Journals
Hepatofugal Portal Venous Flow: From Normal to Pathological
A B S T R A C T
Whether segmental or diffuse, a hepatofugal blood flow is almost always pathological. Over the years, Doppler ultrasonography has retained its position as one of the most accessible and physiological imaging techniques to evaluate the direction of the portal blood flow. Detection of a reverse flow is important as it may change patient care and outcome.
Keywords
Liver, hepatofugal, hepatopetal, main portal vein
Introduction
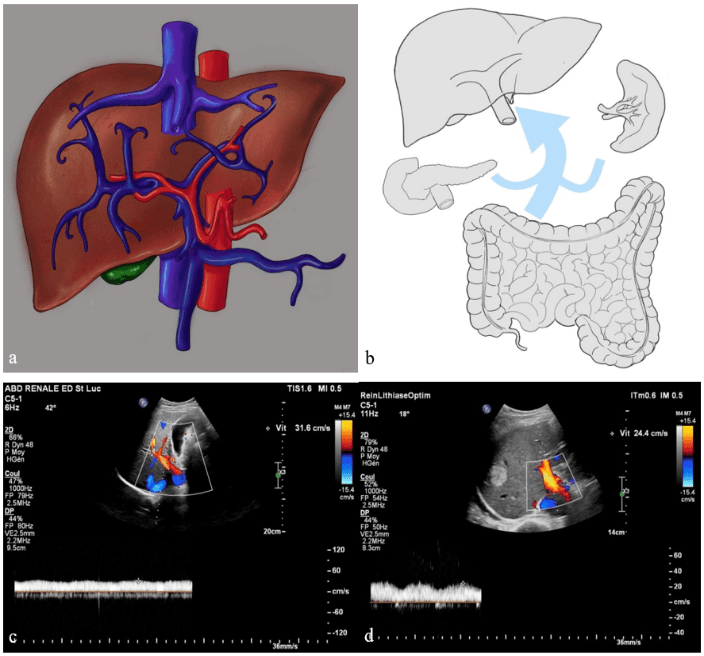
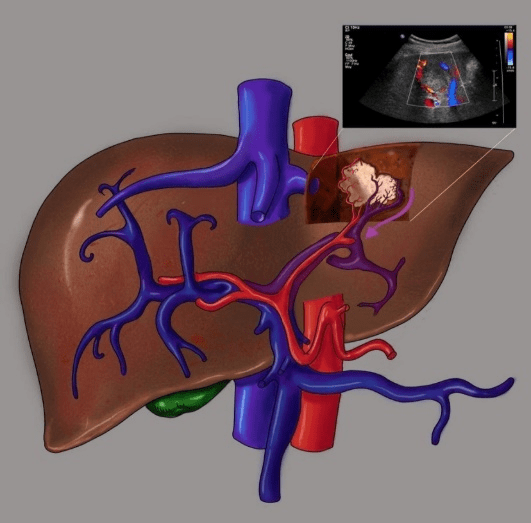
The liver is one of the most vascularized organs of the human body. It is estimated that 10-15% of the body’s total blood volume is contained in the liver. Its vasculature supply is dual with approximately 30% of arterial blood and 70% of venous blood. Although there are many variations, the arterial inflow (hepatic artery) usually arises from the coeliac trunk and provides oxygenated blood. The venous inflow (portal vein) supplies the liver with deoxygenated blood drained from the superior and inferior mesenteric veins, the splenic vein, the left gastric vein and the cystic vein (Figure 1a). The oxygenated and deoxygenated bloods mix in the hepatic sinusoids and then are drained into the hepatic veins and the inferior vena cava towards the outflow systemic circulation.
