Instrument Separation Outside the Root Canal: Handling Methods and Difficulties
A B S T R A C T
In endodontics, fracturing of the instrument in the root canal can arise as an inevitable problem for the dentist, especially during the application of the metal-nickel-titanium devices to the root canal. What is more, the broken parts of the instruments may be beyond the point of the apex, which can produce a range of symptoms and cause additional physical and mental pain to the patients that must be relieved as fast as possible. A few cases are available, in which the separated endodontic instruments beyond the apex are addressed with surgical approaches, indicating that some cases can be resolved by surgical management. However, it is difficult to achieve the ideal results often due to bleeding, a lack of clinic experience, and an inability to accurately comprehend soft tissue activities. The best way, then, is to prevent the occurrence entirely if possible.
Keywords
Instrument separation, root canal therapy, periradicular surgery
Introduction
Root canal therapy (RCT) is the most commonly used treatment method for the management of pulpitis and periapical periodontitis. Metal instruments are widely used during this process; unfortunately, instrument separation occurs from time to time because of metal fatigue and improper use of root canal–enlarging needles and broaches. According to the literature, the probability of instrument separation is about 2.2% for teeth treatment and 1.1% in relation to the root canal. Generally, the length of separated instruments is about 3.07±1.46 mm, and mostly occurs in the first a third part of the root apex [1, 2]. There are many reports regarding the reasons and countermeasures of instrument separations in the root canal, and there are also mature treatment methods and techniques available for use in the clinic practice [1-6]. However, there are few reports on the subject of the instrument separations outside or beyond the root canal; hence not much discussion reported about the probability of its occurrence or about what should be done or not, when and how to be done once it happens, or about the complexity of handling these cases [6, 7]. In this report, this problem is deeply discussed through the presentation of 5 cases.
Typical Clinical Cases
Case 1
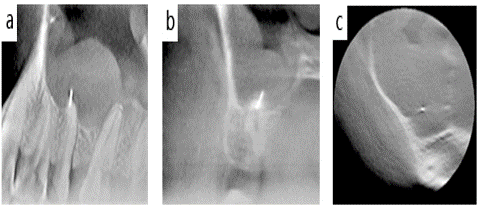
A male aged 18 years old came to see the doctor because of primary dental pain lasting for two days in the upper-right posterior tooth. It was found that deep caries had perforated into pulps in the mesio-occlusal surface of the no. 15 tooth, with heat application stimulating sharp pain but percussion provoking a painless response. The diagnosis was acute pulpitis, and root canal therapy was performed under local infiltration anaesthesia. However, in the process of therapy, 30# and 35# K-files were broken off in and outside the root canal. Additionally, cone-beam computed tomography (CBCT) revealed that the fractured needle outside the root canal was about 3 mm in length, perforating into the maxillary sinus (Figures 1, 2a & 2b).
Figure 1: The fractured needle perforated into the maxillary sinus.
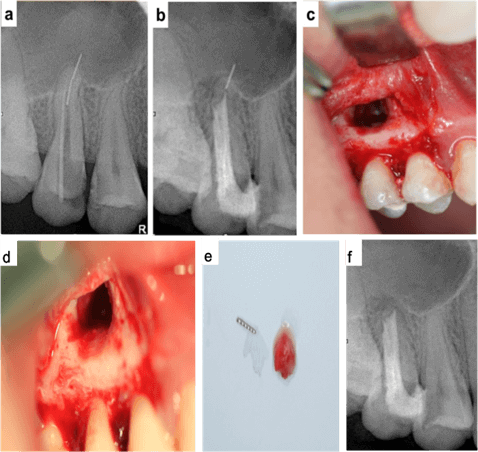
With the consent of the patient and his parents, the fractured needle located in the root canal was taken out using the ultrasonic vibration and oscillation method, and root canal filling and resin restoration were performed (Figures 2c & 2d). After two weeks, without contraindication of the local infiltrating anaesthesia, a full-thickness rectangular flap was established to open the mucoperiosteal flap (Figure 2c), revealing the apex area of the alveolar bone (Figure 2d). Here, approximately 2 mm of the root apex was removed (Figure 2e), the fractured needle was taken out (Figure 2e), and a root surface hole of about 3 mm was prepared (Figure 2d). Then, the operator filled in the root surface hole with a glass ionomer binding material (Japan Fuji Company, Tokyo, Japan). Once the surface of the wound was full of blood, the operator sutured the mucoperiosteal flap and filled in the wound with periodontal packing. The sutures were taken out one week later. No adverse effects were observed after three months of the surgery (Figure 2f).
