Internet Usage May Improve Quality of Life (QoL) in Type 1 Diabetes Mellitus Patients
A B S T R A C T
Objective: To delineate the effect of self-gained information through internet on glycemic control and overall QoL in type 1 diabetes patient.
Methodology: 35 type 1 diabetes patients, who had reasonably good glycemic control were classified by a single clinician into net- savvy and ordinary based on their behaviour towards use of internet to gather information regarding health queries and their glycemic control and QoL analysed.WHO-5 questionnaire which is used in clinical practise was applied.
Result: Of net savvy group (n=18), 14 (82%) had WHO-5 score greater than 13 while among ordinary (n=17) only 7 had WHO5 of same range. Thus, those who surfed internet were in general likely to have better QoL. Among net savvy group all had individual smart phones and used google as search engine. Among ordinary, 40% (9/17) had smart phones. The mean HbA1c of net savvy group was 7.2 which was lower than that of ordinary group mean HbA1c of 7.6. Those of net savvy group were more likely to agree to increase in number of s.c. insulin injections (12/18) as compared to ordinary group (4/17). The self-reported hypoglycemia episodes were also more in net savvy group (6/ person-week) as compared to ordinary (2/ person- week).
Conclusion: Use of smart search engines like google (with strong in-built Artificial Intelligence (AI) systems), even if unsupervised, should be encouraged as part of DSME in type 1 Diabetes patients for optimizing glycemic control and detecting hypoglycemic episodes.
Keywords
Google, type 1 Diabetes mellitus, diabetes education
Introduction
Type 1 Diabetes is chronic disorder requiring training in diabetes self-management and education (DSME). Calorie counting, change in insulin dose, calculating glycemic index of foods, precautions to be taken before and after are some of the specific factors requiring detailed patient education. DSME have been found to be effective in dealing with these objectives and have been widely incorporated in clinical practise [1]. However, in country like India, it’s not always possible to implement DSME in type 1 Diabetes due to time and resource constraints. On the other hand, increasing number of patients are turning to information available online to address DSME queries. The effect of such self-gained information on glycemic control and QoL is not known. The following study aims to address it.
Materials and Methods
This was cross sectional observational study involving adolescent Type 1 Diabetes attending Diabetes clinic OPD under department of Endocrinology & Metabolism. Those with bad glycemic control (HbA1c >9) were excluded. The sample size was determined based on previous study on type 1 diabetes [2]. A total of 35 type 1 diabetes mellitus patients (15-24 years) who consented for study were included. The internet use of the participant was assessed by single clinician using simple questionnaire (Table 1).
Table 1: Classification into net savvy and ordinary.
|
Did you ever try to find out about problems faced by type 1 Diabetes through use of internet? |
Yes/No
|
|
Did you ever use social media to know more about type 1 diabetes? |
Yes/No |
|
Did you us internet to find information about diet and exercise in type 1 diabetes? |
Yes/No |
An affirmative to any of the questions was used to classify an individual as net savvy or ordinary. The subjects were then asked questions pertaining to attituded towards glycemic control intensification, self-diagnosed and confirmed hypoglycemia (defined as glucometer blood glucose <72 mg/dl). Self-monitoring of blood glucose in (SMBG) was assessed by average weekly consumption of glucose strips in last 3 months. As most standard guidelines on type 1 Diabetes suggest at least 4 or more daily SMBG, use of > 25 strips/week was used to ascertain optimum blood glucose monitoring in the participants [1]. Quality of life of last 2 weeks was ascertained using WHO-5 questionnaire (Table 2) as previously reported [2]. All participants were asked about preferred internet search engine. The number of participants in each group were compared using chi-square test. SPSS 19 was used for calculation, A p value of <0.05 was considered significant. The study was approved by Institutional Ethics committee.
