Hydrocephalus Associated with Brain Tumor: Characteristics, Management & Outcomes in a Regional Neurosurgical Centre in Nigeria
A B S T R A C T
Introduction: Brain tumor is a common neurosurgical condition encountered by neurosurgeons in clinical practice. Hydrocephalus could be associated with brain tumor thereby increasing the burden of the disease to the affected patients. Characteristics and outcome of hydrocephalus resulting from brain tumors are almost unknown in our setting. The objectives of this study were to describe the characteristics and outcome of hydrocephalus caused by brain tumor in our center.
Methods: A retrospective analysis of all cases of hydrocephalus resulting from brain tumor managed in our center between January 2015 to December 2019. Relevant data extracted from patient’s case files and operation register was analysed.
Results: Out of the total sixty-eight cases of brain tumors, thirty (44.1%) cases of hydrocephalus caused by brain tumor were managed over the study period. The mean age of presentation was 14 years ± 2 SD with a slight male preponderance (M: F = 1.07:1). The most common clinical presentations were headache, progressive visual impairment, altered conscious level and ataxia. Posterior fossa tumors were the commonest (21/30), followed by craniopharyngioma (6/30) and one case each for pituitary macroadenoma, pineal region tumor and choroid plexus papilloma respectively. Pediatric age group was the most affected (19/30). All patients had ventriculoperitoneal shunting before definitive surgery. Postoperative outcome was good in the majority of cases (27/30), mortality was recorded in one patient (1/30).
Conclusion: Hydrocephalus is a common association in patients with brain tumor in our center. Most cases of brain tumor associated hydrocephalus occur in children and posterior fossa tumor is the commonest aetiology. The outcome of ventriculoperitoneal shunting is relatively good in our setting.
Keywords
Hydrocephalus, brain tumors, ventriculoperitoneal shunt
Introduction
Hydrocephalus is a relatively common association in patients with brain tumor. Tumor-associated hydrocephalus is seen in about half of cases of pediatric brain tumors depicting its preference for children [1]. Brain tumor-associated hydrocephalus may occur due to many factors such as obstruction, overproduction of cerebrospinal fluid (CSF) or both [2]. Obstructive hydrocephalus occurs when there is blockage along the pathway of cerebrospinal fluid circulation by the tumor or proteinaceous materials secreted by the tumor. Overproduction of CSF by tumors could also leads to hydrocephalus as a result of imbalance between production and absorption of CSF. The presence of hydrocephalus increases the morbidity and possibly mortality in some cases. Hydrocephalus leads to an increase intracranial pressure in addition to the symptoms and signs of the brain tumor. Majority of patients with brain tumor-related hydrocephalus in developing countries/regions do report late to the hospital, mostly in acute situations requiring emergency treatments [3]. The optimal timing and type of treatment of hydrocephalus associated with brain tumor is controversial [4-6].
Some authors advocate pre-craniotomy ventriculoperitoneal shunt or endoscopic third ventriculostomy or external ventricular drain and subsequent craniotomy and excision of brain tumor, while others prefer initial tumor excision and subsequent treatment of hydrocephalus when it persists [4, 5, 7]. However, treatment of hydrocephalus associated with brain tumor should depend on acuity of presentation, availability of neurosurgical facilities and the skills of the surgeon. In our setting where patients present late with raised intracranial pressure, paucity of resources and long-waiting lists, ventriculoperitoneal (VP) shunt is preferred because shunts are available and effective in relieving the deadly intracranial hypertension while waiting to have a stable patient that can withstand major craniotomy and tumor excision. Little or no attention is given to hydrocephalus associated with brain tumor especially in developing countries.
Objectives
The objectives of this paper were to determine the characteristics and management outcomes of hydrocephalus associated with brain tumor seen in our center.
Materials and Methods
A retrospective analysis of all cases of hydrocephalus resulting from brain tumor managed in our center between January 2015 to December 2019. Relevant data such as bio-demographics, clinical characteristics and management outcomes extracted from patients’ case files and operation register were analysed.
