Journals
Guillain Barré syndrome complicated by hip osteoarthropathy
A B S T R A C T
The paraosteoarthropathies are complications occurring in the wake of central but also peripheral neurological pathologies such as Guillain Barré syndrome in its severe form. We report in this case the case of a young patient who presented during the recovery phase a hip osteoarthropathy causing the sitting station.
I N T R O D U C T I O N
Neurogenic paraosteoarthropathies, formerly known as osteomas, correspond to periarticular heterotopic ossifications of the soft tissues, occurring in the wake of a central or peripheral neurological pathology, during a prolonged coma, a long stay in intensive care or after a burn. They are responsible for joint stiffness from which the installation of vicious attitudes hinders the function and comfort of the patient. Paraosteoarthropathies occur more frequently in central and peripheral neurological pathologies. In our observation, we report the case of a neurogenic paraosteoarthropathy occurring in a patient with Guillain Barré syndrome following a short stay in medical resuscitation.
Observation
It is Mr. AE, aged 39, of function, without significant pathological antecedents, who presented following an anti-influenza vaccination a clinical picture made of incomplete tetraplegia of ascending and progressive installation with respiratory disorders and swallowing. The diagnosis was Guillain Barré syndrome, based on a cluster of clinical, neurophysiological (nerve conduction velocity and latency of peripheral nerves at the four limbs) and biological (cyto-albuminological dissociation at 