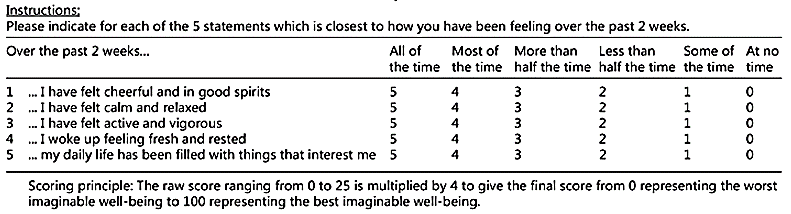
Table 3: Comparison between net savvy and ordinary Type 1 diabetes mellitus group.
|
|
Net savvy (n=18) |
Ordinary(n=17) |
p-value |
|
WHO-5 raw score > 13 |
14 |
7 |
0.03 |
|
Average WHO -5 raw score |
14.2 |
12.5 |
0.09 |
|
HbA1c |
7.2 |
7.6 |
0.02 |
|
Episodes of self-reported hypoglycemia (per person per week) |
6 |
2 |
0.05 |
|
Agreeing to increase the number of subcutaneous insulin injection |
12 |
4 |
0.01 |
|
SMBG monitoring >/= 25 strips/week |
11 |
10 |
0.3 |
|
Use of google as search engine |
18 |
17 |
0.4 |
|
Owning a smartphone |
18 |
9 |
0.08 |
Results
The average age of net savvy group (18.6 years) was not statistically different from those in ordinary group (19.2 years). Among net savvy group all had individual smart phones and used google as search engine. Among ordinary, 40% (9/17) had smart phones. Of net savvy group (n=18), 14 (82%) had WHO-5 raw score greater than 13 while among ordinary (n=17) only 7 had WHO5 of same range. This was statististically significant (Table 3). However, the average WHO-5 between two groups was not statistically significant. The mean HbA1c of net savvy group was 7.2 which was lower than that of ordinary group mean HbA1c of 7.6. Thus, those who used internet were likely to achieve better HbA1c target. The net-savvy group also had better reporting rates of hypoglycemia-(6/ person-week) as compared to ordinary (2/ person-week). They were also more likely to agree to increase in number of subcutaneous (s.c.) insulin injections (12/18) as compared to ordinary group (4/17) (Table 3). Among net savvy group all had individual smart phones and used google as search engine. Even among those in ordinary group, everyone used google as search engine.
Discussion
DSME is intricate part of type 1 Diabetes management and has long been recognized as important tool to achieve management objectives [3]. There has been long list of different mediums, educational material and holistic socio-cultural intervention for DSME in type 1 diabetes in pediatric and adolescent age group [4]. In country like India trained manpower and time constraints often impact DSME quality. There is renewed interest is use of information technology to facilitate health education Indeed, adolescent patients with type 1 diabetes have preferred the use modern information technology mediums for diabetes education [5, 6]. Our study was intended to gauge the effect of use of internet on quality of life and glycemic control among adolescent age group (15-24 years) in real life scenario, when most of information attained by an individual is unsupervised. Since all of the study subjects used google as search engine, we have used the term googling, references to which do exist [7].
The net savvy group in our study had better quality of life as assessed by WHO-5. WHO-5 focusses mainly on psychological well-being and is developed from Major Depression Inventory to measure quality of life. The raw score is multiplied by 4 to get score from 0 (worst imaginable) to 100 (best imaginable) [8]. Thus, raw score 12.5 is generally taken as a cut-off point below which a subject can be deemed to have compromise in quality of life. 82% of subject in net-savy achieved a raw score of above 13 suggesting a subjective feeling of well-being as compared to only 41 % in ordinary group. The cause of better QoL is possibly related to better access to information (even if unsupervised) and thereby a feeling of better control over disease aspect. It could also be due to increase use of social media to seek support system (family and friends).
Those in net savvy group also had better glycemic control. This could be because information gained in unsupervised way motivated them towards practices like better insulin dose adjustment, regular follow up, seeking to learn concepts of calorie counting, bolus calculation, food glycemic index and awareness about diabetes complication. It is documented that those who use type diabetes support programme via social media sites like facebook have better outcomes, especially with regard to hypoglycemia [9]. The fact that hypoglycaemia awareness was better in net savvy group supports this hypothesis. In a prospective study involving adolescent Type 1 Diabetes patients, there were decreased number of diabetic ketosis episodes in those using Facebook. But every internet visit was personalized with patients need and regulated for content by supervising doctor [10]. Our study is different, as we retrospectively analysed the subjects who were using internet unsupervised by any healthcare provider yet demonstrated benefit. Low literacy level and poor numeracy skills have been shown to be associated with adverse glycemic control in type 1 diabetes independent of socioeconomic factors [11].
