evaluation and diagnosis of GSI [4, 15]. Radiological studies rely mainly on Rigler’s triad which is comprised of pneumobilia, an ectopic stone, and signs of bowel obstruction [2, 13]. These findings were insignificant in the current case. Only 14-53% of GSI cases presented with Rigler’s triad were reported in the literature [10]. Moreover, the CT scan is the most reliable with sensitivity and specificity reaching more than 90% offering fast diagnosis [2, 10, 12, 13]. In our case, an abdominal CT scan was performed and its findings were previously mentioned in the in-case presentation section. In the literature, the preoperative diagnosis of GSI was achieved in 10-44% of cases [13]. In 2013, Dai et al. documented that the diagnosis of 50% of GSI cases is achieved only at laparotomy [9].
In spite of the fact that the management of GSI varies depending on the patient’s demographics and comorbidities, surgery still is the mainstay of treatment, involving enterolithotomy procedures [9, 13]. Enterolithotomy has three distinct operational strategies as one and two-stage procedures. A one-stage procedure consists of enterolithotomy, cholecystectomy, and fistula closure, in a single surgical time. The two-stage procedure starts initially with enterolithotomy and then after a period of time, cholecystectomy and closure of the fistula [4, 13]. Lastly, enterolithotomy procedure is performed alone at the antimesenteric border [13]. Enterolithotomy alone was the surgical approach for GSI extraction in our case. Multiple studies demonstrated that enterolithotomy is associated with low risks of both morbidity and recurrence in such cases [8, 13]. Many authors reported that one and two-stage procedures are associated with higher mortality and morbidity in comparison with Enterolithotomy [2, 4, 5].
Conclusion
Despite the rarity of GSI post-cholecystectomy, they should be considered in elderly patients with unusual abdominal pain and/or vague non-specific symptoms. Imaging modalities help to diagnose GSI. Enterolithotomy is the most common surgical approach to managing GSI. Due to the dilemma of GSI diagnosis and management, documentation of such cases is highly encouraged in order to overcome the current limitations of resources within the literature.
Conflicts of Interest
None.
Funding
None.
Ethical Approval
Not applicable.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author Contributions
Ali Alenezi: paper writing, editing, picture editing, manuscript drafting. Saqer Alenezi: Literature review, paper writing, and editing. Athary Saleem: Literature review, paper editing, picture editing, and supervision. Mohammed Alshamali: paper editing, and providing pictures. Khaled Alshammari: performed surgery, critical review, picture and paper editing, supervision, and final approval.
Guarantor
Ali Alenezi, M.D., General surgery department, Al-Adan Hospital, Kuwait.
Research Registration
Not applicable.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
Article Info
Article Type
Case ReportPublication history
Received: Mon 20, Feb 2023Accepted: Wed 08, Mar 2023
Published: Fri 17, Mar 2023
Copyright
© 2023 Ali Alenezi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2023.01.04
Author Info
Ali Alenezi Saqer Alenezi Athary Saleem Mohammed Alshamali Khaled Alshammari
Corresponding Author
Ali AleneziDepartment of General Surgery, Al-Adan hospital, State of Kuwait
Figures & Tables


References
1. Souiki T, Mazaz K
(2022) Gallstone ileus: an unusual cause of mechanical intestinal obstruction
in an elderly woman. Pan Afr Med J 42: 40. [Crossref]
2. Teelucksingh S,
Boppana LKT, Goli S, Naraynsingh V (2018) Gallstone ileus 1 year after
cholecystectomy. J Surg Case Rep 2018: rjy153. [Crossref]
3. Lindsey TM, Katz
Unger A, Strickland Jr WM (1975) Gallstone ileus in the absence of a
gallbladder: A case report. Arch Surg 110: 448. [Crossref]
4. Segundo UM, Sánchez
AP, Bernal MPS, Burguete ACP (2021) Gallstone ileus after recent
cholecystectomy. Case report and review of the literature. Int J Surg Case Rep 79:
470-474. [Crossref]
5. Fedele S, Lobascio
P, Carbotta G, Balducci G, Laforgia R et al. (2017) Gallstone ileus in a
ninety-two years old colecistectomized patient after endoscopic biliary sphincterotomy:
a case report. G Chir 38: 299-302. [Crossref]
6. Alzerwi NAN, Idrees
B, Alsareii S, Aldebasi Y, Alsultan A (2021) The Regularity of the Site of
Impaction in Recurrent Gallstone Ileus: A Systematic Review and Meta-Analysis
of Reported Cases. Can J Gastroenterol
Hepatol 2021: 5539789. [Crossref]
7. Helmy NA, Ryska O
(2023) Gallstone Ileus Post-cholecystectomy: A Case Review. Cureus 15: e33345. [Crossref]
8. Desai HK, Rathva
BC, Chauhan PV, Patel RD, Patel RR (2013) Gallstone ileus: a rare cause of
intestinal obstruction. National Journal
of Medical Research 3:
90-92.
9. Dai XZ, Li GQ,
Zhang F, Wang XH, Zhang CY (2013) Gallstone ileus: case report and literature
review. World J Gastroenterol 19: 5586-5589. [Crossref]
10. Chang L, Chang M,
Chang HM, Chang AI, Chang F (2018) Clinical and radiological diagnosis of
gallstone ileus: a mini review. Emerg
Radiol 25: 189-196. [Crossref]
11. Alibegovic E,
Kurtcehajic A, Hujdurovic A, Mujagic S, Alibegovic J et al. (2018) Bouveret
syndrome or gallstone ileus. Am J Med
131: e175. [Crossref]
12. Saedon M,
Gourgiotis S, Salemis NS, Majeed AW, Zavos A (2008) Gallstone ileus one quarter
of a century post cholecystectomy. Ann
Hepatol 7: 258-259. [Crossref]
13. Kirchmayr W,
Mühlmann G, Zitt M, Bodner J, Weiss H et al. (2005). Gallstone ileus: rare and
still controversial. ANZ J Surg 75: 234-238. [Crossref]
14. Kathawa J, Karana R, Piper M (2021). S1560 An Unusual Case of Gallstone Ileus 6 Years Post-Cholecystectomy. The American Journal of Gastroenterology 116: S705.
15. Ibrarullah M, Samantaray PK, Meher S, Bruno WH (2019) Gallstone ileus of upper gastrointestinal tract: A case series. Indian J Gastroenterol 38: 273-275. [Crossref]
