Gunshot Wound to Abdomen Causing Life-Threatening Zone I Retroperitoneal Hematoma from Artery of Adamkiewicz
A B S T R A C T
Introduction: Traditionally speaking, all patients with traumatic zone I hematomas should undergo operative exploration because of the high likelihood of injury to the aorta, the inferior vena cava, or one of the major mesenteric vessels.
Case Description: We describe the case of a 26-year-old male patient who presented to our level 1 trauma center after sustaining a gunshot wound to his abdomen. Exploration revealed his main source of bleeding to be due to paraspinal arterial injury, specifically the transection of the artery of Adamkiewicz. Hemostasis was obtained via trans-vertebral packing.
Discussion: Although traditional teaching dictates emergent operative exploration for patients with penetrating abdominal wounds and hemodynamic compromise, little guidance exists in the literature on the operative management of massive bleeding from paraspinal vessels. It is possible that in select cases, interventional radiologic measures might translate into better functional outcomes for patients with similar injuries.
Keywords
Zone I retroperitoneal hematoma, artery of Adamkiewicz, penetrating trauma to paraspinal, vessels
Introduction
Retroperitoneal hematomas are categorized into zones to facilitate management strategies. Traditionally speaking, all zone 1 hematomas are explored both in blunt and in penetrating trauma patients because of the high likelihood of injury to the aorta, the inferior vena cava, or one of the major mesenteric vessels [1-4]. Here, we present the case of a trauma patient who had sustained a gunshot wound to his abdomen resulting in a zone I retroperitoneal hematoma. Upon exploration, however, with the benefit of hindsight, we questioned our paradigm.
Clinical Case
Patient DC is a 26-year-old male with a history of bipolar disorder and schizophrenia who was transferred to our Level 1 Trauma Hospital after sustaining multiple gunshot wounds. He had been found to be hypotensive in the field and was given one unit of packed red blood cells during transfer. On arrival at our facility, the patient was initially hemodynamically stable with heart rate in the 70s and blood pressure in 150s/110s. The secondary exam revealed two gunshot wounds, one to the left anterior flank and another to the right gluteus. His examination was also notable for motor deficit in his right lower extremity. His chest x-ray was normal, but his FAST scan was grossly positive. As he was becoming progressively more hypotensive and diaphoretic, he was taken directly to the operating room for exploration. No additional imaging was done at this time.
Upon entry to the abdomen, there was a large amount of hemoperitoneum, and our institution's massive transfusion protocol was activated. Four-quadrant packing allowed anaesthesia to catch up with resuscitation. Upon removing our packs in a sequential manner, we noted several small liver lacerations that were all amenable to the application of hemostatic agents and packing. The spleen appeared normal, and no gross bleeding was noted in the pelvis. On running the small bowel, we found a large mesenteric hematoma and two small bowel enterotomies in the mid- jejunum that were controlled with staples and a LigaSure device. During this maneuver, we noted a rapidly expansive and pulsatile-appearing retroperitoneal hematoma in zone I with an associated acute drop in the patient's blood pressure despite active and ongoing resuscitation with whole blood.
In response to the above, we placed a supraceliac aortic clamp and performed a modified Mattox maneuver to expose the aorta distally, which we controlled with a vessel loop. Further exploration showed no injury to the aorta, and the clamp was removed after 10 minutes. Again, a drastic drop in the patient's blood pressure alerted us to an unrecognized injury as large amounts of blood was welling up in zone I. Although the bleeding initially appeared to be arterial, we proceeded with performing a Cattell-Braasch maneuver to explore the IVC to no avail, and again, bleeding was controlled with packing. Finally, on our third exploration of zone I, we identified a hole just left of the aorta at about L1-L3 level that had traversed through the entire peritoneal cavity creating a finger-width defect in the anterior body of a lumbar vertebra. The bleeding was identified as arterial in nature, arising directly through this defect. The bleeding was finally controlled with SURGICEL and an EVARREST patch tightly packed into the defect. Given the patient's intermittent hemodynamic instability and developing acidosis, he was left in discontinuity and after placement of a temporary closure device, he was taken to the Surgical Intensive Care Unit for resuscitation. In total, he had received two units of packed red blood cells and six units of whole blood.