Figure 2: Case 1 on the treatment of the fractured needle. a) The fractured needle located inside and outside of the root canal; b) After root canal filling; c) Opened flap, exposed bone and root apex following removal of 2 mm of the root apex; d) Gutta-percha in the apical foramen after removal of 2mm from the root apex; e) Fracture root apex and fractured needle; f) X-ray image taken at 3 months after surgery.
Case 2
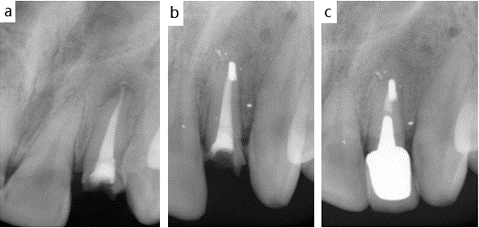
A female aged 23 years old came to see her doctor because of long-term pustules located in the gingiva under the right anterior tooth. She had experienced a traumatic injury six months ago, during that time, the upper-right anterior tooth crown was broken and, after receiving root canal therapy in another hospital, she contracted pustules in the gingiva lasting for about 4 months. An examination found that the mucosa sinus tract had discharged purulent secretions in the root apex of the no. 12 tooth, while no pain with percussion was reported. X-ray images showed that the root canal was overcharged, and the root apex outside of the root canal displayed a low-density shadow and a 1 mm high-density foreign body (Figure 3a). The patient was diagnosed with apicitis, overcharge, and foreign body outside the root apex. Considering that the root was about 14 mm with no loose, apical surgery and then post crown rehabilitation were conducted. Due to a lack of surgery contraindication, two incisions were made after local infiltration anaesthesia was established. One was a vertical incision in the far mid-axis and the other was an internal incision in the gingival sulcus. Then the operator opened the full-thickness mucoperiosteal flap (triangular flap), exposed the root apex area, took out the foreign body (broach needle), removed 1 mm of root apex, prepared a root surface hole of 3 mm and filled the hole with silver amalgam (Figure 3b). The granulation tissue of bone in the root apex area was thoroughly scraped and, after the root apex area was filled with blood, the tissue flap was sutured and filled with periodontal packing. All suturing was subsequently removed one week later. Post crown was repaired after two months and no abnormality was observed after three years (Figure 3c).
Figure 3: Case 2 on the treatment of the foreign body (broach needle). a) Overcharged and foreign body outside of the root canal; b) The root apex after surgery for 3 months; c) 3years after post crown restoration.
Case 3
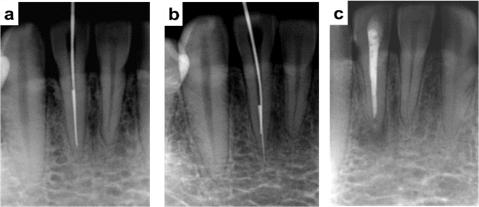
A male patient aged 32 years old was undergone root canal therapy due to the no. 42 acute apicitis caused by deep overbite-induced occlusal trauma of the anterior teeth. In the treatment, a 35# root canal reamer was observed to be broken and left in the apical area (Figure 4a). The root canal therapy was continued by a bypass. After the bypass was open, the broken reamer was pushed out of the root canal and further into the surrounding tissue during continuous enlargement (Figures 4a & 4b). However, the broken reamer was not removed by the repeated ultrasonic treatment. Therefore, root canal filling was then performed, and the broken reamer was ultimately removed by apical excision surgery through apical excision, apical hole preparation on the root surface, and retrograde apical filling (Figure 4c). The filling was conducted by using a glass ionomer (GC Company, Tokyo, Japan). Postoperative follow-up showed good healing.
