Improved Apical Margins with Use of Periurethral Suspension Stitch in Robotic Assisted Radical Prostatectomy
A B S T R A C T
Introduction: Robotic surgery has transformed the standard treatment for localized prostate cancer. Oncologic control is at the foremost concern when treating prostate cancer. Previous studies have detailed the use of a periurethral suspension stitch during robotic assisted radical prostatectomy (RARP), but none have demonstrated significant improvement in surgical margins.
Objective: The purpose of this study is to illustrate the use of a periurethral suspension stitch during RARP and its impact on apical surgical margin status.
Methods: This study retrospectively analysed 97 patients who underwent RARP by a single high-volume robotic surgeon (TJM) between November 2011 and February 2014. The patients were split into two cohorts with one group (Suspended Stitch) having the dorsal venous complex (DVC) ligation stitch suspended while the second group having the DVC ligation stitch unsuspended (Unsuspended Stitch).
Results: Positive margins were seen in 39.6% of patients in the Unsuspended Stitch group and 20.4% of patients in the Suspended Stitch group (p=0.04). Patients in the Unsuspended Stitch group had a Gleason score > 7 in 33.3% of cases, where patients in the Suspended Stitch group had a Gleason score > 7 in 57.1% of cases.
Conclusion: Localized prostate cancer treatment has significantly changed with RARP. This study provides an additional technique for achieving improved oncologic control.
Keywords
Robotics, prostate cancer
Introduction
With the advent of robotics in urology, robotic assisted radical prostatectomy (RARP) has quickly become the standard treatment for localized prostate cancer [1, 2]. The robotic platform has allowed for numerous benefits related to blood loss, time to convalescence and visualization of the surrounding neurovasculature [3]. The central dogma with respect to the treatment of prostate cancer, in order of importance, is oncological control, preservation of urinary continence, and lastly the maintenance of sexual function. The use of a periurethral suspension stitch during RARP has been advocated in prior series as a method of significantly improving short-term recovery of urinary continence, as well as offering a short-term quality of life and sexual function advantage in this patient population [4, 5]. To our knowledge, no studies have shown a significant improvement in margin rates with the use of periurethral suspension stitch.
Walsh originally described this method of urethral suspension in open radical retropubic prostatectomy series, with Patel being the first to describe it being performed robotically [4]. A suture is passed through the dorsal venous complex (DVC) and then the perichondrium of the pubic symphysis. This technique essentially suspends the urethral stump and reestablishes the function of the ligated puboprostatic ligaments once tied in place. In our recent experience, it was postulated that the stitch may additionally aid in the apical dissection and result in an improvement in apical margin status. In an effort to further refine robotic surgical technique, we report our institutional experience with the use of a periurethral suspension stitch during RARP and its impact on apical surgical margin status.
Methods
This study analysed 97 patients who underwent RARP by a single high-volume robotic surgeon (TJM) between November 2011 and February 2014. The surgeon had extensive robotic surgical experience with more than 500 RARP’s prior to the initiation of the database. Data was retrospectively analysed from a prospectively maintained database. Institutional review board approval was obtained for all collected data, with all patients providing written informed consent within a prospectively maintained database. All patients analysed underwent standard pre-operative evaluation for their prostate cancer, which included complete history and physical exam, digital rectal exam, serum PSA, transrectal ultrasound of the prostate with biopsies and additional advanced imaging, when indicated. Patients without clinical evidence of extra-prostatic invasion or distant metastasis were provided with the option of RARP for initial definitive therapy. Patient demographics included age, BMI, estimated blood loss (EBL), length of operation, length of stay (LOS), Gleason Score, final pathological stage, and complications.
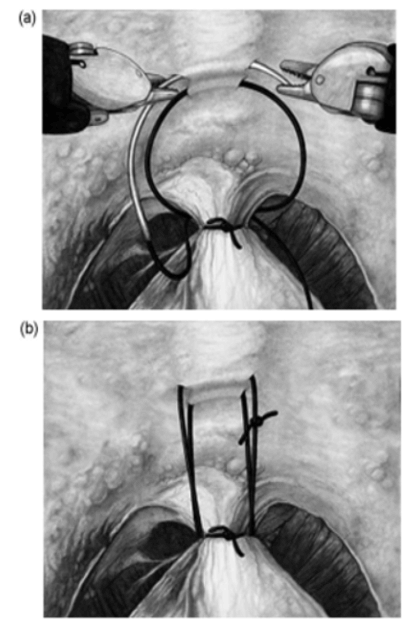
Throughout the study period, all RARP’s started with a posterior approach, followed by dropping the bladder, and exposing the space of Retzius. After bladder neck transection and subsequent ligation of the prostatic pedicles, a DVC stitch was placed on the prostate. The technique used for the periurethral stitch was described by Patel, et al., and is depicted in (Figures 1 & 2). We began performing the periurethral suspension stitch on December 4, 2012. Prior to this date, the DVC was ligated with a single interrupted stitch and did not include periurethral suspension. The Unsuspended Stitch group included men that underwent RARP without a suspension stitch from November 2011 to December 2012. The Suspended Stitch group included RARP from July 2012 to February 2014. We did not include the initial six months of patient data to avoid the confounding factor of physician learning curve with respect to the suspension stitch. Prostate specimens were processed according to standard pathological methods and classified according to the American Joint Committee on Cancer TNM classification system. Additional information was reported by the pathology department with respect to location of positive margins. The two cohorts were then analysed with respect to their surgical margin status with attention paid to location.