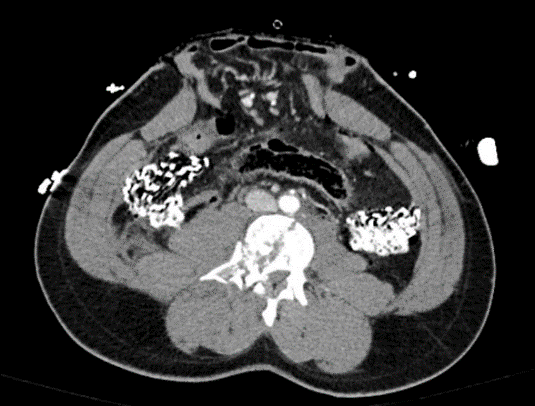
Once stabilized, the patient underwent computed tomography of his chest, abdomen and pelvis with thoracic and lumbar spine reconstructions. Final radiographic reads showed a three-column injury at the level of L3 with an associated fracture of the vertebral body. No active bleeding was noted.
Figure 1: CT scan, performed postoperatively. Representative image showing the patient's L3 three-column fracture, with concern for bone fragments in the spinal canal. Trauma packing in right and left hemiabdomen.
The patient was taken back to the operating room the following day for re-exploration, hemostatic assurance, restoration of intestinal continuity and closure of the abdomen. His recovery was marked by the development of incomplete paraplegia of his bilateral lower extremities. He was discharged from the hospital on postoperative day 22.
Discussion
Retroperitoneal hematomas are common injuries following penetrating trauma to the abdomen. Expert literature recommends exploration of all penetrating zone I hematomas [1-4]. Most commonly, these injuries arise from major abdominal vessels: Aorta, Inferior Vena Cava, Celiac Axis, and Superior or Inferior Mesenteric Arteries [3]. More rare causes include lumbar artery injuries that may be associated with lumbar vertebral fractures [5, 6]. Given the amount of blood loss in our case, the degree of the patient's hemodynamic instability, and the visual confirmation of arterial bleeding through a vertebral defect, we believe that our patient's life-threatening injury arose from the largest of the radiculomedullary arteries: The artery of Adamkiewicz.
To review, the spinal cord's arterial supply is primarily from the anterior spinal artery (ASA) and two posterolateral spinal arteries (PSA) [7, 8]. The ASA arises from the two vertebral arteries and is also supplied from segmental arteries, originating in pairs, from the posterior aspect of the aorta. Below T3, these typically arise as a single vessel at each level [7]. The largest of these is the artery of Adamkiewicz (AKA), also known as the great anterior radiculomedullary artery [7, 8]. It typically arises from the aorta between T8 and L2 and is approximately 0.5mm-1mm in diameter. Injuries to the AKA can cause spinal cord ischaemia [8, 9]. The radiculomedullary arteries are commonly found on CT scan or angiography, helping them be distinguished from other arterial injuries and are readily managed with embolization [10, 11]. Transcatheter embolization allows for a selective approach, ideally improving blood supply to the spinal cord, minimizing the risk of ischaemia.
Figure 2: 1) Posterior spinal arteries; 2) anterior spinal artery; 3) great anterior radiculomedullary artery or artery of Adamkiewicz; 4) medial musculocutaneous branch; 5) lateral musculocutaneous branch; 6) posterior radiculomedullary artery; 7) retrocorporeal arteries; 8) spinal branch; 9) posterior (dorsal) branch; 10) anterior (ventral) branch; 11) left segmental artery (posterior intercostal artery); 12) right segmental artery (posterior intercostal artery); 13) aorta.
Traditional teaching dictates emergent operative exploration for patients with penetrating abdominal wounds and hemodynamic compromise [1-4, 12]. Hemodynamically stable patients may be first to receive cross-sectional imaging to delineate injury pattern, although this is more commonly reserved for patients who had sustained blunt trauma [1].