Figure 4: Case 3 on the treatment of the broken root canal reamer. a) Root canal reamer was observed to be broken in the apical area; b) The broken reamer was pushed out of the root and further into the tissue; c) After retrograde apical filling treatment.
Case 4
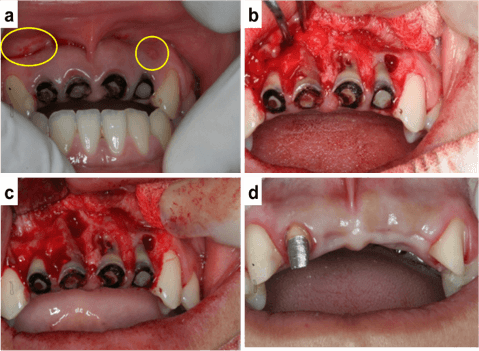
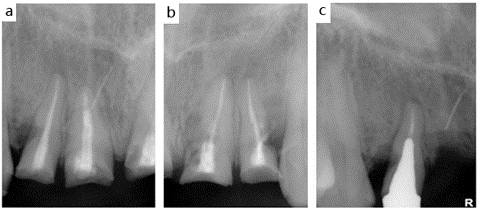
A female aged 25 years old was transferred to our hospital to undergo denture repair one year after being treated in another hospital. The examination showed that the no. 12, no. 11, no. 21 and no. 22 teeth had residual roots, while the no. 11, no. 21 and no. 22 tooth formed mucosal sinus tracts in the labial alveolar socket, with purulent secretions (highlighted in yellow circles in Figure 5a). The teeth were loose with a 0 to 1 degree and no pain with percussion. Labial periodontal bags were measured as 2 to 5 mm. The X-ray images showed that the roots were all overcharged; the no. 11, no. 21 and no. 22 tooth roots’ external absorption (lateral perforation) was very serious, and a metal foreign body had perforated the sidewall in mesio-occlusion of one-third of the no. 11 tooth root apex, which is about 4 mm (Figures 6a & 6b). The department of prosthodontics suggested restoring the crown after root canal therapy. However, X-ray images (Figure 6) indicated that the external absorption profile of the no. 11, no. 21 and no. 22 teeth (lateral perforation) was serious and no longer suitable for crown restoration. X-ray imaging results further showed that the fractured needle was located on the palatal side, affecting about one-third of the root apex of no. 11 tooth, located about 3 mm away from the labial alveolar bone (Figure 6a).
Figure 5: Case 4 on the treatment of the mucosal sinus tracts and residual roots. a) Residual roots and sinus tracts can be seen; b) The sidewall of the no. 11, no. 21 and no. 22 teeth had been perforated seriously (also indicating out-of-root absorption); c) No fractured needles were observed upon boning the no. 11 tooth root; d) Tooth abutments of the no. 12, no. 13 and no. 23 teeth checked three months after the surgery.
With the consent of the patient and the staff of the department of prosthodontics, and after confirmation that the patient has no contraindication of local infiltration anaesthesia, the operator then opened a rectangular full-thickness mucoperiosteal flap. After this, it could be seen that the sidewall of the no. 11, no. 21 and no. 22 teeth had been perforated seriously (also indicating out-of-root absorption) in a large area (Figures 5b & 5c). Furthermore, the fractured needle at the mesial side of the no. 11 tooth was not locatable when even boning up to 4 to 5 mm deep in the root areas (Figure 5c). Thus, there was a concern that the long-term outcome of post crown rehabilitation after sidewall repair would be ineffective. Again, with the consent of the patient and the staff of the department of prosthodontics, the no. 11, no. 21 and no. 22 teeth were decided to be removed. However, while removing the no. 11 tooth, no metal foreign body was taken out, so boning the alveolar bone layer by layer to locate the metal foreign body, according to the image information, was conducted.
