Investigating the Diagnostic Value of Ultrasound in Determining the Opposite Inguinal Hernia in Children with Unilateral Inguinal Hernia Diagnosis
A B S T R A C T
Objective: This study was conducted to evaluate and compare the results of ultrasound and clinical examination in the diagnosis of inguinal hernia in children and also to evaluate the benefits and complications of ultrasound in these children.
Study Design: This study, was performed by a cross-sectional method in Children's Medical Center Hospital during 2013-2014 years and follow up was done until July 2020 with the help of a questionnaire from 70 children who had been referred due to unilateral inguinal hernia symptoms. All 70 children underwent Ultrasonographic evaluation and the results of the ultrasound were compared with the initial clinical examination and then with surgery and follow up.
Results: In 95.7% of cases, uni or bilateral inguinal hernia was correctly diagnosed by ultrasound. Ultrasound revealed 13.4% of cases were bilateral and 86.6% were unilateral, all of which were confirmed by surgery. In 17.1% of cases, although they were referred with the chief complaint and clinical examination of unilateral inguinal hernia, Bilateral diagnosis was made for them during the ultrasound, and during the surgery, 75% of them were confirmed to have bilateral inguinal hernia.
Conclusion: Ultrasound is effective in diagnosing the opposite side of the hernia in cases with unilateral hernia.
Keywords
Inguinal hernia, diagnosis of inguinal hernia, children, ultrasound, clinical examination
Introduction
Inguinal hernia is one of the most common surgical conditions in children and occurs in about 0.8 to 5% of newborns (approximately 10 to 20 births per 1000 live births) And more than 30% occurs in premature infants [1-5]. The most common type of inguinal hernia in children is indirect (99%) that is caused by the patency of processus vaginalis (PPV) which has known as the cause of inguinal hernia in children [3, 6]. The causes of metachronous contralateral inguinal hernia (MCIH) is also assumed to be PPV [7]. In surgical cases, in 80% of children, the inguinal hernia is unilateral [1]. And it has been confirmed that children with clinically unilateral inguinal hernia are at risk of MCIH [7]. Development of contralateral hernia after unilateral repair was noted in around 8.8% of cases if the contralateral side was left alone. Hence, detection and closure of contralateral PPV can help to avoid contralateral hernia development but it is difficult to evaluate the contralateral side’s processus vaginalis in asymptomatic cases exploring the contralateral side in children with unilateral hernia or hydrocele, have been discussed many times in the literature, but it is still an unanswered question [8-10].
One of the confirming reasons for the need for an exploration of hernia on the contralateral side is that a strangulated hernia develops when the blood supply to the intestines is compromised, which is a surgical emergency and can cause intestinal obstruction, ischaemia, subsequent necrosis, and perforation .and is therefore associated with erythema, edema, and pain. Irreducible hernias can cause testicular damage and testicular atrophy (15%) In boys, and also ovarian damage in girls [6]. Conventional surgical exploration of the contralateral inguinal canal in children with unilateral hernias or hydrocele leads to an unacceptably high rate of open negative exploration [1]. To prevent MCIH in patients at high risk for bilateral inguinal hernia using techniques such as contralateral inguinal herniotomy, herniography, pneumoperitoneal examination, and laparoscopic examination through hernia sac have been performed. herniotomy in patients with a high risk of bilateral inguinal hernia, which may have some complications such as testicular atrophy and infertility [7, 9, 10]. Herniography and diagnostic pneumoperitoneum are invasive procedures with several complications including hematoma and a bowel perforation [10]. In some cases, the peritoneal veil can result in false-negative findings [9].
Laparoscopic repair of inguinal hernia is performing more and more because it allows contralateral exploration in children and potentially reduces the time of operation and its complications [11]. Proponents of the laparoscopic approach to hernia repair report similar success rates to open surgery. Because it is a safe and effective method, while physical examination, even under anaesthesia, is unreliable. Advantages of laparoscopy over open surgery include; Potential reduction of surgical stress, pain and need for postoperative analgesia, respiratory complications, and postoperative wounds, shortening of postoperative recovery and length of hospital stay, rapid return to the normal diet, improved cosmetic results, ability to easily visualize, Reduce the postoperative complications and fluid shifts that may be associated with it [4, 12, 13]. However, opponents of this approach, argue that laparoscopic examination of the contralateral hernia makes many patients undergo unnecessary surgery. Although the incision is small and the risk of damage to the umbilical cord structure is very low, it is not clear what the benefits of CPPV repair are in the absence of symptoms. Even if CPPV detected in some cases, we cannot be sure about the exact risk of this lesion becoming symptomatic in the future [13]. Also, Special equipment is required for laparoscopic repair, which is not available in all centers.