There is little guidance in the literature about the best open operative management of injuries to paraspinal vessels, particularly without preoperative imaging. A left-sided medial visceral rotation is the preferred exposure for suprarenal aortic injuries following gaining proximal control, while a suprarenal IVC injury is best exposed through right-sided medial visceral rotation [3, 4]. The lumbar spine can be identified through either approach. Definitive intraoperative identification of the injured vessel is quite challenging, if not impossible [13]. Had we obtained a computed tomography scan first, we might have decided to opt for control of the bleeding with interventional radiologic measures, possibly preserving more blood flow to the spinal cord that might have translated into a better functional outcome for our patient. Perhaps we should lower our threshold to obtain a preoperative CT scan in the case of penetrating trauma patients where temporary hemodynamic support can be achieved with transfusion. Ultimately, though, understanding the patient's initial injury, trajectory and common wound patterns remains the cornerstone of our management algorithm.
Article Info
Article Type
Case ReportPublication history
Received: Mon 15, Jun 2020Accepted: Mon 29, Jun 2020
Published: Sat 04, Jul 2020
Copyright
© 2023 Piroska Kopar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.01.04
Author Info
Corresponding Author
Piroska KoparDepartment of Surgery, Washington University School of Medicine, Saint Louis, Missouri, USA
Figures & Tables

References
- Feliciano DV (1990) Management of traumatic retroperitoneal hematoma. Ann Surg 211: 109-123. [Crossref]
- Evans J (2007) Top Knife: The Art and Craft of Trauma Surgery. Ann R Coll Surg Engl 89: 453-454. [Crossref]
- Kobayashi LM, Costantini TW, Hamel MG, Dierksheide JE, Coimbra R (2016) Abdominal vascular trauma. Trauma Surg Acute Care Open 1: e000015. [Crossref]
- Chapellier X, Sockeel P, Baranger B (2010) Management of penetrating abdominal vessel injuries. J Visc Surg 147: e1-e12. [Crossref]
- Nakao S, Ishikawa K, Ono H, Kusakabe K, Fujimura I et al. (2019) Radiological classification of retroperitoneal hematoma resulting from lumbar vertebral fracture. Eur J Trauma Emerg Surg 45: 353-363. [Crossref]
- Sclafani SJ, Florence LO, Phillips TF, Scalea TM, Glanz S et al. (1987) Lumbar arterial injury: radiologic diagnosis and management. Radiology 165: 709-714.
- Santillan A, Nacarino V, Greenberg E, Riina HA, Gobin YP et al. (2012) Vascular anatomy of the spinal cord. J Neurointerv Surg 4: 67-74. [Crossref]
- Lindeire S, Hauser JM (2020) Anatomy, Back, Artery Of Adamkiewicz. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Taterra D, Skinningsrud B, Pękala PA, Hsieh WC, Cirocchi R et al. (2019) Artery of Adamkiewicz: a meta-analysis of anatomical characteristics. Neuroradiology 61: 869-880. [Crossref]
- Koakutsu T, Aizawa T, Yuzawa H, Itoi E, Kushimoto S (2016) Lumbar artery injury from which the Adamkiewicz artery originated associated with lumbar spine injury: successfully treated by transcatheter arterial embolization. Eur Spine J 25: 124-128. [Crossref]
- Armstrong NN, Zarvon NP, Sproat IA, Schurr MJ (1997) Lumbar artery hemorrhage: unusual cause of shock treated by angiographic embolization. J Trauma 42: 544-545. [Crossref]
- Hirshberg A, Wall MJ Jr, Mattox KL (2002) Bullet trajectory predicts the need for damage control: an artificial neural network model. J Trauma 52: 852-858. [Crossref]
- Marty B, Sanchez LA, Wain RA, Ohki T, Marin ML et al. (1998) Endovascular treatment of a ruptured lumbar artery aneurysm: case report and review of the literature. Ann Vasc Surg 12: 379-383. [Crossref]
- Charles YP, Barbe B, Beaujeux R, Boujan F, Steib J (2011) Relevance of the anatomical location of the Adamkiewicz artery in spine surgery. Surg Radiol Anat 33: 3-9. [Crossref]
