Late-Onset of Keratocysts in De Novo Mutation c.1347+1G>A on Intron 9 PTCH1- (NBCCS) – Diagnosis and Therapy
A B S T R A C T
Introduction: The occurrence of two main symptoms (calcification of the falx cerebri, odontogenic keratocysts, basal cell carcinoma) and a minimum of one secondary symptom is necessary for de-novo diagnosing a Basal Cell Nevus Syndrome (BCNS). Late diagnosing is usual if the primary symptoms are absent. Subtypes of BCNS may express phenotypes at different ages. Early recognition is needed. The adhesion of keratocysts to the basal bone layer varies, so different treatment options are standard.
Aim: A 47-year-old woman without clinical signs of BCNS except macrocephaly suffered from de-novo-mutation of the PTCH1 gene. Odontogenic keratocysts were recognized sporadically by CB-CT ten years later, as late-onset; Compared to subsequent generations, who often present the main symptoms in childhood. The indication of resection, marsupialization, or enucleation with or without Carnoy-solution is a clinical decision.
Conclusion: Despite 100% penetrance, intrafamilial expression of the clinical phenomenon is variable. In child morbidity, the parents’ lifelong co-screening should be mandatory by radiological and clinical investigation. Late-onset KCOT should be resected en-bloc, including soft tissue movement. Enucleation has less morbidity for mandibular keratocysts near the nerve. Carnoy-solution helps minimize the risk of relapse.
Keywords
Gorlin syndrome, basal cell nevus syndrome, falx cerebral calcification, keratocystic odontogenic tumor, PTCH1
Introduction
Gorlin-Goltz-Syndrome (basal cell nevus syndrome (BCNS)) is well-known for a prevalence of 1:50.000 to 1:150.000 and was first described by Gorlin et al. in 1960 [1]. It is a hereditary disease, an autosomal dominant trait characterized by high penetration and variable phenotypical expression [2]. A direct molecular genetic test confirms germline mutation in the PTCH1 gene chromosome 9q22.32. A multidisciplinary approach is necessary since the clinical symptoms often begin in adolescents, in the case of medulloblastomas, even in early childhood [3, 4]. Patients older than 20y have calcification of the falx [5]. Pathognomonic for BCNS are keratocystic odontogenic tumors (KCOT) in the jaws and multiple basal cell carcinomas. Skeletal abnormities are pits, bifid ribs, hypertelorism, and macrocephaly. They should be carefully detected [6-9]. For maxillofacial regions, a CB-CT is favourable for diagnostic reasons [10, 11].
Aim
Parental generations should have genetic counseling by a specialist after detecting a mutation of the long arm of the chromosome 9q22.3 (PTCH1) in subsequent generations. To detect main symptoms like calcification of the falx cerebri, odontogenic keratocysts, basal cell carcinomas, and secondary symptoms (e.g., macrocephaly, cleft lip and palate, spine/rib abnormalities or polydactyly). Therefore, secondary symptoms often appear earlier and should receive more attention to avoid the extent of the destruction. There are various options for treating keratocysts: marsupialization enucleation, and block resection [12, 13].
Late-onset KCOT should be resected en-bloc, including soft tissue movement. Some authors recommend Enucleation for mandibular keratocysts near the nerve [14-18]. Carnoy-solution helps minimize the risk of relapse [13, 19-21].
Case Presentation
I Diagnosis
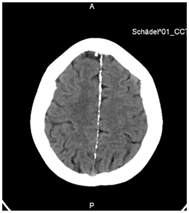
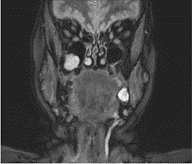
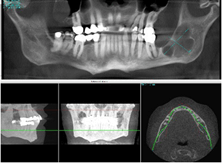
A 47-year-old woman suffered from a de novo mutation c.1347+1G>A on Intron 9 PTCH1-Gene and suspected BCNS. Diagnostical staging results in main symptoms: Calcification of the falx cerebri (Figure 1) and odontogenic keratocysts (Figures 2 & 3). So far, no basal cell carcinomas and point-shaped pits in the palmoplantar skin have appeared. Evident as secondary symptoms macrocephaly, strabismus, hypertelorismus, and bifid ribs appeared.
Figure 1: CT-Scan from the head with calcification of the falx cerebri at the age of 57 years.
Figure 2: Front- plane NMR of the mother at the age of 57 years.