Furthermore, during the laparoscopic procedure, the peritoneal cavity is usually entered, which is associated with a potential risk of intra-abdominal viscera injury and a lifetime risk of adhesive small bowel obstruction [6]. Preoperative imaging, like inguinal ultrasound, is also used for this purpose so since the discussion of inguinal hernia surgery on the contralateral side has not been resolved in many references and articles yet, in this study, we have decided to evaluate the diagnostic value of ultrasound in determining the contralateral inguinal hernia to prevent reoperation in the unilateral hernia cases, reduce the possible complications of contralateral hernia, avoid unnecessary surgery in cases where there is no real hernia, and reduce unnecessary treatment costs for patients [7, 9, 10].
Methods
This study was a cross-sectional study and the population we studied on, were all infants and children who were candidates for unilateral (chief complaint) inguinal hernia surgery in the surgical ward of Children’s Medical Center for 2 years. The criterion for patients to enter the study included all children with unilateral hernia diagnosis and were in the age range of under 18 years, both boys and girls. Also, patients with bilateral hernia diagnosis were excluded from the study. The dependent variables in this study included the result of the examination and the result of ultrasonography, and the independent variables included age, sex, and age at birth. Each patient's information including age, sex, birth weight, birth age, and family history of the child, was entered into a three-part questionnaire designed for this study. All children were examined by a surgeon and the results of the examination were recorded on the relevant form.
Ultrasonography was performed before the operation for all children who were candidates for surgery due to unilateral inguinal hernia. then bilateral surgery was performed for all patients who were diagnosed as bilateral hernia by ultrasonography. The results of the ultrasonography were recorded by the radiologist and the results of operation on the hernia sac and the condition of the ring were recorded by the surgeon on separate relevant forms. Finally, the results of preoperative physical examination, sonographic, and surgical findings were compared. In the end, the collected data were entered into SPSS statistical software and the data were described by central indicators and data analysis was performed with appropriate statistical tests.
Findings
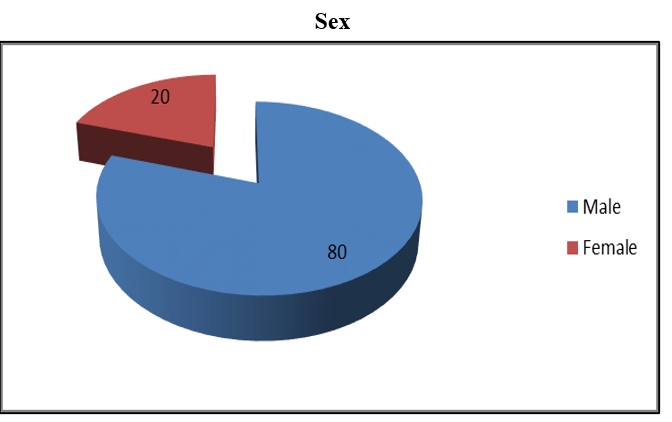
A total of 70 children with a diagnosis of unilateral inguinal hernia were included in this study who were in the age range of under 18 years. In terms of gender, 56 boys (80%) and 14 girls (20%) formed our patients, which is shown in (Table 1) and (Figure 1). Of 70 patients in our study, 48 cases (68.6%) referred with right unilateral inguinal hernia chief complaint (cc) and 22 cases (31.4%) referred with left unilateral inguinal hernia, that all of whom confirmed by clinical examination. Table 2 shows these results. We performed ultrasound for all 70 patients, and base on ultrasound’s diagnosis, we found 14 cases had unilateral left inguinal hernia, 44 cases had unilateral right inguinal hernia, and 12 cases had bilateral inguinal hernia, which is shown in (Table 3).
Figure 1: In our study population, 80% were boys and 20% were girls, which shows a 4-fold prevalence of inguinal hernia in boys.