Statistical analysis included suitable cases from chart review, scrutinized at the case level and patients with missing data were excluded from analyses. The two groups were statistically compared with the primary end points of positive surgical margin and positive apical surgical margin. Secondary end points included age, BMI, estimated blood loss, length of operation, length of stay, final Gleason score, final pathological stage, and complications. Chi-square test of the Fisher exact test was used to compare categorical variables. Continuous variables were compared using Wilcox-Mann-Whitney test. Analysis was performed using SAS® Proprietary Software version 9.4 and standard statistical significance was defined as p<0.05.
Figure 1: Periurethral suspension stitch. Patel et al. [4].
Figure 2: Surgical demonstration of suspension stitch.
Results
A total of 97 patients were included in the study and split into two cohorts, the Unsuspended Stitch group (n=48) and the Suspended Stitch group (n=49). The mean age was 64.7 and 62 years, for the Unsuspended and Suspended groups, respectively. The mean BMI was 29.1 and 29.4, for the Unsuspended and Suspended groups, respectively. There were not clinically or statistically significant differences between the two cohorts with respect to EBL, length of operation, length of stay or overall complications (Table 1).
Table 1: Demographics/Perioperative Data.
|
|
Unsuspended Stitch (n=48) |
Suspended Stitch (n=49) |
p-value |
|
Age (years) |
64.7 |
62 |
|
|
BMI |
29.1 |
29.4 |
|
|
EBL (mL) |
172.3 |
223.4 |
0.33 |
|
Length of Operation (minutes) |
125.1 |
131.8 |
0.61 |
|
Length of Stay (Days) |
1.6 |
1.3 |
0.36 |
There was a statistically significant difference found between the two groups with respect to Gleason Score (Table 2). Patients in the Unsuspended Stitch group had a Gleason score > 7 in 33.3% of cases, where patients in the Suspended Stitch group had a Gleason score > 7 in 57.1% of cases. There was no significant difference in final pathological stage for each cohort. Overall positive margins were seen in 39.6% of patients in the Unsuspended Stitch group and 20.4% of patients in the Suspended Stitch group (p=0.04). When specifically analysing apical positive margins, 12 patients had a positive apical margin in the Unsuspended Stitch group versus 2 patients in the Suspended Stitch group (p <0.05).
Table 2: Pathologic Outcomes.
|
|
Unsuspended Stitch (n=48) |
Suspended Stitch (n=49) |
p-value |
|
Gleason Score 6 7 8+ |
32 (66.7%) 14 (27.1%) 3 (6.2%) |
21 (42.9%) 25 (51.1%) 3 (6%) |
0.01 |
|
Pathology Stage T0 T2 T3 |
1 (2.1%) 38 (79.2%) 9 (18.8%) |
0 (0) 43 (87.7%) 6 (12.2%) |
0.33 |
|
Surgical Positive Margin Yes No |
19 (39.6%) 29 (60.4%) |
10 (20.4%) 39 (79.6%) |
0.04 |
|
Apical Positive Margin Yes No |
12 (25%) 36 (75%) |
2 (4.1%) 47 (95.9%) |
0.05 |
Discussion
To our knowledge, this is the first study to demonstrate a significant improvement of both surgical and apical margin status in RARP while utilizing the periurethral suspension stitch. In addition to achieving better oncological margins with the periurethral suspension stitch, the Suspended Stitch group had statically significant higher Gleason scores compared to the Unsuspended Stitch group. Although our study demonstrated noteworthy changes in our oncological outcomes by implementation of the periurethral suspension stitch, functional outcomes were not captured in these cohorts. Due to a combination of geographic distance and inability to remove biases associated with several different urologists assessing postoperative continence rates, short and long term follow up of these patients would have been difficult to record.
Patel and colleagues reported a significant statistical difference in the early recovery of continence at three months following RARP, with 92.8% compared to 83% return of continence in the cohort that received the periurethral suspension stitch. However, continence rates at six and 12 months were not significantly affected between those that did and did not receive the periurethral suspension stitch. The suspended stitch cohort had a higher positive surgical margin rate at 12.2% compared to 9.5% in the unsuspended stitch cohort, however, this was not statistically significant.