Unfortunately, despite boning even to the mesial alveolar bone of the no. 11 tooth, the metal foreign body was still not located. As it was considered that there were no granulation tissues, and the damage of continuing with boning would be too much, the search for metal foreign bodies was abandoned. Then, the incision was closely sutured after the wound surface of the alveolar bone was full of blood. Suturing lines were removed after one week, and then restoration with a temporary concealed-denture apparatus was completed. No abnormalities were discovered upon rechecking the mucosa and alveolar bone three months later (Figure 5d). Also, the X-ray images showed that alveolar bone had healed well, with the fractured needle and alveolar bone fused together (Figure 6c). Hence, preparations for managing the no. 13, no. 12 and no. 23 teeth and plans to complete restorations with a fixed-denture apparatus.
Figure 6: The X-ray imaging of the fractured needles in Case 4. a) X-ray imaging of the no. 11 and no. 12 teeth before surgery; b) X-ray imaging of the no. 22 teeth before surgery; c) The X-ray image after surgery.
Case 5
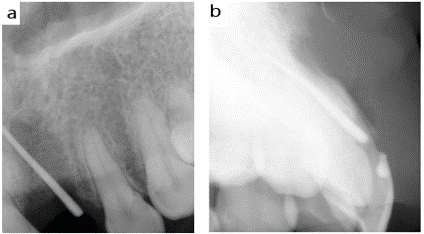
A female aged 54 years old came to our hospital because of suffering from facial pain for about three months after her upper-left incisor had been removed. The dull pain was firstly reported and became more and more serious when the facial muscle moved, beginning with the treatment of the upper-left incisor via root canal therapy in another hospital five months ago. Three months before coming to our hospital, the tooth was ultimately removed. However, the facial pain still persisted. An examination showed that the mucosa of the extracted no. 21 tooth was well-healed, and the height of the alveolar bone was normal. However, there was tenderness at the alveolar mucosa, and the pain became more serious when the area was rubbed. The X-ray images revealed that there was a high-density foreign body of about 2.5 mm (broach needle) in the root apex area of the no. 21 gingival groove (Figure 7a). The patient was informed that there was possibly a metal needle left in the soft tissue, and the needle location needs to be confirmed by performing an additional X-ray imaging scan.
With the patient's consent and no contraindications, the clinicians performed block anaesthesia on the left side of the canine fossa, inserted in the gutta-percha point in the direction of the root apex of the no. 21 tooth, and took 2 X-ray images according to parallel and lateral projection, respectively. The lateral X-ray imaging showed that the fractured needle was located in the mucosa of the no. 21 buccal alveolar socket (Figure7). After the approximate position was determined, the mucosa of the root apex of the no. 21 tooth was cut off in a longitudinal manner, and the needle was searched layer by layer. However, the fractured needle was not found even after repeatedly searching for 2 hours. The patient was suggested that the fractured needle could be located in the subperiosteal mucosa according to further X-ray imaging, and with the mucosa of the buccal alveolar socket in this region of about 1×1.5 cm2 large could be then completely cut off. Finally, a direct suturing would be performed. After consideration, the patient refused the above suggestion, so the interrupted suturing of the incision was performed instead. A week after surgery, a slight dull pain was reported when taking out stitches, and no further treatment was required.
Figure 7: Case 5 on the treatment of the broach needle in the mucosa of the root apex. a) Fractured needle at the no. 21 tooth root apex masked by the gutta-percha point; b) Lateral X-ray images shows the fractured needle located in the alveolar mucosa.
Discussion
According to the People's Republic of China State Council order no. 351, ‘Regulations for Handling Medical Negligence’, and the Health Ministry of the People's Republic of China order no. 32, ‘Medical Negligence Classification Standard’ (2002), level 4 medical negligence contains: (7) non-anatomical variation factors of concern, such as conducting surgical removal of tooth roots and foreign bodies in the maxillary sinus when extracting the maxilla posterior teeth and addressing, and (12) the retention of foreign bodies in soft tissue. In this case series, reports included those on a broken needle that entered the maxillary sinus (case 1), the fractured needles left in alveolar bone (case 4), and a broken needle that stayed in the alveolar mucosa (case 5). All these cases have thus already produced level 4 medical negligence. It is moral to conduct the surgical removal of foreign bodies and eliminate any complications.