1 study of cerebrospinal fluid). The patient received immunoglobulin-based medical treatment during his stay in medical resuscitation for stabilization of his autonomic disorders. Faced with the gradual improvement, the patient was transferred to a physical medicine and rehabilitation service to continue the overall care.
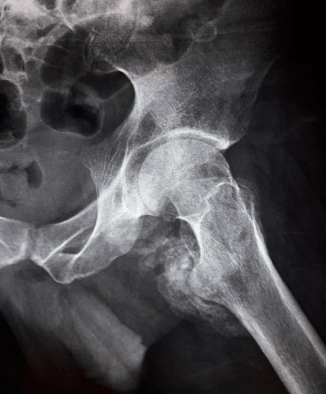
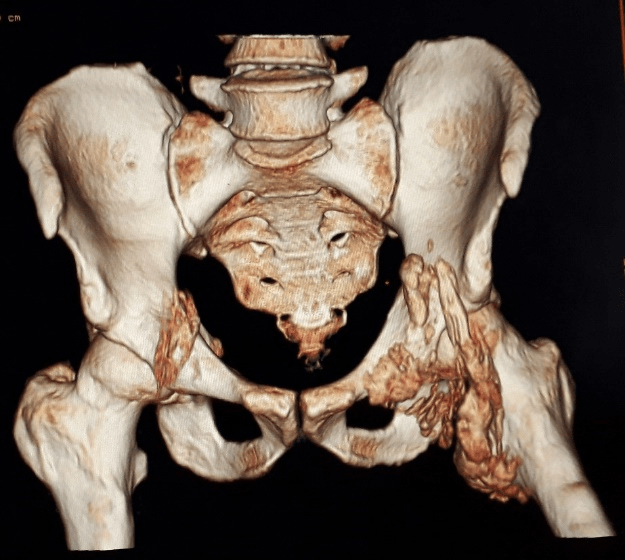
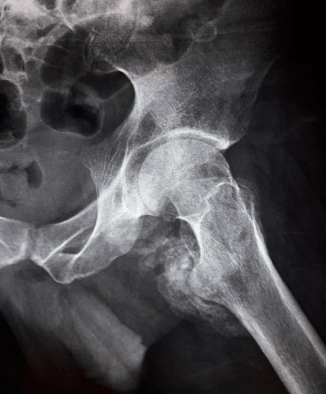
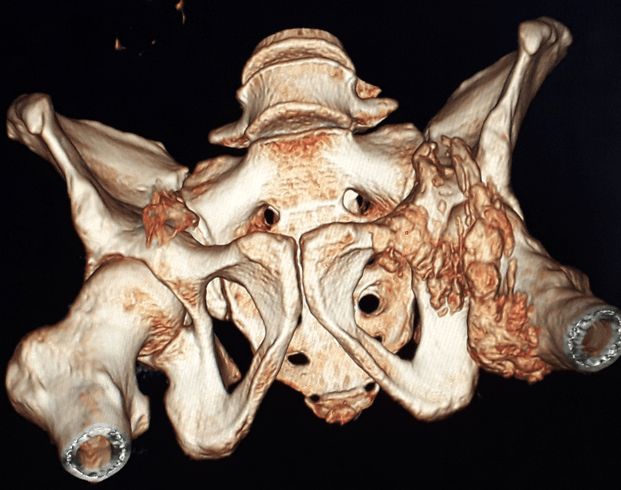
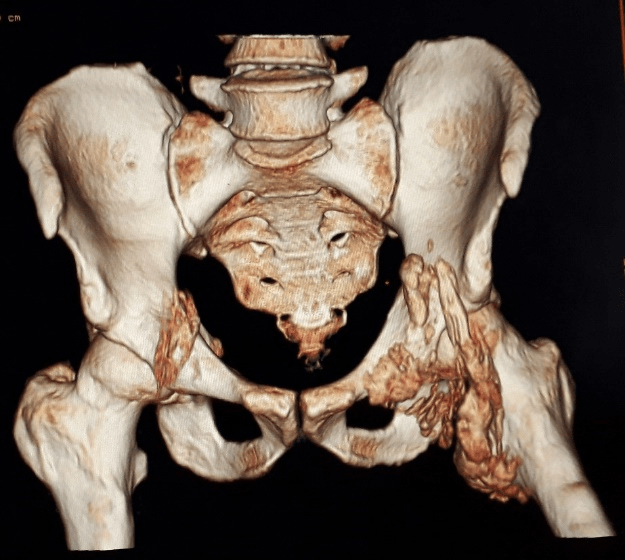
He received daily functional rehabilitation sessions with progressive verticalization, muscular awakening and balance work sitting and standing under the cover of compression stockings and monitoring blood pressure figures. The evolution was marked by the recovery of the engine potential, transfers and turnarounds in the bed but the sitting station was beginning to become troublesome and incorrect on a manual wheelchair. However, the patient experienced mixed pain with left coxofemoral mobilization with localized sensation of heat and swelling. The clinical examination showed a vicious attitude of the whole lower left limb in external adduction-rotation and the presence of inflammatory signs opposite ; with evidence of a hard stop at the flexion of the left hip awakening atrocious mechanical pain hindering the continuation of functional rehabilitation. An inflammatory bioassay was found to be normal with an alkaline phosphatase level equal to twice normal. A standard radiograph of the pelvis opposite showed ectopic juxta-articular ossifications respecting the joint space (Figure 1, 2).