Table 1: In our study population, 80% were boys and 20% were girls, which shows a 4-fold prevalence of inguinal hernia in boys.
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
|
|
Valid |
Male |
56 |
80.0 |
80.0 |
80.0 |
|
Female |
14 |
20.0 |
20.0 |
100.0 |
|
Bilateral surgery was performed for 12 cases who had a positive diagnosis of bilateral inguinal hernia by ultrasound and it confirmed the diagnose in 9 patients (75%). 4 cases of them had referred with unilateral right hernia cc and 5 cases of them had referred with unilateral left hernia cc. Against the ultrasound’s findings, surgery made the diagnose of unilateral hernia for the other 3 cases (25%), all of whom had referred with right hernia cc. The findings of surgery exploration are shown in (Table 4). And the comparison results of these 12 patients’ chief complaint and surgical exploration findings are shown in (Table 5).
Table 2: Findings of patients with unilateral inguinal hernia that was as same as the patient's clinical examination.
|
Comparison results of CC & ex |
||||||||||
|
|
Examination |
Total |
||||||||
|
|
|
yes |
no |
|||||||
|
CC |
right |
Count %Within CC %Within ex |
48 68.6% 68.6% |
22 31.4% 31.4% |
70 100.0% 100.0% |
|||||
|
left |
Count %Within CC %Within ex |
22 31.4% 31.4% |
48 68.6% 68.6% |
70 100.0% 100.0% |
||||||
|
Total |
Count %Within CC %Within ex |
70 100.0% 100.0% |
70 100.0% 100.0% |
70 100.0% 100.0% |
||||||
|
CC & EX Findings |
||||||||||
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
||||||
|
yes |
no |
|||||||||
|
valid |
Right |
48 |
22 |
68.6 |
68.6 |
68.6 |
||||
|
Left |
22 |
48 |
31.4 |
31.4 |
100.0 |
|||||
|
total |
70 |
70 |
100.0 |
100.0 |
|
|||||
Table 3: We examined all cases by ultrasound, and it was diagnosed that 58 cases had unilateral inguinal hernia and 12 cases had bilateral inguinal hernia.
|
Ultrasound findings of hernia’s Site |
|||||
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
|
|
Valid |
Right Left Right & Left (bilateral) Total |
44 14 12 70 |
62.9 20.0 17.1 100.0 |
62.9 20.0 17.1 |
82.9 20.0 100.0 |
|
Missing System |
0 |
0.0 |
|||
|
Total |
70 |
100.0 |
|||
Table 4: Surgery determined that 9 cases of 12 patients with bilateral diagnosis of ultrasound, had bilateral inguinal hernia and the other 3 cases had unilateral right inguinal hernia.
|
Surgical Findings |
||||||
|
|
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
|
valid |
S.F Right presence of hernia |
Yes |
5 |
41.7% |
41.7% |
41.7% |
|
No |
0 |
0.0% |
0.0% |
41.7% |
||
|
S.F Left presence of hernia |
Yes |
4 |
33.3% |
33.3% |
75.0% |
|
|
No |
3 |
25.0% |
25.0% |
100% |
||
|
Total |
12 |
100.0% |
|
|||
Table 5: Ultrasound made the correct diagnosis in 9 cases (75%) of bilateral inguinal hernias.
|
Comparison results of CC & S.F |
|||||
|
Total |
S.F |
|
|||
|
no |
yes |
|
|||
|
7 100.0% 58.3% |
3 42.9% 100.0% |
4 57.1% 44.4% |
Count %Within CC %Within S.F |
right |
CC |
|
5 100% 41.7% |
0 0.0% 0.0% |
5 100.0% 55.6% |
Count %Within CC %Within S.F |
left |
|
|
12 100.0% 100.0% |
3 25.0% 100.0% |
9 75.0% 100.0% |
count %Within CC %Within S.F |
Total |
|
Table 6: We compared the results of the ultrasound and chief complaint. Although all the 70 patients had referred with unilateral cc and clinical examination, ultrasound diagnosed unilateral hernia just in 58 cases.