Figure 3: CBCT: multiple keratocyst (left mandible and right posterior sinus maxillaris).
II Treatment
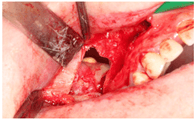
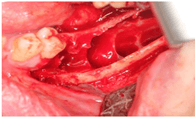
Due to the strong adhesion of the maxilla keratocysts, we resected en-block with piezo- surgery [Piezosurgery® touch, Saw OT7A, Mectron-Deutschland, D-Köln]. For 3 minutes, we plugged a cotton swab soaked in freshly prepared Carnoy's solution [absolute alcohol 6 mL, chloroform 3 mL, glacial acetic acid 1 mL, ferric chloride 0.1 gm/mL; Engelbrecht Labortechnik, Edermünde, Germany] as chemical cauterization [20, 21].
Figure 4: KOT right maxilla with resorption of the anterior wall of the sinus.
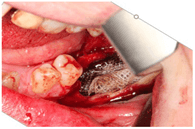
For facial reconstruction, we used the Bichat fat pad for closure. The keratocysts showed macroscopically clinically different colorations with partly yellowish discoloration. Enucleation removed the multicystic keratocysts in the mandible. We used Carnoy-solution for intraluminal injection and post excavatum as chemical cautery of the bony cavity [19]. Tooth 36, which was in the cyst cluster, was osteotomized. We filled the cavity by using the PRGF technique, according to Anitua et al. 2012 [22].
Figure 5: En-bloc-resection of KOT in the right maxilla.
Figure 6: Clinical view of the multilocular KOT in the left mandible after enucleation.
Figure 7: Chemical cauterization of the KOT-cavity with Carnoy-solution on absorbent cotton.
Histological Examination of KCOT
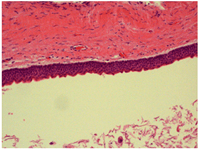
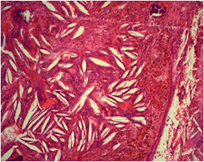
The multilayer squamous epithelium is in line and has an orthokeratotic part of cystic walls (Figure 8). The surface is wave-shaped and palisade like reserve cells. The basement membrane is intact. Horn materials and macrophages peeled off in the lumen. Subepithelial and alternately dense and perivascular accentuated lymph plasma cell infiltrate. Areas with curly collagenous fiber tissue include sparse myelinated nerve fibers. The bony parts show vital osteocytes. The bone lamellae have slightly irregular putty lines and loose collagen fiber tissue. They accumulated sparse associations of a multilayered epithelium with a giant cell reaction around cholesterol voids (Figure 9).
Figure 8: Histological findings of syndromic KCOT (magnification of x 150 H.E.) with regular multilayer squamous epithelium with palisade like up lined reserve cells.
Figure 9: Histological findings of the altered KCOT (magnification of x 240 H.E.) with loose collagen fiber and giant cell reaction around cholesterol voids.
Discussion
I Diagnosis
KCOT are frequently diagnosed incidentally [1, 5, 13, 23]. To avoid extensive lesions, frequent dental check-ups and multimodal therapy are necessary [24-26]. Furthermore, genetic counseling of the entire family is recommendable due to the dominant inheritance. The mother’s 11-year-old boy had early onset of multiple keratocyst, macrocephaly, hypertelorism, and calcification of the falx cerebri [25]. The sister was not affected by the BCNS but showed bifid ribs like her mother. The family was informed about the high risk of recurrence of keratocysts and basal cell carcinoma development.
Diagnoses are often backward detected, as described by Yordonova et al. 2007, who investigated late detection of multiple keratocysts of a 50-year-old mother after screening a BCNS in her 18-year-old daughter [27]. If BCNS is suspected, family examinations sometimes show pair mutations. In the case-report described by Hedge et al., a 38-year-old mother was co-screened with her eight-year-old daughter, who showed odontogenic keratocytes [28]. A meta-analysis of the syndromic keratocystic odontogenic tumor is presented by Antonoglu et al. 2014 [29]. Individuals with BCNS mutations showed a wide range of clinical variations. Pastorino et al. (2005) investigated the genotype/phenotype correlation in BCNS and concluded that carrier and type of mutation did not influence when the patients developed oral keratocysts or basal cell carcinoma. They recommend lifetime supervision in the case of BCNS [30]. Twin-examination shows multiple keratocysts in almost identical areas, as described by Anchlia et al. (2015) [31].