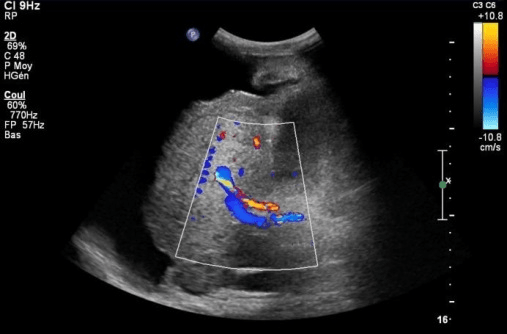
The term “hepatopetal” is used to describe a blood flow that is directed towards the liver whereas the term “hepatofugal” means that the blood flow is directed away from the liver. In the normal portal venous circulation, the blood flow is hepatopetal and is directed from the gastrointestinal tract, the spleen and the pancreas towards the liver (Figure 1b). With few exceptions, a hepatofugal flow in the portal venous system is always pathological. The direction of the blood flow is best demonstrated with the use of Doppler ultrasonography which is a fast, non-invasive and physiological evaluation. However, it can also be assessed by more invasive techniques such as angiography. A normal portal blood flow at Doppler ultrasonography is laminar (Figure 1c). Slight undulations linked to respiratory movements and heart beats are normal and frequently seen in younger patients (Figure 1d). The time average mean velocity ranges between 20 cm/s and 40 cm/s in the main portal vein (MPV). Detection of a hepatofugal portal flow is important as it has been shown to be associated with a poorer clinical outcome after liver transplantation and an overall decreased survival rate in cirrhotic patients.
I Normal hepatofugal flow
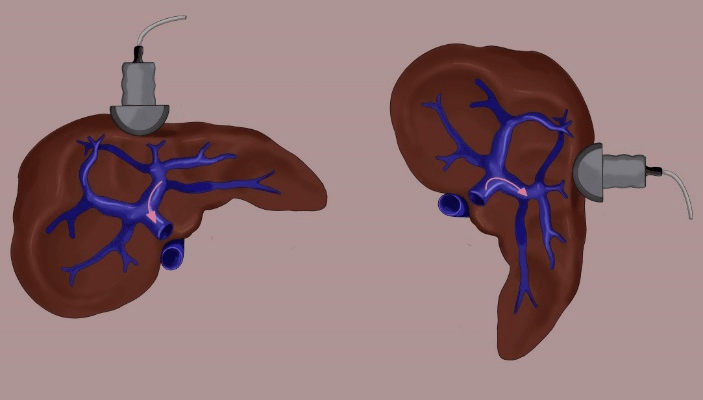
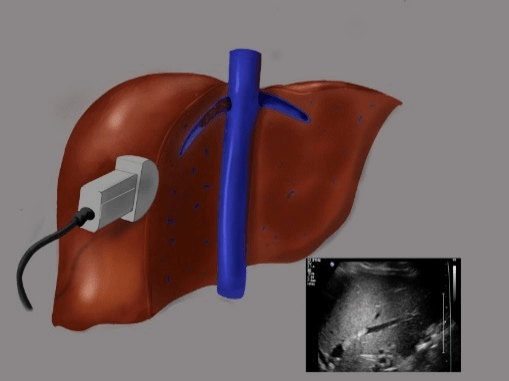
There are only a few rare situations in which a segmental reversed portal flow can be observed and considered normal. The first one is found when a liver transplant patient has received a large graft for its body size. In that situation, when the patient is in the dorsal decubitus position, a hepatofugal left portal vein can be observed on Doppler ultrasonography. When the patient is turned on his left side, the liver’s position shifts towards the center and the hemodynamics change. The left portal vein’s vascular resistance drops and the previously hepatofugal blood flow becomes hepatopetal (Figure 2).