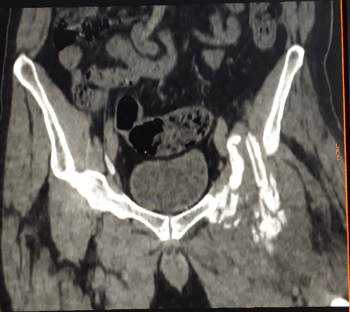
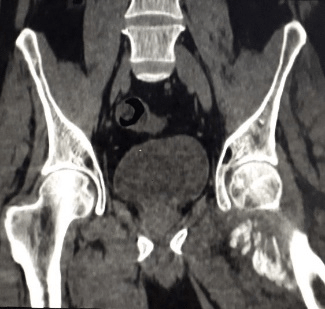
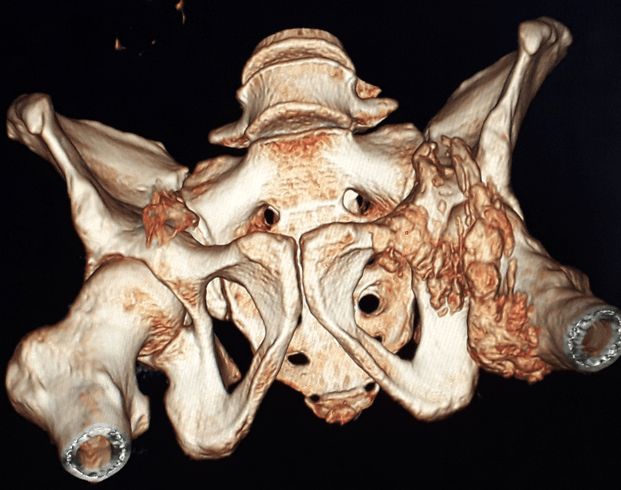
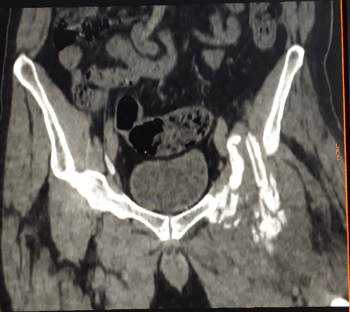
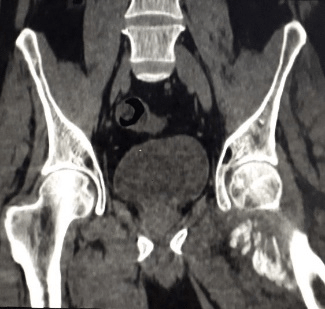
Computed tomography showed the image of paraarticular ossification evoking the neurogenic paraosteoarthropathy of the left hip. (Figure 3, 4, 5, 6). The patient is placed on non-steroidal anti-inflammatory drugs for 4 weeks with intensification of the techniques of gain of the articular amplitudes, manual postures, instrumental and auto-postures. The whole is part of the continuation of the protocol of neurological rehabilitation of Guillain Barré syndrome with respect for patient fatigue.

Discussion
Neurogenic paraosteoarthropathy is a neuro-orthopedic complication characterized by the appearance of ectopic juxta-articular ossification in the peri or para-bone, respecting the joint space. It occurs in the wake of neurological pathologies more central than peripheral and predominates on large joints under lesionnelles.
Ten cases have been reported in the literature following the course of Guillain Barré syndrome [1, 2].
The coxofemoral joint is the most affected (25%) with marked frequency in young adults [3, 4].
The pathophysiology of this complication remains unclear. It involves several factors and several hypotheses:
- Prolonged immobilization associated with passive manipulations [2].
- Lesions of the vegetative nervous system leading to circulatory disorders associated with local microtrauma [1].
These two hypotheses are evoked before the Guillain Barré syndrome in its serious form.
- Involvement of neurogenic hormonal factors.
- genetic predisposition.
- Presence of factors favoring bone formation.
- The clinical picture is presumed in the occurrence of local inflammatory signs in relation to the joint thus reducing the functional area and responsible for the stiffness, the vicious attitude, the pain, even the ankylosis condemning the joint in cause.
All these factors hinder the pursuit of functional rehabilitation and deteriorate the comfort of the patient in the activities of daily life. The phosphocalcic balance precisely the alkaline phosphatases, reflect the process of bone collagen synthesis early. Its dosage allows the detection of neurogenic paraosteoarthropathies; however, its normality does not exclude the diagnosis. In our case, the alkaline phosphatases were dosed two months after the installation of acute polyradiculoneuropathy and the rate was significantly elevated. Radiologically, several examinations contribute to the diagnosis, assess the degree of bone maturation, specify relationships with adjacent structures and look for other subclinical locations. The image objectivized to standard radiography varies according to the evolutionary stage from cloud appearance to density to the appearance of mature bone. Ultrasound can detect early signs six weeks before the appearance of radiological signs [5]. Bone scintigraphy may be required for the detection of infra-radiological locations and to evaluate therapeutic efficacy.