II Treatment
The surgical procedure should enable the combination of minimized morbidity and a low recurrence of the keratocysts [32]. Various therapy options are available for this with increasing intervention effort: enucleation, enucleation with peripheral ostectomy, enucleation with Carnoy-Solution resection [18, 33-39]. The pooled weighted overall treatments of KOT was 16.6%, according to Al-Moraissi et al. (2017) [32]. There is significant heterogeneity among the studies. The weighted event rate of pooled recurrence for 17 studies is 23.1% [32]. For enucleation with peripherical ostectomy, they found a recurrence rate of 17.4% by evaluating eight studies (n= 378). Some countries do not allow Carnoy-solution (CS) including chloroform, according to Dashow et al. 2013, because of the precancerous potential of chloroform [21]. So modified Carnoy-solution without chloroform was used (MC). After 12-51 month follow up (n=210), MC treated patients significantly more relapses (19.2%) compared to CS patients (8.3%). Chiripathomsakul et al. had a recurrence rate of 22.6%. 71.4% of the relapses occurred within five years [24]. A systematic review of 35 pooled studies (n=576) results in recurrence rates of 11.5% [32]. A systematic review of Cochrane-analysis concludes en-bloc or marginal resection as the ultima ratio [40]. A recurrence rate of 8.4% (n=92) in case of resection is estimated [32]. Stoelinga (2001) and Stoelinga & Bronkhorst (1987) recommend resection including soft tissue margin because of satellite cells and cystic remnants in the surrounding tissue [41, 42]. An opinion shared by other authors [6, 9, 12, 24, 25, 32].
Conclusion
Clinical expression of symptoms is variable despite a penetrance of 100%. In the case of child morbidity, the parents' lifelong co-screening should be mandatory by radiological and clinical investigation. Radical resection of late-onset KCOT appears to be a sure option in syndromic cases, including soft tissue movement. For non-syndromic cases, the literature advocates enucleation with the application of Carnoy-solution or as first line-treatment to minimize the risk of relapse.
Consent
The patient gave written consent for publication. The author ensure that the work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). The manuscript is in line with the Recommendations for the Conduct, Reporting, Editing and Publication of Scholarly Work in Medical Journals and aim for the inclusion of representative human populations (sex, age, and ethnicity) as per those recommendations.
Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
None.
Abbreviations
BCNS: Basal Cell Nevus Syndrome
CBCT: Cone Beam Computed Tomography
CS: Carnoy Solution
GGS: Gorlin-Goltz-Syndrome
H.E.: Hematoxylin-Eosin-stained
KCOT: Keratocystic Odontogenic Tumor
MC: Modified Carnoy-Solution
NBCCS: Nevoid Basal Cell Carcinoma Syndrome
NMR: Nuclear Magnetic Resonance
OPT: Orthopantomography
PTCH1: Protein Patched Homolog 1
Article Info
Article Type
Case ReportPublication history
Received: Mon 07, Dec 2020Accepted: Mon 21, Dec 2020
Published: Wed 30, Dec 2020
Copyright
© 2023 Manfred Nilius. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GG.2020.01.06
Author Info
Manfred Nilius Minou Nilius Charlotte Mueller Guenter Lauer
Corresponding Author
Manfred NiliusNiliusklinik, Londoner Bogen, Dortmund, Germany
Figures & Tables

References
- Gorlin RJ, Goltz RW (1960) Multiple nevoid basal-cell epithelioma, jaw cysts, and bifid rib. A syndrome. N Engl J Med 262: 908-912. [Crossref]
- Hodgkinson DJ, Woods JE, Dahlin DC, Tolman DE (1978) Keratocysts of the jaw. Clinicopathologic study of 79 patients. Cancer 41: 803-813. [Crossref]
- Friedrich RE (2007) Diagnosis and treatment of patients with nevoid basal cell carcinoma syndrome Gorlin-Goltz syndrome (GGS). Anticancer Res 27: 1783-1787. [Crossref]
- Muzio L (2008) Nevoid basal cell carcinoma syndrome (Gorlin syndrome). Orphanet J Rare Dis 3: 32. [Crossref]
- Khaliq MIU, Shah AA, Ahmad I, Hasan S, Jangam SS et al. (2016) Keratocystic odontogenic tumors related to Gorlin-Goltz syndrome: a clinicopathological study. J Oral Biol Craniofac Res 6: 93-100. [Crossref]
- Titinchi F, Nortje CJ, Parker ME, van Rensburg LJ (2013) Nevoid basal cell carcinoma syndrome: a 40-year study in the south African population. J Oral Pathol Med 42: 162-165. [Crossref]