|
Comparison of CC/EX and U.F |
|||||
|
Total |
U.F |
|
|||
|
Bilateral |
Unilateral |
|
|||
|
70 100.0% 100.0% |
12 17.1% 100.0% |
58 82.9% 100.0% |
Count %Within cc & ex %Within U.F |
Unilateral |
Cc & ex |
|
0 0.0% 0.0% |
0 0.0% 0.0% |
0 0.0% 0.0% |
Count %Within cc & ex %Within U.F |
Bilateral |
|
|
70 100.0% 100.0% |
12 17.1% 100% |
58 82.9% 100% |
count %Within cc & ex %Within U.F |
Total |
|
Table 7: We compared the results of U.F and S.F in all 70 patients. Ultrasound diagnosed correct diagnosis in 67 patients, in which 58 cases of them were unilateral and 9 of them were bilateral.
|
Comparison of S.F and U.F results |
|||||
|
Total |
S.F |
|
|||
|
Bilateral |
Unilateral |
|
|||
|
58 100.0% 82.9% |
0 0.0% 0.0% |
58 100.0% 95.0% |
Count %Within U.F %Within S.F |
Unilateral |
U.F |
|
12 100% 17.1% |
9 75.0% 100% |
3 25.0% 4.9% |
Count %Within U.F %Within S.F |
Bilateral |
|
|
70 100.0% 100.0% |
9 12.9% 100.0% |
61 87.1% 100.0% |
count %Within U.F %Within S.F |
Total |
|
All 70 patients in our study presented with unilateral hernia chief complaint, which was confirmed by the clinical examination. Ultrasound was performed for all these patients, which was diagnosed as unilateral hernia for 58 patients, and bilateral hernia for 12 patients. All these results are shown in (Table 6). In 58 patients who were diagnosed with unilateral hernia by ultrasound, surgery was performed unilaterally. But for 12 patients diagnosed as bilateral hernia by ultrasound, the contralateral side was explored too. Of these 12 cases, 9 cases were confirmed by surgery, but in 3 cases there was no hernia on the contralateral side, which are shown in (Table 7).
Discussion
The metachronous inguinal hernia has a higher incidence in pediatric patients than adults. The incidence of MCIH in children is 7-15%. However, there is no conclusion as to which patent processus vaginalis (PPV) may develop to be a clinical hernia. However, PPV is known as the cause of MCIH [9, 14]. As Rowe et al. reported, in about 40% of the children with unilateral inguinal hernias the contralateral processus vaginalis will remain patent after the age of 2 years, and half of them will never present with a clinically evident inguinal hernia [15]. when the patient is asymptomatic, it's difficult to understand the status of contralateral processus vaginalis preoperatively [9]. In children diagnosed unilaterally by clinical examination, it is important to check for the presence of CPPV before and during the surgery to reduce the need for a second operation [16]. The discussion about routine exploration for CPPV has continued for several decades. the main point of contention is whether the 10-30% incidence of a return to the OR for the repair of symptomatic contralateral inguinal hernia justifies routine contralateral exploration at the time of repair of unilateral inguinal hernia, or not [13].
Routine surgical exploration of the contralateral inguinal canal in children with unilateral hernias or hydrocele results in an unacceptably high rate of negative surgical explorations [10]. Therefore, for surgeons who perform conventional open hernia surgery in pediatrics, a simple and dependable tool for diagnosing contralateral PPV, is valuable [8]. Exploration of contralateral groin during repair of unilateral hernia can prevent the development of MCIH, another surgery, and another anaesthesia [14]. During the past, various techniques, such as herniography, diagnostic pneumoperitoneum, and also laparoscopy, have been tried. Herniography and diagnostic pneumoperitoneum are invasive procedures with several complications including hematoma and a bowel perforation [10]. In some patients, the peritoneal veil can cause false-negative findings. Two methods of laparoscopic examination are there for observing the contralateral internal inguinal area: through the umbilicus and through the inguinal hernia sac. however, If the hernia sac is too weak, the laparoscopic examination of the hernia sac can't be performed, because of the peritoneal veil, and the failure rate is 3-8% [9].