Computed tomography and magnetic resonance imaging; they are prescribed in view of a preoperative lesion report in order to facilitate the surgical decision for a better functional restoration [2]. The therapeutic management must be multiple with establishment of pharmacological and non-pharmacological means. The pharmacological means make use of first-generation bisphosphonates, nonsteroidal anti-inflammatory drugs and low dose radiation therapy.
The functional reeducation essentially the techniques of gain of the articular amplitudes, when it is instituted early makes it possible to maintain a certain functional articular game and to delay as much as possible the installation of articular ankylosis. It also includes physiotherapeutic means to treat the associated pains. Our patient benefited from regular functional rehabilitation sessions with different techniques of gaining joint amplitudes to preserve a good function. In case of significant discomfort not mastered by the conservative treatment, the surgery becomes the only recourse and the last spring to restore the function. The ideal time for surgery depends on the stage of bone maturation that ranges from 12 to 24 months to 34 months [1, 2]. The techniques depend on the location of the joint to be operated, much more difficult so deep as the hip, and the bilateral nature of the lesion. The surgical procedure consists of a complete excision of the bone bridges as a conservative treatment or a prosthetic replacement as a radical treatment. Whatever the surgical procedure with simple suites, a functional rehabilitation protocol started early is essential to maximize the functional results. Anti-inflammatory drugs may be used as a preventive measure to avoid the risk of recurrence estimated at between 6% and 35% [6].
Conclusion
The paraosteoarthropathies are frequent neuro-orthopedic complications in the central neurological pathologies but can also be seen in the course of a peripheral neurological pathology such as the Guillain Barré syndrome in its serious form associated with vegetative disorders and requiring an initial care in medical reanimation. This is an entity to be mentioned early in the first signs to fight against the installation of stiffness likely to evolve into ankylosis.
The care must be global, integrating several medical and paramedical stakeholders to obtain better functional results.
Conflict of Interest
The authors do not declare any conflict of interest.
Article Info
Article History
Case ReportPublication history
Received: 28 February, 2019Accepted: 18 March, 2019
Published: 20 April, 2019
Copyright
© 2018 S. Khalfaoui. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository. All rights reserved.DOI: 10.31487/j.SSG.2018.01.02
Author Info
Corresponding author
S. KhalfaouiDepartment of Physical Medicine and Rehabilitation, Military Training Hospital Mohamed V-Rabat.
Figures & Tables

References
- 1. Boussaadani Soubai R, Abourazzak FZ, Belfkih R, Belahsen F, El Mrini A et al. (2013) Paraostéoarthropathie neurogène et syndrome de Guillain-Barré: à propos d’un cas. Université Sidi Mohammed Ben Abdellah, Faculté de Médecine et de Pharmacie de Fès - Maroc. Rev Mar Rhum 26: 32-35.
- Hatim Abid, Mohamed El Idrissi, Mohamed Shimi, Abodehalim El Ibrahimi, Abdelmajid El Mrini (2015) La para-osteo-arthropathie neurogene dans le syndrome de guillain Barre: complication rare (à propos d'un cas et revue de la littérature). Pan Afr Med J 20: 245. [Crossref]
- Gagnaire P, Petit H, Pujol S, Darigues JF, Richer E (1994) Etude prospective des complications neuro-orthopédiques du traumatisé crânien grave. Ann Réadapt Med Phys 37: 183-188.
- Rebelleix S, Dartigues JF, Sibrac MC, Bara T (1982) Optimisation pour diagnostic précoce de para-ostéo-arthropathie neurogène. Ann Méd Phys 25: 33-40.
- Ryu SR, Kim JH, Choi IS, Han JY, Lee SG (2008) Heterotopic ossification as an unusual complication after Guillain-Barré syndrome: a case report. Arch phys Med Rehabil 89: 564-567. [Crossref]
- Genet F, Schnitzler A, Jourdan C, Denormandie P (2012) CHU-Hôpital Raymond-Poincaré, 104, boulevard Raymond-Poincaré, 92380 Garches, France Paraostéoarthropathie neurogène (POAN): influence du délai opératoire. Revue d’Epidémiologie et de Santé Publique 55: e178-e183.