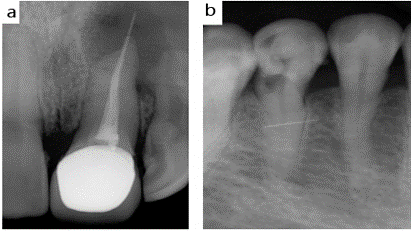
In cases 2 and 4, taking or not taking out the fractured needle located outside the root canal can be argued as necessary, and at what time to do this should be determined according to the specific situation. In case 2, the fractured needle in the root apex area had caused apical periodontitis, formation of a sinus tract, and long-term pyorrhoea. If no action was taken in time, the abscess may continuously expand and endanger adjacent teeth (Figure 8a). Thus, periradicular surgery should be performed as soon as possible. In case 4, the fractured needle was located in the alveolar bone. In this instance, it was not removed, and it did not cause any discomfort or dysfunction neither because of incorporate into the healing of the alveolar bone. As a result, the option of taking it out was suspended to avoid further damage.
Figure 8: Further X-ray images for additional cases. a) Root apex abscess involving an adjacent tooth; b) Broaches penetrated from the wedge-shaped defects and broke off in the alveolar mucosa.
There are many reasons leading to instrument separation during root canal therapy. The main reasons for these case series were the lack of skilled technology and techniques such as expanding needle overexertion, excessive reversion and excessive pressure, not unchoking the root canal carefully before using broaches, or placing too deep, over torsion, or over-extraction when using broaches [3, 8-13]. The instruments themselves may also become the origins of problems, such as repeated usage leading to metal fatigue or over torque. Sometimes, it is possible to push the needle out of the apical foramen of the root canal, making it more difficult to remove the fractured needles. In the cases above, the operation techniques appeared to be crude such as that the technical level is too low to be self-evident. The common forms of instrument separation of the root canal are 1) fracture at narrow points of the perforation of the apical foramen; 2) fracture at places of the perforation of the sidewall, and 3) fracture at locations with wedge-shaped defects [14]. Instrument separation outside the root canal mainly occurs involving broaches, and this was what happened in cases 2, 4 and 5. Cases 2 and 5 presented perforation from the apical, while case 4 discussed perforation via the sidewall.
Also, there were perforations from the locations with wedge-shaped defects to the areas of buccal alveolar mucosa, as shown in (Figure 8b). This situation is caused by unskilled operation. The patient in case 5 complained about suffering from more serious pains while moving the face muscles. This indicates that at least parts of the broken needle had entered the submucosa. So, cutting off the mucosa tissue where the foreign body existed, with help from the X-ray images, might take out the fractured needle. Sometimes, instrument separation inside the root canal (case 3) could happen as well. These could usually be solved by taken out the broken needles by ultrasonic operation or by removing the (whole) affected root canal regions (case 3).
According to the above cases, generally, for the instrument separation occurring outside the root canal: 1) while there is no infection: the fractured needle in the cancellous alveolar bone can be reserved and healed with bone tissues. Fractured needles in soft tissue can also be wrapped in fibrous tissue without further damage. This process will take about 1 to 3 months; 2)while there is no infection, it may form a cyst after being wrapped in fibre as well; 3) while with infection, an abscess in the soft tissue and around the tooth root will be formed and continue to expand; 4) a separated endodontic instrument may affect nearby nerve tissues, causing obvious clinical symptoms and discomfort [7]. Therefore, for the cases of instrument separation outside the root canal that could cause infections (such as in the maxillary sinus), exacerbate existing root inflammation and nerve symptoms, the fractured (instrument) fragments should be removed via early operation, and the control of the infection should be enacted in time.
In the above 3rd situation, in a few cases, cysts may form and gradually expand. Therefore, while met the cases of the fractured needle with infection such as periapical infection, or possibly could cause infection in the case of a needle entering into the maxillary sinus, then earlier surgery should be conducted, and the infection should be controlled as early as possible. The above-mentioned cases 1 and 2 are these situations. As for fractured needles left in the soft tissue, the fractured needles should be removed as early as possible in principle. However, such small fractured needles in the soft tissues (often only 1-3 mm long) is not easy to be found during operations, although, the CBCT and other marketed X-ray instruments can help with the location process. In reality, due to the bleeding, unobvious hand feeling, a lack of strong magnets, and large movement of the soft tissues, it is difficult to achieve an ideal result. Therefore, the best way to avoid the need for metal instrument fragment removal is strictly following the good operating protocols during surgery [15].