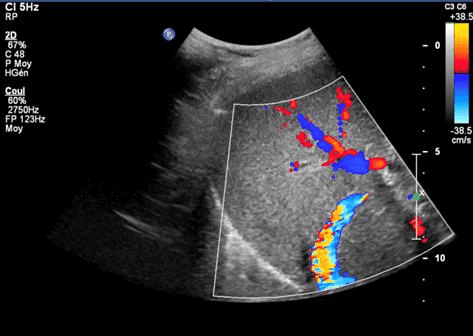
The second situation in which it is considered normal to find a segmental hepatofugal portal flow is in patients with a transjugular intrahepatic portosystemic shunt (TIPS). Furthermore, a hepatopetal flow has been shown to be highly predictive of a dysfunctional shunt especially if previous Doppler ultrasonography reported a hepatofugal flow. A TIPS’s purpose is to achieve portal decompression by bypassing the liver and its pathological high vascular resistance. Having created an alternative low resistance outflow path, the intrahepatic portal flow will be diverted, even if it means reversing, to find its way to the hepatic vein and the systemic circulation. On Doppler ultrasonography, you should expect to find a higher velocity in the MPV (> 40 cm/s), a peak systolic velocity > 50 cm/s in the TIPS and at least one hepatofugal main portal vein depending on the topography of the TIPS (figure 3).
Figure 1: Normal anatomy and Doppler ultrasound findings. a) figure of an anterior view of the arterial and venous vasculature supply of the liver, b) figure of the normal hepatopetal portal venous circulation, c) Doppler ultrasound image of a normal laminar hepatopetal main portal vein and d) Doppler ultrasound image of slight undulations linked to respiratory movements and heart beat in a young patient. Note the right lobe hyperechoic lesion (hemangioma).
Figure 2: Liver transplant patient. Inferior view of the liver with vascular resistance modifications from dorsal decubitus to left lateral decubitus.
II Pathological hepatofugal flow
As mentioned before, with few exceptions, a retrograde flow in the portal venous system is always pathological. We will describe the different causes of a hepatofugal flow by dividing them in two groups. The first group will describe focal or segmental inversion whilst the second group will discuss diffuse portal flow inversion.
Figure 3: TIPS. a) B mode ultrasound image, b) Doppler ultrasound image of a TIPS with segmental intra hepatic hepatofugal blood flow and aliasing artefact from the high velocity in the TIPS and c) normal peak systolic velocity >50 cm/s in the TIPS.
III Segmental portal inversion
Intra hepatic hepatofugal blood flow can be found in both the right and the left hepatic lobes. The focal change in blood flow direction is an indicator of a loco regional process affecting the liver’s vascular resistance.
IV Arterio-portal shunt
Arterio-portal shunts (APS) consist of an abnormal connection between a high pressure feeding artery and a low pressure draining vein. These shunts can be tumorous, for example in a hepatocarcinoma (Figure 4a) or a liver metastasis where they result from tumoral invasion or tumoral compression of the hepatic vein, or non-tumorous, for example after a trauma or a liver biopsy in a transplant patient.
Figure 4: Segmental portal inversion. a) figure and Doppler ultrasound image of a hepatocarcinoma in a cirrhotic liver with a hepatofugal draining vein, b) figure and B-mode ultrasound image of a hepatic vein thrombosis and c) Doppler ultrasound image in a case of Budd Chiari syndrome. Note the small size of the right liver, the hepatofugal main portal vein and the ascites.
V Liver transplant – hepatic vein thrombosis
Hepatic vein thrombosis is rare and only accounts for approximately 5% of vascular complications in liver transplant patients. Although rare, vein obstructions may arise in the postoperative period or as a delayed complication linked to scar tissue. This entity must be kept in mind whilst performing Doppler ultrasonography as it could, if left untreated, lead to graft failure (Figure 4b).
VI Budd Chiari Syndrome
In the Budd Chiari syndrome, the outflow obstruction is also related to the thrombosis of the hepatic veins or the terminal portion of the inferior vena cava [8]. These obstructions result either from a cruoric thrombus or a tumoral endovascular extension. The ultrasound findings depend on the number of veins involved and the rapidity of onset. When the obstruction is found in a single location, Doppler ultrasonography shows segmental portal vein inversion whereas when the obstruction is diffuse, the ultrasound shows signs of portal hypertension with a diffuse portal flow inversion (Figure 4c). In addition to a hepatofugal blood flow, Doppler ultrasonography can demonstrate the absence of blood flow in the hepatic veins, veno-venous hepatic shunts and hypertrophy of the caudate lobe and its draining vein (the only liver segment draining directly in the inferior vena cava).