- Pol C, Ghige S, Kalaskar R, Gosavi S (2013) Gorlin-Goltz syndrome: a rare case report. Contemp Clin Dent 4: 547-550. [Crossref]
- Sasaki R, Miyashita T, Matsumoto N, Fujii K, Saito K et al. (2010) Multiple keratocystic odontogenic tumors associated with nevoid basal cell carcinoma syndrome having distinct PTCH1 mutations: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110: e41-e46. [Crossref]
- Guo YY, Zhang JY, Li XF, Luo HY, Chen F, Li TJ (2013) PTCH1 gene mutations in Keratocystic odontogenic tumors: a study of 43 Chinese patients and a systematic review. PLoS One 8: e77305. [Crossref]
- Sánchez Burgos R, González Martín Moro J, Pérez Fernández E, Burgueño García M (2014) Clinical, radiological and therapeutic features of keratocystic odontogenic tumours: a study over a decade. J Clin Exp Dent 6: e259-e264. [Crossref]
- Apajalahti S, Hagström J, Lindqvist C, Suomalainen A (2011) Computerized tomography findings and recurrence of keratocystic odontogenic tumor of the mandible and maxillofacial region in a series of 46 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111: e29-e37. [Crossref]
- Voorsmit RA, Stoelinga PJ, van Haelst UJ (1981) The management of keratocysts. J Maxillofac Surg 9: 228-236. [Crossref]
- Gosau M, Draenert FG, Müller S, Frerich B, Bürgers R et al. (2010) Two modifications in the treatment of keratocystic odontogenic tumors (KCOT) and the use of Carnoy's solution (CS)- a retrospective study lasting between 2 and 10 years. Clin Oral Investig 14: 27-34. [Crossref]
- Mendes RA, Carvalho JFC, van der Waal I (2010) Characterization and management of the keratocystic odontogenic tumor in relation to its histopathological and biological features. Oral Oncol 46: 219-225. [Crossref]
- Morgan TA, Burton A, Qian F (2005) A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg 63: 635-639. [Crossref]
- Maurette PE, Jorge J, de Moraes M (2006) Conservative treatment protocol of odontogenic keratocyst: a preliminary study. J Oral Maxillofac Surg 64: 379-383. [Crossref]
- Jensen J, Sindet Pedersen S, Simonsen EK (1988) A comparative study of treatment of keratocysts by Enucleation or Enucleation combined with cryotherapy. A preliminary report. J Craniomaxillofac Surg 16: 362-365. [Crossref]
- Güler N, Şençift K, Demirkol Ö (2012) Conservative management of keratocystic odontogenic tumors of jaws. ScientificWorldJournal 2012: 680397. [Crossref]
- Rao K, Kumar S (2014) The use of Enucleation and chemical cauterization (Carnoy's) in the management of odontogenic keratocyst of the jaws. Indian J Otolaryngol Head Neck Surg 66: 8-12. [Crossref]
- Ribeiro Junior OR, Borba AM, Alves CA, de Gouveia MM, Coracin FL et al. (2012) Keratocystic odontogenic tumors and Carnoy's solution: results and complications assessment. Oral Dis 18: 548-557. [Crossref]
- Dashow JE, McHugh JB, Braun TM, Edwards SP, Helman JI et al. (2013) Significantly Decreased Recurrence Rates in Keratocystic Odontogenic Tumor With Simple Enucleation and Curettage Using Carnoy's Versus Modified Carnoy's Solution. J Oral Maxillofac Surg 73: 2132-2135. [Crossref]
- Anitua E, Prado R, Orive G (2012) Bilateral sinus elevation evaluation plasma rich in growth factors technology: a report of five cases. Clin Implant Dent Relat Res 14: 51-60. [Crossref]
- Boffano P, Ruga E, Gallesio C (2010) Keratocystic odontogenic tumor (odontogenic keratocyst): preliminary retrospective review of epidemiologic, clinical, and radiologic features of 261 lesions from University of Turin. J Oral Maxillofac Surg 68: 2994-2999. [Crossref]
- Chirapathomsakul D, Sastravaha P, Jansisyanont P (2006) A review of odontogenic keratocyst and the behavior of recurrences. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101: 5-9. [Crossref]
- Nilius M, Kohlhase J, Lorenzen J, Lauer G, Schulz MC (2019) Multidisciplinary oral rehabilitation of an adolescent suffering from juvenile Gorlin-Goltz syndrome - a case report. Head Face Med 15: 5. [Crossref]
- Pastorino L, Pollio A, Pellacani G, Guarneri C, Ghiorzo P et al. (2012) Novel PTCH1 mutations in patients with keratocystic odontogenic tumors screened for nevoid basal cell carcinoma (NBCC) syndrome. PLoS One 7: e43827. [Crossref]
- Yordanova I, Gospodinov D, Veselin K, Pavlova V, Radoslavova G (2007) A familial case of Gorlin-Goltz syndrome. J IMAB Annu Proc (Sci Papers) 13: 63-66.