Author Contributions
MY, HL and XW conceived the project. MY, HL and XW collected the Cases 1 to 5. XW carried out the surgeries; MY, HL, MW and ZS did the assistance. BC helped to organize and explain the X-ray results. MY, BC, HL and XW drafted the manuscript with contributions from all the other co-authors. All authors read and approved the final manuscript.
Acknowledgments
We are very grateful to the participating individuals and their families.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Thu 16, Jan 2020Accepted: Fri 14, Feb 2020
Published: Wed 19, Feb 2020
Copyright
© 2023 Zhifeng Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2020.01.06
Author Info
Bo Chen Haijiang Liu Min Yi Mingtao Wu Xiaoping Wang Zhifeng Song
Corresponding Author
Zhifeng SongOral Biomedical Engineering Laboratory, Shanghai Stomatological Hospital, Fudan University, Shanghai, China
Figures & Tables
References
- Wang NN, Ge JY, Xie SJ, Chen G, Zhu M (2014) Analysis of Mtwo rotary instrument separation during endodontic therapy: a retrospective clinical study. Cell Biochem Biophys 70: 1091-1095. [Crossref]
- Madarati AA, Hunter MJ, Dummer PM (2013) Management of intracanal separated instruments. J Endod 39: 569-581. [Crossref]
- McGuigan MB, Louca C, Duncan HF (2013) Endodontic instrument fracture: causes and prevention. Br Dent J 214: 341-348. [Crossref]
- Hansen JR, Beeson TJ, Ibarrola JL (2013) Case series: tooth retention 5 years after irretrievable separation of LightSpeedLSX instruments. J Endod 39: 1467-1470. [Crossref]
- Gandevivala A, Parekh B, Poplai G, Sayed A (2014) Surgical removal of fractured endodontic instrument in the periapex of mandibular first molar. J Int Oral Health 6: 85-88. [Crossref]
- Heydari A, Rahmani M, Heydari M (2016) Removal of a Broken Instrument from a Tooth with Apical Periodontitis Using a Novel Approach. Iran Endod J 11: 237-240. [Crossref]
- Ozbek MS, Kaman S, Demiralp KO (2016) Paraesthesia caused by the separated endodontic instrument: case report. Int J Appl Dent Sci 4: 17-19.
- Siqueira JF Jr, Rôças IN, Ricucci D, Hülsmann M (2014) Causes and management of post-treatment apical periodontitis. Br Dent J 216: 305-312. [Crossref]
- Naito T (2010) Surgical or nonsurgical treatment for teeth with existing root filings? Evid Based Dent 11: 54-55. [Crossref]
- Li H, Zhai F, Zhang R, Hou B (2014) Evaluation of microsurgery with SuperEBA as root-end filling material for treating post-treatment endodontic disease: a 2-year retrospective study. J Endod 40: 345-350. [Crossref]
- Song M, Kang M, Kang DR, Jung HI, Kim E (2018) Comparison of the effect of endodontic-periodontal combined lesion on the outcome of endodontic microsurgery with that of isolated endodontic lesion: survival analysis using propensity score analysis. Clin Oral Investig 22: 1717-1724. [Crossref]
- Wang ZH, Zhang MM, Wang J, Jiang L, Liang YH (2017) Outcomes of Endodontic Microsurgery Using a Microscope and Mineral Trioxide Aggregate: A Prospective Cohort Study. J Endod 43: 694-698. [Crossref]
- Jafari F, Jafari S (2017) Importance and methodologies of endodontic microleakage studies: A systematic review. J Clin Exp Dent 9: e812-e819. [Crossref]
- Stoll R, Betke K, Stachniss V (2005) The influence of different factors on the survival of root canal fillings: a 10-year retrospective study. J Endod 31: 783-790. [Crossref]
- Torabinejad M, Corr R, Handysides R, Shabahang S (2009) Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod 35: 930-937. [Crossref]