VII Diffuse portal inversion
Diffuse hepatofugal blood flow is in an indicator of portal hypertension. The most frequent cause is liver cirrhosis but other etiologies such as congestive heart failure and acute liver failure can be responsible for the same ultrasound findings.
Figure 5: Diffuse portal inversion. a) Doppler ultrasound image of diffuse hepatofugal blood flow in end stage liver cirrhosis, b) figure of a cirrhotic liver, c) Doppler ultrasound image of mild congestive heart failure and b) Doppler ultrasound image of end stage congestive heart failure.
VIII Cirrhosis and portal hypertension
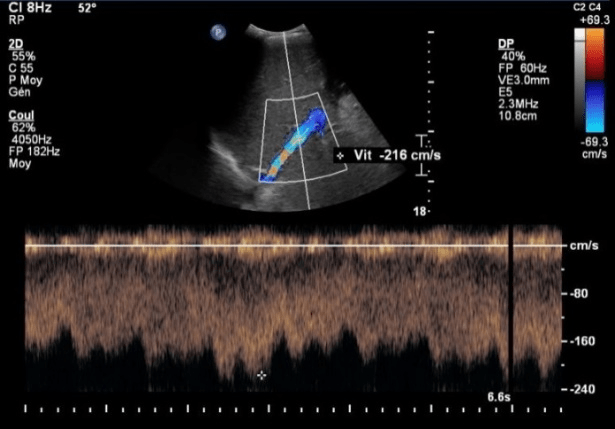
Non-forward portal flow in cirrhotic patients is a sign of advanced portal hypertension and advanced liver function impairment [1]. These patients have a significantly lower survival rate than those with a forward portal flow [4]. The mechanism can be explained with the alteration of the parenchyma, the development of fibrosis, the increase in the vascular hepatic resistance and the development of both small hepatic vein obstruction and diffuse arterio-portal shunts (Figure 5a, 5b) [1]. In the early stages of cirrhosis, the peak systolic velocity drops below 20 cm/s in the MPV. With time, and in correlation with the progression of the disease and the Child-Plug score, the velocity drops even further (< 10 cm/s) before sometimes becoming bidirectional and finally hepatofugal.
IX Congestive heart failure with tricuspid regurgitation
The mechanism in patients with heart failure is different. Indeed, in cirrhotic patients, the increase in vascular resistance is found within the liver. In patients with congestive heart failure, the increase in vascular resistance is situated on the outflow tract of the liver: the hepatic veins and the inferior vena cava. On Doppler ultrasonography, the portal blood flow shows undulations which come from the transmission of the heart beats (Figure 5c, 5d).
X Acute liver failure
Fulminant hepatic failure is characterized by an acute liver injury in the absence of an underlying chronic liver disease. There are many causes that can lead to acute liver failure and the diagnosis is not always evident. At real time Doppler ultrasonography, you may find a hepatofugal MPV, a decrease in liver echogenicity and a heterogeneous parenchyma.
XI Drug induced acute hepatitis
Drug induced acute hepatitis is caused by a toxic amount of a certain drug, toxin or supplement (vitamin, herbs). The diagnosis is essentially established on clinical history, drug use history and laboratory tests but physicians may want to exclude biliary obstruction and prescribe an ultrasound.
XII Liver transplant – acute cellular rejection
Acute cellular rejection is rare but remains an important cause of increased mortality in liver transplant patients [5]. The mechanism is complex with an important inflammatory infiltration along the portal tract as well as cholangitis and endothelitis (venulitis). Although the gold standard remains the liver biopsy, Doppler ultrasonography is useful for the differential diagnosis (vascular and biliary complications). In the case of acute cellular rejection, the periportal space is hyper echoic with a decreased velocity MPV or hepatofugal MPV. You may also notice hepatomegaly, an attenuation of the intrahepatic biliary ducts and an attenuation of the intra hepatic branches of the hepatic artery.