Johnson and colleagues also reported similar results in their experience with the periurethral suspension stitch demonstrating an improvement in continence at three months, but this difference in continence rates disappeared by six months postoperatively. Similarly to our study, Johnson et al. reported a lower percentages of positive surgical margin (13.79% v. 19.72%) and positive apical margin (4.60% v. 9.86%) in the anterior urethropexy stitch cohort versus those without the anterior urethropexy stitch, but both parameters did not reach statistical significance. In contrast to our study, neither of the previous studies showed statistically significant improvement in margin rates when the suspension stitch was employed. Patel et al. showed an insignificant increase in positive margin rates. Johnson et al. found a decrease in their margin rates when the stitch was used, but unfortunately failed to reach statistical significance. In our opinion, the stitch aids in the dissection of the apex by elevating the DVC away from the prostate. This allows for safer dissection of the apex while theoretically decreasing risk of hemorrhage from the DVC as well as allowing for better delineation of the urethral apical margin.
Limitations to this study can be directly linked to the pathological analysis. Our institution does not have a dedicated uropathology’s, allowing for some variation in how margin status is reported. Additionally, this study is unable to delineate focal margins and false-starts from true surgical margins. One way to potentially elucidate clinically significant oncological control is to follow these cohorts long-term with respect to biochemical recurrence rates. Further limitations of our study include its small cohorts and retrospective design. Finally, as stated above, many patients followed with outside urologists, which limited our ability to establish strict postoperative continence and erectile function criteria (i.e. number of pads used, quality of life).
Conclusion
Robotic surgery has significantly changed the landscape of prostate cancer surgery. This study adds to the evolution of RARP and provides additional techniques that assist with the most important aspect of prostate cancer treatment, oncological control. While our study was unable to elucidate functional outcomes, such as urinary incontinence and erectile function, this study is the first to demonstrate statistically significant lower rates of surgical positive margins utilizing a periurethral suspension stitch.
Funding
None.
Ethical Approval
This article is a retrospective study that does not require ethical approval.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 06, Mar 2021Accepted: Tue 16, Mar 2021
Published: Fri 09, Apr 2021
Copyright
© 2023 Kevin Keating. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2021.01.04
Author Info
Kevin Keating Matthew Rohloff Thomas J. Maatman
Corresponding Author
Kevin KeatingDepartment of Urological Surgery, Metro Health: University of Michigan Health, Michigan, USA
Figures & Tables
Table 1: Demographics/Perioperative Data.
|
|
Unsuspended Stitch (n=48) |
Suspended Stitch (n=49) |
p-value |
|
Age (years) |
64.7 |
62 |
|
|
BMI |
29.1 |
29.4 |
|
|
EBL (mL) |
172.3 |
223.4 |
0.33 |
|
Length of Operation (minutes) |
125.1 |
131.8 |
0.61 |
|
Length of Stay (Days) |
1.6 |
1.3 |
0.36 |
Table 2: Pathologic Outcomes.
|
|
Unsuspended Stitch (n=48) |
Suspended Stitch (n=49) |
p-value |
|
Gleason Score 6 7 8+ |
32 (66.7%) 14 (27.1%) 3 (6.2%) |
21 (42.9%) 25 (51.1%) 3 (6%) |
0.01 |
|
Pathology Stage T0 T2 T3 |
1 (2.1%) 38 (79.2%) 9 (18.8%) |
0 (0) 43 (87.7%) 6 (12.2%) |
0.33 |
|
Surgical Positive Margin Yes No |
19 (39.6%) 29 (60.4%) |
10 (20.4%) 39 (79.6%) |
0.04 |
|
Apical Positive Margin Yes No |
12 (25%) 36 (75%) |
2 (4.1%) 47 (95.9%) |
0.05 |

References
1. Pasticier G, Rietbergen JBW, Guillonneau B, Fromont G, Menon M et al. (2001) Robotically assisted laparoscopic radical prostatectomy: feasibility study in men. Eur Urol 40: 70-74. [Crossref]
2. Lowrance WT, Eastham JA, Savage C, Maschino AC, Laudone VP et al. (2012) Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. J Urol 187: 2087-2092. [Crossref]
3. Ploussard G (2018) Robotic surgery in urology: facts and reality. What are the real advantages of robotic approaches for prostate cancer patients? Curr Opin Urol 28: 153-158. [Crossref]
4. Patel VR, Coelho RF, Palmer KJ, Rocco B (2009) Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: description of the technique and continence outcomes. Eur Urol 56: 472-478. [Crossref]
5. Johnson EK, Hedgepeth RC, He C, Wood DP (2011) The impact of anterior urethropexy during robotic prostatectomy on urinary and sexual outcomes. J Endourol 25: 615-619. [Crossref]