Based on a report from Antonoff et al., for pediatric surgeons, the rate of the laparoscopic finding of hernia sac in 1996 was 2%, in 2002 was 24%, and in 2005 was 37%. the most accurate method to observe the contralateral PPV is Laparoscopic examination through the umbilicus [17]. In 2014, the prevalence of MCIH in the laparoscopic examination was reported 1.78% through the hernia sac and 0.85% through the umbilicus by Zhong et al. the round ligament in girls which has a role to support the internal genital organs can be preserved by laparoscopy [18]. This is mostly a potential practice with common bilateral exploration in girl's contralateral side negative herniotomy can be reduced by laparoscopy [7]. A study by Klin et al. reports laparoscopy for the hernia sac examination is easy and exact, besides, it can have a role in reducing contralateral negative herniotomy [19]. But it needs Special equipment for laparoscopic repair, which is not available in all centers. Also, during the laparoscopic procedure, the peritoneal cavity is routinely entered, which is associated with a potential risk of intra-abdominal visceral injury and a lifetime risk of adhesive small bowel obstruction [6]. Also, Ultrasonographic evaluation of contralateral groin has been reported for PPV detection. the benefits of Ultrasound include being safe and low cost, non-invasive, and easily repeated.
Groin ultrasound is a precious tool as an adjunct in the management of pediatric hernias by high accuracy detecting PPV [8-10]. However, the accuracy of ultrasound can be affected by its resolution, diagnostic criteria, and person proficiency. Namgoong et al. have reported preoperative ultrasound for inguinal lesion had 20.5% sensitivity, 95.2% specificity, 75% positive predictive value, and 63.2% negative predictive value. Accuracy ultrasound was 64.5% [9]. According to the finding of ultrasound, the surgeon can order uni or bilateral hernia surgery and the prevalence of contralateral hernia development is insignificant. Preoperative groin ultrasound with contralateral PPV closure can be alternative in children to laparoscopic hernia repair for preventing the progression of the contralateral hernia or hydrocele. As a result, the family and physician are allowed to notice the hernia presence before surgery also, in 2015, Kaneda et al. suggested that ultrasound could reduce the prevalence of MCIH by preoperative check [8-10, 20].
In this study, we reported the results of ultrasound in children with a diagnosis of unilateral hernia who were candidates for surgery at the Children’s Medical Center for 2 years. Our primary goal was to evaluate the diagnostic value of ultrasonography in determining the opposite side inguinal hernia. Ultrasound correctly detected the presence of unilateral or bilateral inguinal hernias in 95.7% of cases. 17.1% of the cases, although they had referred with the main complaint and clinical examination of unilateral hernia, were diagnosed bilateral hernia during the ultrasound, and in 75% of them, surgery confirmed the diagnosis of bilateral. According to the results of our study, ultrasonography is effective in diagnosing the contralateral hernia in cases with unilateral hernia. In studies by Hasanuzzaman et al., Zaidi et al., and Hata et al., the accuracy of ultrasound was reported similar to our study, more than 90%. The results of their studies are listed below. Zaidi et al. reported that ultrasound examination for contralateral groin has a very high specificity (97%) with 86.7% positive predictive value and 94.6% negative predictive value for inguinal hernia in children less than 12-year-old [10]. Hata et al. In 2004 used ultrasound in 348 cases of unilateral inguinal hernia, then in 78 patients with sonographically positive PPV, performed bilateral herniotomy.
In comparing the results of ultrasound and herniotomy, ultrasound (with 94.9% accuracy) confirmed the patency in 74 of 78 cases [16]. In 2011, Hasanuzzaman et al. performed ultrasonography for 30 patients of unilateral inguinal hernia for observing the contralateral PPV. 12 opened PPV was founded and bilateral herniotomy was performed. sonography accuracy in this study was 91.7% [21]. Also, Other studies have been performed in this field that confirmed the effect of ultrasound in the diagnosis of contralateral hernias. According to a meta-analysis by Dreuning et al. preoperative ultrasonography because of high sensitivity and specificity, is useful. but They stated there is a need for follow up observations of cases with sonographically negative PPV and as well to clear up the diagnostic criteria of contralateral PPV [22]. And in a study by Toki et al., the incidence of negative exploration before and after performing ultrasonography in the diagnosis of contralateral hernias was 10.2% and 1.5% respectively, that was different significant statistically [23]. In our study population, 80% were boys and 20% were girls, which can be concluded that inguinal hernia is 4 times more common in boys than girls. Also, 20% had left hernia, and 67.1% had right hernia and 12.9% had bilateral hernia, which results in a higher prevalence of right hernia.