XIII Hepatic sinusoidal obstruction syndrome
Sinusoidal obstruction syndrome is characterized by a non-thrombotic occlusion of the terminal hepatic venules and the hepatic sinusoids. The luminal narrowing, caused by endothelium cell injury and swelling, is responsible for an increase in vascular resistance and, thus, portal hypertension. The early manifestations on Doppler ultrasonography are a decreased velocity main portal vein, hepatomegaly, thickening of the gallbladder wall, a rapid increase in spleen size and ascites. With time, and in correlation with the severity of the disease, Doppler ultrasonography may show portal flow inversion.
Conclusion
In line with recent studies and the better understanding of the liver’s complex vasculature, Doppler ultrasonography remains one of the most accessible and physiological imaging techniques to evaluate the venous portal system. With few exceptions, a hepatofugal blood flow, whether segmental or diffuse, is always pathological and its detection is important as it plays an important role in patient care and outcome.
Conflicts of interest
All authors agree for publication and report no conflict of interest.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 02, Aug 2019Accepted: Wed 21, Aug 2019
Published: Sat 31, Aug 2019
Copyright
© 2023 Margaux Collard. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2019.03.10
Author Info
Anca Dragean Emmanuel Coche Margaux Collard Marin Halut
Corresponding Author
Margaux CollardDepartment of Imaging, St Luc Univeristy Hospital, Avenue Hippocrate 10, 1200 Brussels, Belgium
Figures & Tables


References
- Elsayes KM, Shaaban AM, Rothan SM, Javadi S, Madrazo BL et al. (2017) A comprehensive approach to hepatic vascular disease. RadioGraphics 37: 813-836. [Crossref]
- Tarantino L, Giorgio A, de Stefano G, Mariniello N, Perrotta A et al. (1997) Reverse flow in intrahepatic portal vessels and liver function impairement in cirrhosis. Eur J Ultrasound 6: 171-177. [Crossref]
- Wachsberg RH, Bahramipour P, Sofocleous CT, Barone A (2002) Hepatofugal flow in the portal venous system: pathophysiology, imaging findings, and diagnostic pitfalls. RadioGraphics 22: 123-140. [Crossref]
- Jeong WK, Kim KW, Lee SJ, Shin YM, Kim J et al. Hepatofugal portal venous flow on doppler sonography after liver transplantation. J Ultrasound Med 31: 1069-1079. [Crossref]
- Kondo T, Maruyama H, Sekimoto T, Shimada T, Takahashi M et al. (2015) Reversed portal flow: clinical influence on the long-term outcomes in cirrhosis. World J Gastrqoenterol 21: 8894-8902. [Crossref]
- Levitsky J, Goldberg D, Smith AR, Mansfield SA, Gillespie BW et al. (2017) Acute Rejection Increases Risk of Graft Failure and Death in Recent Liver Transplant Recipients. Clin Gastroenterol Hepatol 15: 584-593. [Crossref]
- Copelan A, Kapoor B, Sand M (2014) Transjugular intrahepatic portosystemic shunt: indications, contraindications, and patient work-up. Semin Intervent Radiol 31: 235-242. [Crossref]
- Plessier A, Valla DC (2008) Budd-Chiari Syndrome. Semin Liver Dis 28: 259-269. [Crossref]
- Wells ML, Fenstad ER, Poterucha JT, Hough DM, Young PM et al. (2016) Imaging findings of congestive hepatopathy. RadioGraphics 36: 1024-1037. [Crossref]
- Michael L. Wells, Eric R. Fenstad, Joseph T. Poterucha, David M. Hough, Phillip M. Young, Philip A. Araoz, Richard L. Ehman, Sudhakar K. Venkatesh. Imaging findings of congestive hepatopathy. RadioGraphics 36: 1024-1037. [Crossref]
