Hat-Trick: On a Case of Hip Replacement Complicated by Dislocation and Infection and Periprosthetic Fracture
A B S T R A C T
Case Presentation: A 79-year-old man with several general medical comorbidities referred to our orthopaedic Unit with dislocation, infection and periprosthetic fracture of a long-stem hip hemiarthroplasty.
Results: A one-stage revision was performed using a dual mobility cup and a standard modular-neck stem, both fixed with antibiotic-loaded cement.
Conclusion: Hip replacement is a common treatment for femoral neck fractures in the elderly population with a significant improvement in the quality of life of patients. Local complications can lead to poor outcomes. The simultaneous presence of dislocation, infection and periprosthetic fracture is a challenge of treatment for the surgeon and the frailty of the patients get this scenario even worse. Every attempt must be driven toward a safe and time-preserving “single-shot” procedure.
Keywords
Hip replacement, infection, dislocation, periprosthetic fracture
Introduction
Femoral hip fractures (FHF) are common, with 1.6 million occur¬ring annually worldwide and an expected occurrence of 6.3 million by 2050 due to the fact that increased age is significantly associated with fracture. The optimal treatment of FHF is still an ongoing debate; surgical options include internal fixation, hemiarthroplasty (HA) and total hip arthroplasty. Hip replacement is commonly performed to treat various hip pathologies, is a cost-effective procedure, and found to be associated with a significant improvement in the quality of life of patients. HA using modular-head partial prostheses is an increasingly popular treatment option and has become a common surgical procedure used to treat elderly patients who have suffered FHFs. Given the increase of HA being performed annually, the number of complications necessitating revision surgery is increasing.
The main complications are prosthetic dislocation, due to sarcopenia in elderly patients and their attempts to regain the pre-injury range of motion, and periprosthetic joint infection (PJI), which potentially impact morbidity and quality of life and may contribute to mortality. Despite improvements in surgical techniques and in the use of antibiotic prophylaxis, PJI remains a major cause of implant failure and need for revision. PJI is associated with both human host-related and bacterial agent-related factors. Periprosthetic fracture remains a major source of reoperation following hip arthroplasty too [1-5]. To our knowledge no cases of HA dislocation simultaneously to periprosthetic infection and in conjunction with periprosthetic fracture have been described in scientific English literature previously.
Case Report
We present a case of a 79-year man who was admitted to the Nephrology Unit in our University Hospital and referred to our Orthopaedic Unit for a consultation, due to a problem in his right hip. The patient presents several comorbidities: anemia; pleural effusion; previous cardiologic problems, thus in pharmacological multiple treatment since 15 years ago; chronic renal failure in hemodialytic therapy three times /week and diabetes mellitus under oral medication. Three months before he underwent right HA for FHF in another Hospital, revised after six weeks for periprosthetic fracture. Non-smoker.
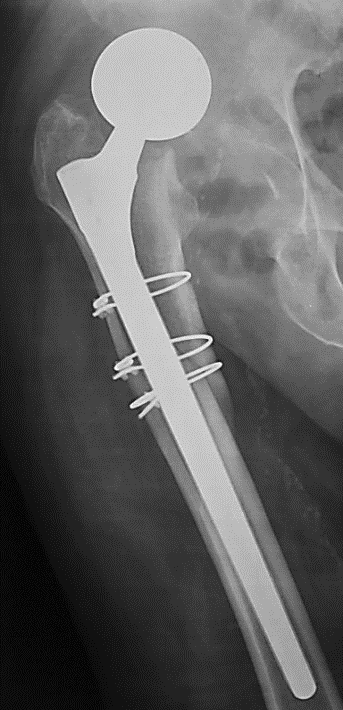
On physical examination he presented lying supine, with the lower right limb shortened, internally rotated and slightly adducted. Pain was provoked by attempts to mobilize the right hip. No altered sensibility on the leg and foot; the dorsalis pedis artery could not be felt because of the swelling. Inability to actively raise the leg. By inspection, the presence of a secreting fistula localized on the surgical scar in the lateral aspect of the upper part of the thigh was noticed. AP view X-ray showed dislocation of a right HA, with long Wagner-type non-modular stem, and three metallic cerclages in the proximal meta-diaphyseal region of the femur, likely used to fix the periprosthetic fracture, simultaneously to the stem exchange (Figure 1). Although no other radiological films were available for comparison, sinking of the stem into the femoral medullary canal seemed as likely. Given the described local and general conditions, the patient was defined as ASA IV score and operative decision was taken to perform a one-stage revision total hip arthroplasty under general anesthesia. Intravenous antibiotics was not discontinued, and thromboembolic prophylaxis was made with enoxaparin.
Figure 1: Dislocation of a long-stemmed hip hemiarthroplasty, used in conjuction with three cerclages to fix a periprosthetic fracture.