Considering that sonography correctly detected the presence of the right hernia sac in 90% of cases and also left hernia sac in 80% of cases, we conclude that ultrasound is effective in diagnosing right and left hernia sac. Ultrasound diagnosis of the presence of the right herniated organ in 90.3% of cases and left herniated organ in 83.3% was confirmed by a procedure that shows that ultrasound is also effective in diagnosing right and left herniated organ. Also, according to the results of this study, ultrasound is effective in diagnosing different degrees of right mild hydrocele, but it is not very effective in diagnosing the degree of left hydrocele. Besides, in this study, during the ultrasound examination, the absence of testicles in the right inguinal canal in 97.9% of cases and the presence of testicles in the right inguinal canal in 2.1% of cases were detected, all of which were confirmed by surgery. As well as examination of the left inguinal canal also confirmed the ultrasound diagnosis of testicular presence or absence in more than 90% of cases by surgery. As a result, ultrasound is effective in examining the inguinal canal. Therefore, if used correctly and accurately measured with ultrasound, this method is the most reliable method for diagnosing hernia, especially in cases where there is an accurate history of the disease, but no relevant clinical findings are seen. Ultrasound is also effective in assessing the possibility of contralateral hernias in children with unilateral hernias.
Article Info
Article Type
Research ArticlePublication history
Received: Thu 22, Oct 2020Accepted: Sat 31, Oct 2020
Published: Sat 21, Nov 2020
Copyright
© 2023 Ashjaei Bahar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.02.05
Author Info
Ashjaei Bahar Amiri Shakiba Najdi Fatemeh Movahedi Jadid Merisa
Corresponding Author
Ashjaei BaharDepartment of Pediatric Surgery, Children Medical Center of Excellence, Tehran University of Medical Sciences, Tehran, Iran
Figures & Tables
Table 1: In our study population, 80% were boys and 20% were girls, which shows a 4-fold prevalence of inguinal hernia in boys.
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
|
|
Valid |
Male |
56 |
80.0 |
80.0 |
80.0 |
|
Female |
14 |
20.0 |
20.0 |
100.0 |
|
Table 2: Findings of patients with unilateral inguinal hernia that was as same as the patient's clinical examination.
|
Comparison results of CC & ex |
||||||||||
|
|
Examination |
Total |
||||||||
|
|
|
yes |
no |
|||||||
|
CC |
right |
Count %Within CC %Within ex |
48 68.6% 68.6% |
22 31.4% 31.4% |
70 100.0% 100.0% |
|||||
|
left |
Count %Within CC %Within ex |
22 31.4% 31.4% |
48 68.6% 68.6% |
70 100.0% 100.0% |
||||||
|
Total |
Count %Within CC %Within ex |
70 100.0% 100.0% |
70 100.0% 100.0% |
70 100.0% 100.0% |
||||||
|
CC & EX Findings |
||||||||||
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
||||||
|
yes |
no |
|||||||||
|
valid |
Right |
48 |
22 |
68.6 |
68.6 |
68.6 |
||||
|
Left |
22 |
48 |
31.4 |
31.4 |
100.0 |
|||||
|
total |
70 |
70 |
100.0 |
100.0 |
|
|||||
Table 3: We examined all cases by ultrasound, and it was diagnosed that 58 cases had unilateral inguinal hernia and 12 cases had bilateral inguinal hernia.
|
Ultrasound findings of hernia’s Site |
|||||
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
|
|
Valid |
Right Left Right & Left (bilateral) Total |
44 14 12 70 |
62.9 20.0 17.1 100.0 |
62.9 20.0 17.1 |
82.9 20.0 100.0 |
|
Missing System |
0 |
0.0 |
|||
|
Total |
70 |
100.0 |
|||
Table 4: Surgery determined that 9 cases of 12 patients with bilateral diagnosis of ultrasound, had bilateral inguinal hernia and the other 3 cases had unilateral right inguinal hernia.