There can be speculation whether with current socio-economic scenario in India, adolescent with type 1 diabetes mellitus are able to use internet in positive way like their western counterparts. We will point to recent study has shown how adolescent with type 1 diabetes are able to manage a complicated device like insulin pump without contact with a healthcare provider [12]. Ours is first study to indicate benefit even from unsupervised googling. The improved Artificial Intelligence (AI) systems in search engine like google could possibly separate relevant DSME information from misinformation for Type 1 Diabetes and improve quality of DSME. Hitherto poorly defined patient factors like inadequate numeracy skills, can be overcome even without supervision of healthcare provider [11]. Mobile AI application have already shown to replace need for healthcare provider in some areas [13].
Our study had several pitfalls. There was no statistically significant difference between average WHO-5 scores between two groups. This explains the fact that QoL in type diabetes mellitus adolescent is influenced by a lot of complex factors like age, duration, gender, ethnicity, number of insulin injections, socioeconomic status We did not comprehensive study these factors [14]. The sample size was also inadequate and in a retrospective observational study there could be a recall bias. Net savvy ness could also explain an information hungry nature and thereby due increase urge to know about type 1 diabetes management. There was no difference in SMBG by two groups indicating increased online learning may not translate to compliance so called Knowledge attitude practise (KAP)gap or the fact that information regarding SMBG accessed by participants was incorrect [14].
Although extensively validated and used routinely in clinical practise for type 1 diabetes, WHO-5 reflects QoL over preceding 2 weeks while HbA1c is value over 12 weeks. Given two-way relationship between Diabetes and Depression, it is indeed possible that better HbA1c would have increased QoL [15]. More research, especially long-term prospective study is needed to delineate the role of increasing use of internet (often unsupervised) in type 1 Diabetes. Another pitfall we would like to highlight is excellent HbA1c which we had in our subjects. Type 1 DM patients do not tend to have such good glycemic control. It’s possible the study subjects included were highly motivated and well versed in DSME.
Conclusion
Use of smart search engines like google, with strong in-built Artificial Intelligence (AI) systems, even if unsupervised, should be encouraged as part of DSME in type 1 Diabetes patients for optimizing glycemic control and detecting hypoglycemic episodes.
Conflict of Interest
None.
The Ethical Permission
The study was approved by IEC, AIIMS Jodhpur vide approval no AIIMS/IEC/2017/395.
Author Contributions
RS designed the study, wrote first draft and provided critical inputs. DM did statistics and revised the manuscript.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 11, Jul 2020Accepted: Thu 23, Jul 2020
Published: Mon 10, Aug 2020
Copyright
© 2023 Ravindra Shukla. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDMC.2020.01.06
Author Info
Ravindra Shukla Divyangi Mishra
Corresponding Author
Ravindra ShuklaAssociate Professor, Department of Endocrinology & Metabolism, AIIMS Jodhpur, India
Figures & Tables
Table 1: Classification into net savvy and ordinary.
|
Did you ever try to find out about problems faced by type 1 Diabetes through use of internet? |
Yes/No
|
|
Did you ever use social media to know more about type 1 diabetes? |
Yes/No |
|
Did you us internet to find information about diet and exercise in type 1 diabetes? |
Yes/No |
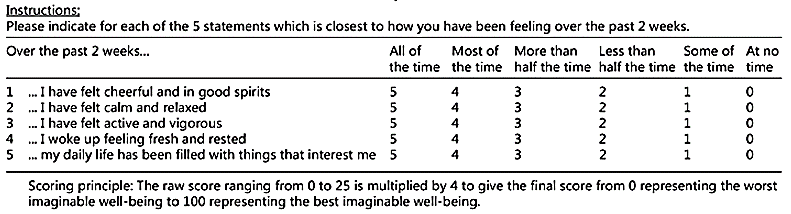
Table 3: Comparison between net savvy and ordinary Type 1 diabetes mellitus group.