Results
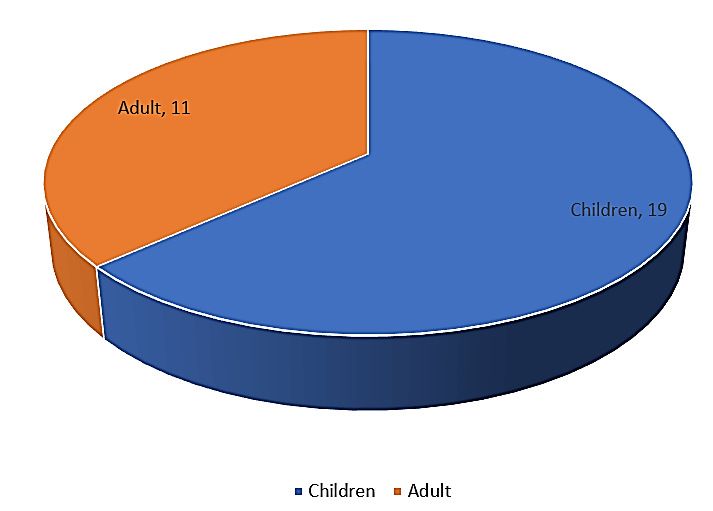
Out of the total sixty-eight cases of brain tumors, thirty (44.1%) cases of hydrocephalus caused by brain tumor were managed over the study period. The mean age of presentation was 14 years ± 2 SD with a slight male preponderance (M: F= 1.07:1). The most common clinical presentations were headache, progressive visual impairment, altered conscious level and ataxia. Posterior fossa tumors were the commonest (21/30), followed by craniopharyngioma (6/30) and one case each for pituitary macroadenoma, pineal region tumor, and choroid plexus papilloma respectively. Pediatric age group was the most affected (19/30) (Figure 1).
Figure 1: Age distribution of the patients.
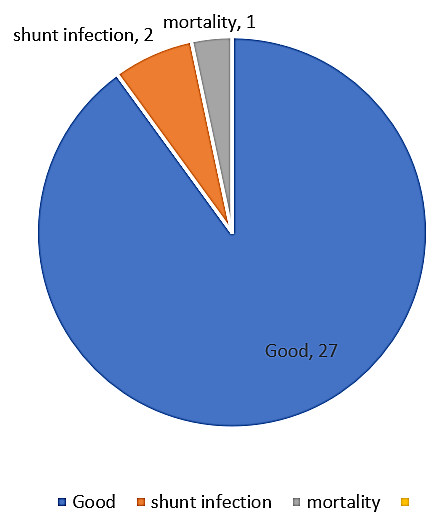
All patients had ventriculoperitoneal shunting before definitive surgery. Postoperative outcome was good (clinical improvement with no complication related to the VP shunt) in the majority of cases (27/30), mortality was recorded in one patient (1/30) (Figure 2).
Figure 2: Post VP shunt outcome.
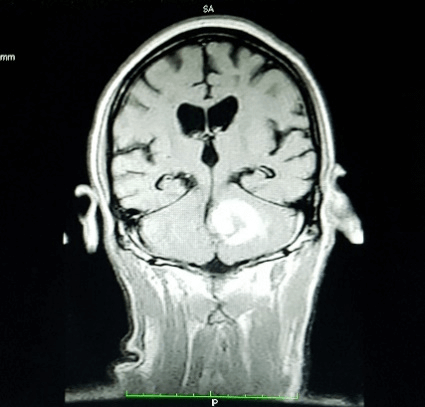
Figure 3: MRI coronal view showing left cerebellar hemispheric tumor obstructing 4th ventricular outflow and hydrocephalus.
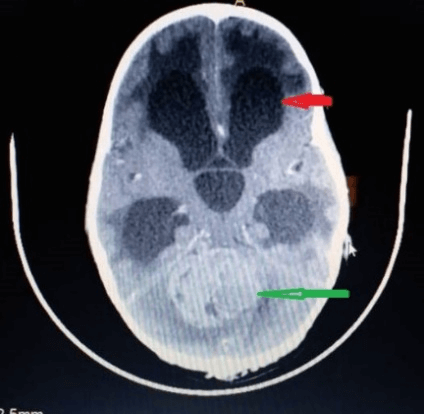
Figure 4: Axial view CT scan showing midline cerebellar tumor (green arrow) with hydrocephalus (red arrow).