We used chlorhexidine for disinfection of the surgical site in the operating room and alcoholic povidone iodine solution just before draping the limb; an iodine-impregnated plastic adhesive tape covered the surgical site. With the patient lying on the contralateral unaffected side, skin was incised on the previous scar removing the tissues around the sinus, the direct lateral approach was used, and the dislocated HA easily identified and removed. The three cerclages from the previous operation were left in situ. Several specimens were taken from superficial and deep layers for postoperative cultural investigation. Acetabulum was cleaned and prepared with motorized reamers paying attention to avoid breakage of the frail bony medial wall; a dual mobility Liberty® cup was cemented in with digital pressurization. The femur was then manually rasped, a distal cement restrictor was used, the medullary canal was cleaned with saline lavage and an injection gun was employed; a Profemur®Xm modular-neck stem was implanted with its centralizer (Figure 2). Both cements were antibiotic loaded with gentamicin and clindamycin. All prosthetic components were manufactured by MicroPort Orthopedics, Arlington, TN. Postoperative days were uneventful: the patient was allowed to cautious mobilization with the assistance of a therapist after removing the intraarticular drain in second postoperative day and weight bearing was permitted with two crutches since removal of staples after two weeks. None of the intraoperative swabs demonstrated growth of any bacterial pathogen. At the latest follow-up, after 10 months since the last surgical procedure, by phone the patient reports to be able of walking for a short distance with one crutch in the left side. No recurrence of infection nor dislocation have occurred so far.
Figure 2: Postoperative X-ray. Cemented total hip replacement was performed, with a dual-mobility cup and a modular-neck stem.
Discussion
HA is a common treatment for FHFs in the elderly population; guidelines and systematic reviews have suggested that cemented fixation is more effective than uncemented and thus surgeons should consider cemented fixation of the stem in the HA treatment of displaced femoral neck fractures in the absence of contraindications even if potential negative effect of using cement is the “bone cement implantation syndrome” (characterized by hypoxia and/or hypotension in combination with an unexpected loss of consciousness which occasionally occurs following cement insertion) [1, 6]. This complication may be fatal. Uncemented HAs -as the one used in the presented case- are placed press-fit in the femur and rely on the primary stability in the cancellous endosteal femoral bone; long-term stability, weeks after the surgery and due to the bond between femur and the stem, is dependent on osseous integration occurring secondary to endosteal microfractures at the time of preparation and subsequent bone ingrowth.
However, bone quality is generally poor in elderly FHF patients, which may lead to periprosthetic fractures during press-fit placement or inadequate bony in-growth post-operatively and thus uncemented HAs are suspected to be associated with a higher risk of periprosthetic fractures [7]. It must be underlined that Vancouver type B periprosthetic femoral fractures are challenging complications and some controversies remain; the aim of the treatment is to ensure sufficiently stable fixation, to restore the length, axis and rotation of the fractured femur, to enable healing of the fracture while preserving the function of the joints and so allowing for rapid mobilization. Periprosthetic fracture treatment is still being debated because an unanimously recognized algorithm has not been defined yet. Indeed, this has been complicated by numerous factors, including the usually advanced age of the patient, the poor bone quality and quantity for stable fixation, the possible endosteal vascular insufficiency due to broaching for the first implant, and eventually the presence of cement in the femoral canal.
The overall clinical outcome among Vancouver type B periprosthetic femoral fractures was satisfactory, however treatment with internal fixation in type B2 and B3 fractures had a significantly longer time to heal and lower mobility than revision cases and open reduction with internal fixation using plates of suitable length and with a sufficient number of screws and cerclage wires, may represent a mechanically and biologically satisfying and be a viable option if bone stock is adequate around uncemented or tapered polished stems [8, 9]. Regarding the surgical approach for HA, there were no evident advantages of the posterior approach the one used in the presented case- and its routine use for fracture-related HA should be questioned. As a matter of fact, compared to the lateral and anterior approaches, no significant differences were found concerning perioperative fractures, wound infections, and hospital length of stay, whilst posterior approach poses an increased risk of dislocation [10]. When a hip dislocation occurs, closed reduction is generally unsuccessful and for those patients with unsuccessful closed reduction, revision arthroplasty should be considered when possible, as this results in a better functional outcome with a lower mortality than excision arthroplasty [11].
During revision, in the presented case we used a dual mobility cup and a modular-neck stem, both fixed to the bone with double antibiotic-loaded cement that, despite a slightly longer operating time, should be the preferred form of treatment for patients at high risk of dislocation and infection for their capability to allow better accuracy in restoring the anatomy and biomechanics of hip joint and to offer the advantage of achieving early high concentrations of the antibiotic directly at the site of infection at the same time [12, 13].
The patient in the present study was affected by several medical pathologies. Comorbidities increase the risks of mortality and infection, that occurs in 1% to 2% of primary HAs and is one of the most devastating and costly complications following total joint arthroplasty and the second most common cause of prosthetic joint failure [3, 4, 14]. Periprosthetic infection is also associated with substantial financial burden on the healthcare system and significant physical and psychological morbidity on patients [14]. Morbidity and cost associated with repeat surgery, prolonged medical treatment and joint immobilization render importance to the accurate and timely diagnosis, and appropriate treatment of prosthetic joint infection [4].