|
|
Net savvy (n=18) |
Ordinary(n=17) |
p-value |
|
WHO-5 raw score > 13 |
14 |
7 |
0.03 |
|
Average WHO -5 raw score |
14.2 |
12.5 |
0.09 |
|
HbA1c |
7.2 |
7.6 |
0.02 |
|
Episodes of self-reported hypoglycemia (per person per week) |
6 |
2 |
0.05 |
|
Agreeing to increase the number of subcutaneous insulin injection |
12 |
4 |
0.01 |
|
SMBG monitoring >/= 25 strips/week |
11 |
10 |
0.3 |
|
Use of google as search engine |
18 |
17 |
0.4 |
|
Owning a smartphone |
18 |
9 |
0.08 |
References
- Jane L Chiang, David M Maahs, Katharine C Garvey, Korey K Hood, Lori M Laffe et al. (2018) Type 1 Diabetes in Children and Adolescents: A Position Statement by the American Diabetes Association. Diabetes Care 41: 2026-2044. [Crossref]
- Maartie de Wit, Frans Pouwer, Reinoud J B J Gemke, Henriette A Delemarre-van de Waal, Frank J Snoek (2007) Validation of the WHO-5 Well-Being Index in Adolescents With Type 1 Diabetes. Diabetes Care 30: 2003-2006. [Crossref]
- Thomas Danne, Moshe Phillip, Bruce A Buckingham, Przemyslawa Jarosz-Chobot, Banshi Saboo et al. (2018), ISPAD Clinical Practice Consensus Guidelines 2018 Compendium Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes 27: 115-135. [Crossref]
- S E Hampson, T C Skinner, J Hart, L Storey, H Gage et al. (2001) Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review. Health Technol Assess 5: 1-79. [Crossref]
- Francis S Collins (2015) Exceptional opportunities in medical science: a view from the National Institutes of Health. JAMA 313: 131-132. [Crossref]
- Datta J, Olle H (2002) Adolescent Consultation Day for the NICE Guideline on Type 1 Diabetes: Report Commissioned by the National Collaborating Centre for Women's and Children's Health. London: National Children's Bureau. [Crossref]
- Sarah Khan, Anne Holbrook, Baiju R Shah (2018) Does googling lead to statin intolerance? Int J Cardiol 262: 25-27. [Crossref]
- Staehr Johansen K (1998) The use of well-being measures in primary health care - the DepCare project; in World Health Organization, Regional Office for Europe: Well-Being Measures in Primary Health Care - the DepCare Project. Geneva, World Health Organization, target 12, E60246. [Crossref]
- Zainab A AlQarni, Faisel Yunus, Mowafa S Househ (2016) Health information sharing on Facebook: an exploratory study on diabetes mellitus. J Infect Public Health 9: 708-712. [Crossref]
- Goran Petrovski, Marija Zivkovic (2017) Impact of Facebook on Glucose Control in Type 1 Diabetes: A Three-Year Cohort Study. JMIR Diabetes 2: e9. [Crossref]
- S Marden, P W Thomas, Z A Sheppard, J Knott, J Lueddeke (2012) Poor numeracy skills are associated with glycaemic control in Type 1 diabetes. Diabet Med 29: 662-669. [Crossref]
- Goran Petrovski, Marija Zivkovic, Slavica Subeska Stratrova (2015) Social media and diabetes: can Facebook and Skype improve glucose control in patients with type 1 diabetes on pump therapy? One-year experience. Diabetes Care 38: e51-e52. [Crossref]
- C Peter Waegemann (2010) mHealth: the next generation of telemedicine? Telemed J E Health 16: 23-25. [Crossref]
- David J Pettitt, Jennifer Talton, Dana Dabelea, Jasmin Divers, Giuseppina Imperatore et al. (2014) Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care 37: 402-408. [Crossref]
- Patrick J Lustman, Ray E Clouse (2007) Depression in diabetes: the chicken or the egg? Psychosom Med 69: 297-299. [Crossref]