|
Surgical Findings |
||||||
|
|
|
|
Frequency |
Percent |
Valid percent |
Cumulative percent |
|
valid |
S.F Right presence of hernia |
Yes |
5 |
41.7% |
41.7% |
41.7% |
|
No |
0 |
0.0% |
0.0% |
41.7% |
||
|
S.F Left presence of hernia |
Yes |
4 |
33.3% |
33.3% |
75.0% |
|
|
No |
3 |
25.0% |
25.0% |
100% |
||
|
Total |
12 |
100.0% |
|
|||
Table 5: Ultrasound made the correct diagnosis in 9 cases (75%) of bilateral inguinal hernias.
|
Comparison results of CC & S.F |
|||||
|
Total |
S.F |
|
|||
|
no |
yes |
|
|||
|
7 100.0% 58.3% |
3 42.9% 100.0% |
4 57.1% 44.4% |
Count %Within CC %Within S.F |
right |
CC |
|
5 100% 41.7% |
0 0.0% 0.0% |
5 100.0% 55.6% |
Count %Within CC %Within S.F |
left |
|
|
12 100.0% 100.0% |
3 25.0% 100.0% |
9 75.0% 100.0% |
count %Within CC %Within S.F |
Total |
|
Table 6: We compared the results of the ultrasound and chief complaint. Although all the 70 patients had referred with unilateral cc and clinical examination, ultrasound diagnosed unilateral hernia just in 58 cases.
|
Comparison of CC/EX and U.F |
|||||
|
Total |
U.F |
|
|||
|
Bilateral |
Unilateral |
|
|||
|
70 100.0% 100.0% |
12 17.1% 100.0% |
58 82.9% 100.0% |
Count %Within cc & ex %Within U.F |
Unilateral |
Cc & ex |
|
0 0.0% 0.0% |
0 0.0% 0.0% |
0 0.0% 0.0% |
Count %Within cc & ex %Within U.F |
Bilateral |
|
|
70 100.0% 100.0% |
12 17.1% 100% |
58 82.9% 100% |
count %Within cc & ex %Within U.F |
Total |
|
Table 7: We compared the results of U.F and S.F in all 70 patients. Ultrasound diagnosed correct diagnosis in 67 patients, in which 58 cases of them were unilateral and 9 of them were bilateral.
|
Comparison of S.F and U.F results |
|||||
|
Total |
S.F |
|
|||
|
Bilateral |
Unilateral |
|
|||
|
58 100.0% 82.9% |
0 0.0% 0.0% |
58 100.0% 95.0% |
Count %Within U.F %Within S.F |
Unilateral |
U.F |
|
12 100% 17.1% |
9 75.0% 100% |
3 25.0% 4.9% |
Count %Within U.F %Within S.F |
Bilateral |
|
|
70 100.0% 100.0% |
9 12.9% 100.0% |
61 87.1% 100.0% |
count %Within U.F %Within S.F |
Total |
|
References
- Dreuning KMA, Broeke CEMT, Twisk JWR, Robben SGF, Rijnet RRV et al. (2019) Diagnostic accuracy of preoperative ultrasonography in predicting contralateral inguinal hernia in children: a systematic review and meta-analysis. Eur Radiol 29: 866-876. [Crossref]
- Cao Z, Chen J, Li Z, Li G (2018) Modified 2-port laparoscopic herniorrhaphy with Kirschner wire in children: A retrospective review. Medicine 97: e12790. [Crossref]
- Hutson JM, O’Brien M, Beasley SW, Teague WJ, King SK (2015) Jones’ clinical paediatric surgery. 7th edn. Chichester: John Wiley & Sons, 332.