Discussion
Hydrocephalus occurring in patients with brain tumor has been termed as tumoral hydrocephalus or brain tumor-associated/related hydrocephalus. It’s a common condition in brain tumors especially in posterior fossa tumors. This poses great challenge to neurosurgeons adding significantly to morbidity and the cost of management. Tumoral hydrocephalus has been reported to occur after resection of posterior fossa tumor in 10-36% of cases [6, 8-10]. In our study, hydrocephalus was observed in 44.1% of all cases of brain tumors managed. Children have higher incidence of 63.3% in the present study which was in tandem with the reports of other studies [1, 11]. Some authors found a higher occurrence of about 70-90% in their studies [5, 12-14]. However, a study in Senegal, a west African country found tumoral hydrocephalus in 25% of their series [3]. The reasons for the observed variance of incidence of tumoral hydrocephalus may be from differences in study design and geographical location. We found a slight male predominance similar to the findings of other studies in literature [15, 16]. An index study shows that tumoral hydrocephalus is common in children aged fourteen years old. In contrast, a different study conducted elsewhere in west African sub-region reported it often occurrence amongst mean age of 35 years [3].
All the patients presented with features of raised intracranial pressure in the present study. Late presentation is a norm in our settings because of cultural beliefs about neurological conditions mostly being attributed to spiritual attacks, in addition to few neurosurgeons handling millions of patients, concentration of neurosurgeons to urban areas, high rates of poverty and insufficient health insurance and poor transport infrastructures precluding early neurosurgical visitation. The commonest cause (70%) of tumoral hydrocephalus was posterior fossa tumors. Similar findings were noted in previous studies [3, 17]. While the second common cause was craniopharyngioma. Craniopharyngioma is a relatively common tumor in Nigeria compared to other part of the world [18]. Different modalities for tumoral hydrocephalus have been described depending on the clinical status of the patients, available facilities and the skills of the surgeon. Some scholars suggest initial ventriculoperitoneal shunting or external ventricular drain or endoscopic third ventriculostomy prior to definitive tumor excision [19, 20]. This is to abate intracranial hypertension and possibly reduce operative mortality [21].
Possible risks of the aforementioned approach include delaying definitive surgery, occurrence of shunt metastasis in in malignant tumor, upward trans-tentorial herniation, placing shunts in patients who may not require it permanently and shunts may become infected before definitive tumor excision [15]. ventriculoperitoneal is being considered by some neurosurgeons as the most desirable treatment measure in tumoral hydrocephalus [4]. In our setting, we opted for initial ventriculoperitoneal shunts before definitive surgery because our patients presented late with marked intracranial hypertension requiring emergency surgery. This approach allows patients to become stable enough to withstand definitive craniotomy and tumor excision. Non-functioning equipment for endoscopic third ventriculostomy prevented the procedure. We had two cases of shunt infection developing before definitive surgery and one mortality was recorded.
Conclusion
Hydrocephalus is a common association in patients with brain tumor in our center. Most cases of brain tumor associated hydrocephalus occur in children and posterior fossa tumor is the commonest aetiology. The outcome of ventriculoperitoneal shunting is relatively good in our setting.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 17, Nov 2020Accepted: Thu 17, Dec 2020
Published: Tue 22, Dec 2020
Copyright
© 2023 Aliyu Muhammad Koko. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2020.06.03
Author Info
Aliyu Muhammad Koko Nasiru Jinjiri Ismail Lasseini Ali Bello Bala Shehu
Corresponding Author
Aliyu Muhammad KokoDepartment of neurosurgery, regional centre for neurosurgery Usmanu Danfodiyo University Teaching Hospital Sokoto, Nigeria
Figures & Tables
References
- Wong TT, Liang ML, Chen HH, Chang FC (2011) Hydrocephalus with brain tumors in children. Childs Nerv Syst 27: 1723-1734. [Crossref]
- Roth J, Constantini S (2019) Hydrocephalus and Brain Tumors. Limbrick DD, Leonard JR eds. (2019) Cerebrospinal Fluid Disorders. Springer Nature Switzerland AG 199-217.