We are well aware that two-stage revision surgery with antibiotic-loaded spacer implantation represents the standard of care for patients who develop chronic infection at the site of a total joint replacement to maintain joint cavity thereby facilitating reimplantation and their use is also intended to deliver antibiotics locally contributing to the cure of infection, but the presented case was not considered as a chronic infection, because the previous operation had been performed six weeks before, and we felt confident to have the opportunity to solve the three concomitant problems arose with a “single-shot” procedure, safe and time-preserving, and to permit an early rehabilitation to our frail patient [13].
Conclusion
In conclusion, the case we have described raises some points for consideration. We suggest the surgical option in this paper as the optimal treatment when a combination of local complications in an elderly and medically frail patient occurs, since antibiotic-loaded cemented implant can eradicate the infection and dual mobility cup with modular-neck stem can strongly limit the risk of further dislocation.
Another important point is that the patient had already suffered previous surgeries and was classified as ASA IV with presence and history of several comorbidities; he underwent a one-stage exchange (explant and revision) of the prosthesis to prevent or limit the risk of perioperative general complications. At a short follow-up period, our option has shown to be a winning strategy.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Sat 04, Apr 2020Accepted: Mon 20, Apr 2020
Published: Fri 24, Apr 2020
Copyright
© 2023 Giuseppe Solarino. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.04.07
Author Info
Antonio Virgilio Biagio Moretti Francesco Maruccia Giuseppe Solarino Vito Belviso
Corresponding Author
Giuseppe SolarinoDepartment of Basic Medical Sciences, Neuroscience and Sense Organs, Orthopaedics and Traumatology Unit, University of Bari "Aldo Moro", Bari, Italy
Figures & Tables

References
- Rodriguez Buitrago A, Attum B, Cereijo C, Yusi K, Jahangir AA et al. (2019) Hemiarthroplasty for Femoral Neck Fracture. JBJS Essent Surg Tech 9: e13. [Crossref]
- Hauer G, Heri A, Klim S, Puchwein P, Leithner A et al. (2020) Survival Rate and Application Number of Total Hip Arthroplasty in Patients With Femoral Neck Fracture: An Analysis of Clinical Studies and National Arthroplasty Registers. J Arthroplasty 35: 1014-1022. [Crossref]
- Solarino G, Abate A, Vicenti G, Spinarelli A, Piazzolla A et al. (2016) Reducing periprosthetic joint infection: what really counts? Joints 3: 208-214. [Crossref]
- Izakovicova P, Borens O, Trampuz A (2019) Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev 4: 482-494. [Crossref]
- Kizkapan TB, Misir A, Uzun E, Oguzkaya S, Ozcamdalli M (2020) Factors affecting dislocation after bipolar hemiarthroplasty in patients with femoral neck fracture. Injury 51: 663-669. [Crossref]
- Okike K, Chan PH, Prentice HA, Paxton EW2 Burri RA (2020) Association Between Uncemented vs Cemented Hemiarthroplasty and Revision Surgery Among Patients With Hip Fracture. JAMA 323: 1077-1084. [Crossref]
- Lin FF, Chen YF, Chen B, Lin CH, Zheng K (2019) Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: A meta-analysis of randomized controlled trails. Medicine (Baltimore) 98: e14634. [Crossref]
- Zheng H, Gu H, Shao H, Huang Y, Yang D et al. (2020) Treatment and outcomes of Vancouver type B periprosthetic femoral fractures. Bone Joint J 102-B: 293-300. [Crossref]
- Stoffel K, Blauth M, Joeris A, Blumenthal A, Rometsch E (2020) Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: a systematic review. Arch Orthop Trauma Surg. [Crossref]
- van der Sijp MPL, van Delft D, Krijnen P, Niggebrugge AHP, Schipper IB (2018) Surgical Approaches and Hemiarthroplasty Outcomes for Femoral Neck Fractures: A Meta-Analysis. J Arthroplasty 33: 1617-1627. [Crossref]
- Gill JR, Kiliyanpilakkill B, Parker MJ (2018) Management and outcome of the dislocated hip hemiarthroplasty. Bone Joint J 100-B: 1618-1625. [Crossref]
- Vicenti G, Solarino G, Spinarelli A, Carrozzo M, Picca G et al. (2016) Restoring the femoral offset prevent early migration of the stem in total hip arthroplasty: an EBRA-FCA study. J Biol Regul Homeost Agents 30: 207-212. [Crossref]
- Balato G, Ascione T, Rosa D, Pagliano P, Solarino G et al. (2015) Release of gentamicin from cement spacers in two-stage procedures for hip and knee prosthetic infection: an in vivo pharmacokinetic study with clinical follow-up. J Biol Regul Homeost Agents 29: 63-72. [Crossref]
- Aggarwal VK, Rasouli MR, Parvizi J (2013) Periprosthetic joint infection: Current concept. Indian J Orthop 47: 10-17. [Crossref]