- Batavia JPV, Tong C, Chu DI, Kawal T, Srinivasan AK (2018) Laparoscopic inguinal hernia repair by modified peritoneal leaflet closure: Description and initial results in children. J Pediatr Urol 14: 272.e1-272.e6. [Crossref]
- Crankson SJ, Tawil KA, Namshan MA, Jadaan SA, Baylon BJ et al. (2015) Management of inguinal hernia in premature infants: a 10-year experience. J Indian Assoc Pediatr Surg 20: 21-24. [Crossref]
- Evie Y, Pacilli M, Nataraja RM (2020) Inguinal hernias in children. Aust J Gen Pract 49: 38-43. [Crossref]
- Kokorowski PJ, Wang HHS, Routh JC, Hubert KC, Nelson CP (2014) Evaluation of the contralateral inguinal ring in clinically unilateral inguinal hernia: a systematic review and meta-analysis. Hernia 18: 311-324. [Crossref]
- Yip PKF (2019) Ultrasound detection and closure of contralateral patent processus vaginalis in pediatric patients with unilateral inguinal hernia and hydrocele: a longitudinal study to prove efficacy in avoiding contralateral hernia development. Hernia 23: 1253-1259. [Crossref]
- Namgoong JM, Choi WY (2019) Reliability of Preoperative Inguinal Sonography for Evaluating Patency of Processus Vaginalis in Pediatric Inguinal Hernia Patients. Int J Med Sci 16: 247-252. [Crossref]
- Zaidi SH, Rahman JU, Siddiqui TS, Rehman HU, Ahmed N et al. (2017) Exploration Of The Contralateral Groin In Paediatric Inguinal Hernia Or Hydrocele Based On Ultrasound Findings - Is It Justified? J Ayub Med Coll Abbottabad 29: 26-29. [Crossref]
- Dreuning K, Maat S, Twisk J, Heurn EV, Derikx J (2019) Laparoscopic versus open pediatric inguinal hernia repair: state-of-the-art comparison and future perspectives from a meta-analysis. Surg Endosc 33: 3177-3191. [Crossref]
- Gupta R, Singh S (2009) Challenges in paediatric laparoscopic surgeries. Indian J Anaesth 53: 560-566. [Crossref]
- Valusek PA, Spilde TL, Ostlie DJ, Peter SDS, Morgan WM 3rd et al. (2006) Laparoscopic evaluation for contralateral patent processus vaginalis in children with unilateral inguinal hernia. J Laparoendosc Adv Surg Tech A 16: 650-653. [Crossref]
- Dreuning KMA, Broeke CEMT, Twisk JWR, Robben SGF, Rijn RRV et al. (2019) Diagnostic accuracy of preoperative ultrasonography in predicting contralateral inguinal hernia in children: a systematic review and meta-analysis. Eur Radiol 29: 866-876. [Crossref]
- Rowe MI, Copelson LW, Clatworthy HW (1969) The patent processus vaginalis and the inguinal hernia. J Pediatr Surg 4: 102-107. [Crossref]
- Hata S, Takahashi Y, Nakamura T, Suzuki R, Kitada M et al. (2004) Preoperative sonographic evaluation is a useful method of detecting contralateral patent processus vaginalis in pediatric patients with unilateral inguinal hernia. J Pediatr Surg 39: 1396-1399. [Crossref]
- Antonoff MB, Kreykes NS, Saltzman DA, Acton RD (2005) American academy of pediatrics section on surgery hernia survey revisited. J Pediatr Surg 40: 1009-1014. [Crossref]
- Zhong H, Wang F (2014) Contralateral metachronous hernia following negative laparoscopic evaluation for contralateral patent processus vaginalis: a meta-analysis. J Laparoendosc Adv SurgTech A 24: 111-116. [Crossref]
- Klin B, Efrati Y, Kishk IA, Stolero S, Lotan G (2010) The contribution of intraoperative trans inguinal laparoscopic examination of the contralateral side to the repair of inguinal hernias in children. World J Pediatr 6: 119-124. [Crossref]
- Kaneda H, Furuya T, Sugito K, Goto S, Kawashima H et al. (2015) Preoperative ultrasonographic evaluation of the contralateral patent processus vaginalis at the level of the internal inguinal ring is useful for predicting contralateral inguinal hernias in children: a prospective analysis. Hernia 19: 595-598. [Crossref]
- Hasanuzzaman SM, Chowdhury LH, Sarker RN, Bari MS, Talukder SA et al. (2011) Ultrasonographic evaluation of contralateral exploration of patent processus vaginalis in unilateral inguinal hernia. Mymensingh Med J 20: 192-196. [Crossref]
- Dreuning KMA, Broke CEMT, Twisk JWR, Robben SGF, Rijn RRV et al. (2018) Diagnostic accuracy of preoperative ultrasonography in predicting contralateral inguinal hernia in children: a systematic review and meta-analysis. Eur Radiol 29: 866-876. [Crossref]
- TokiA, OguraK, Miyauchi A (1995) Ultrasonographic diagnosis of inguinal hernia in children. Pediatr Surg Int 10: 541-543.