- Thiam AB, Mbaye M, Gerald R, Kala B, Thioub M et al. (2020) Management of Hydrocephalus in Brain Tumors to Fann Teaching Hospital in Dakar. Int J Neurosurg 4: 1-6.
- El Ghandour NMF (2011) Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in the treatment of obstructive hydrocephalus due to posterior fossa tumors in children. Childs Nerv Syst 27: 117-126. [Crossref]
- Rami AQ, Nidal K, Feras H, Muath A (2017) Neuroendoscopy Sway in the Treatment of Posterior Fossa Tumours associated Hydrocephalus in Children. J Neurol Stroke 6: 00203.
- Schijman E, Peter JC, Rekate HL, Sgouros S, Wong TT (2004) Management of hydrocephalus in posterior fossa tumors: How, what, when? Childs Nerv Syst 20: 192-194. [Crossref]
- Lee M, Wisoff JH, Abbott R, Freed D, Epstein FJ (1994) Management of hydrocephalus in children with medulloblastomas: prognostic factors for shunting. Pediatr Neurosurg 20: 240-247. [Crossref]
- Goel A (1993) Whither preoperative shunts for posterior fossa tumours? Br J Neurosurg 7: 395-399. [Crossref]
- Culley DJ, Berger MS, Shaw D, Geyer R (1994) An analysis of factors determining the need for ventriculoperitoneal shunts after posterior fossa tumor surgery in children. Neurosurgery 34: 402-407. [Crossref]
- Due Tønnessen BJ, Helseth E (2007) Management of hydrocephalus in children with posterior fossa tumors: Role of tumor surgery. Pediatr Neurosurg 43: 92-96. [Crossref]
- Sherrod BA, Iyer RR, Kestle JRW (2020) Endoscopic third ventriculostomy for pediatric tumor-associated hydrocephalus. Neurosurg Focus 48: E5. [Crossref]
- Beltagy MA El (2018) Hydrocephalus Associated to Tumors. Di Rocco C et al. (2018) Textbook of Pediatric Neurosurgery. Springer International Publishing AG 1-13.
- Lam S, Reddy GD, Lin Y, Jea A (2015) Management of hydrocephalus in children with posterior fossa tumors. Surg Neurol Int 6: S346-S348. [Crossref]
- Foreman P, McClugage S III, Naftel R, Griessenauer CJ, Ditty BJ et al. (2013) Validation and modification of a predictive model of postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 12: 220-226. [Crossref]
- M Mbaye, M Thioub, AB Thiam, CN Sy, R G Boukaka et al. (2017) Treatment of tumor hydrocephalia by endoscopic ventriculo-cisternostomy. J Afr Chirurgie 4: 131-136.
- Roux A, Botella C, Still M, Zanello M, Dhermain F et al. (2018) Posterior Fossa Metastasis-Associated Obstructive Hydrocephalus in Adult Patients: Literature Review and Practical Considerations from the Neuro-Oncology Club of the French Society of Neurosurgery. World Neurosurg 117: 271-279. [Crossref]
- Raimondi AJ, Tomita T (1981) Hydrocephalus and infratentorial tumors Incidence, clinical picture, and treatment. J Neurosurg 55: 174-182. [Crossref]
- Richard E, Saleem A, Laligam NS (2012) Principles of Neurological surgery, Third edition. Elsevier Saunders 598.
- Khasawneh N, Bani Mustafa H, Abu Wandi E (2008) Endoscopic Third Ventriculostomy in the Treatment of Hydrocephalus Secondary to Posterior Fossa Tumours In Children. JRMS 15: 47-51.
- Bognar L, Borgulya G, Benke P, Madarassy G (2003) Analysis of CSF shunting procedures requirement in children with posterior fossa tumors. Childs Nerv Syst 19: 332-336. [Crossref]
- Greenberg MS (2010) Handbook of Neurosurgery, Seventh Edition. Thieme Medical Publishers 590.