- Hegde S, Shetty S (2012) Radiological features of familial Gorlin-Goltz syndrome. Imaging Sci Dent 42: 55-60. [Crossref]
- Antonoglou GN, Sándor GK, Koidou VP, Papageorgiou SN (2014) Non-syndromic and syndromic keratocystic odontogenic tumors: systematic review and meta-analysis of recurrences. J Craniomaxillofac Surg 42: e364-e371. [Crossref]
- Pastorino L, Cusano R, Baldo C, Forzano F, Nasti S (2005) Nevoid Basal Cell Carcinoma Syndrome in infants: improving diagnosis. Child Care Health Dev 31: 351-354. [Crossref]
- Anchlia S, Vyas S, Bahl S, Nagavadiya V (2015) Gorlin-Goltz syndrome in twin brothers: an unusual occurrence with review of the literature. BMJ Case Rep 2015: bcr2015211608. [Crossref]
- Al Moraissi EA, Dahan AA, Alwadeai MS, Oginni FO, Al Jamali JM et al. (2017) What surgical treatment has the lowest recurrence rate following the management of keratocystic odontogenic tumors? A large systematic review and meta- analysis. J Craniomaxillofac Surg 45: 131-144. [Crossref]
- Pitak Arnnop P, Chaine A, Oprean N, Dhanuthai K, Bertrand JC et al. (2010) Management of odontogenic keratocysts of the jaws: a ten-year experience with 120 consecutive lesions. J Cranio-Maxillofacial Surg 38: 358-364. [Crossref]
- Schmidt BL, Pogrel MA (2001) The use of Enucleation and liquid nitrogen cryotherapy in the management of odontogenic keratocysts. J Oral Maxillofac Surg 59: 720-725. [Crossref]
- Nagy K, Kiss E, Erdei C, Oberna F, Fejérdy P et al. (2008) Complex care by multiple medical and dental specialists of a patient with aggressive Gorlin-Goltz syndrome. Postgrad Med J 84: 330-332. [Crossref]
- Kinard BE, Chuang SK, August M, Dodson TB (2013) How well do we manage the odontogenic keratocyst? J Oral Maxillofac Surg 71: 1353-1358. [Crossref]
- Tolstunov L, Treasure T (2008) Surgical treatment algorithm for odontogenic keratocyst: combined treatment of odontogenic keratocyst and mandibular defect with marsupialization, Enucleation, iliac crest bone graft, and dental implants. J Oral Maxillofac Surg 66: 1025-1036. [Crossref]
- Shimada Y, KI M, Kabasawa Y, Taguchi T, Omura K (2013) Clinical manifestations and treatment for keratocystic odontogenic tumors associated with nevoid basal cell carcinoma syndrome: a study in 25 Japanese patients. J Oral Pathol Med 42: 275-280. [Crossref]
- Titinchi F, Nortje CJ (2012) Keratocystic odontogenic tumor: a recurrence analysis of clinical and radiographic parameters. Oral Surg Oral Med Oral Pathol Oral Radiol 114: 136-142. [Crossref]
- Sharif FN, Oliver R, Sweet C, Sharif MO (2010) Interventions for the treatment of keratocystic odontogenic tumors (KCOT, odontogenic keratocysts (OKC)). Cochrane Database Syst Rev 9: CD008464. [Crossref]
- Stoelinga PJ (2001) Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg 30: 14-25. [Crossref]
- Stoelinga PJ, Bronkhorst FB (1987) The incidence, multiple presentation, and recurrence of aggressive cysts of jaws. J Craniomaxillofac Surg 15: 184-195. [Crossref]
- Marker P, Brøndum N, Clausen PP, Bastian HL (1996) Treatment of large odontogenic keratocysts by decompression and later cystectomy: a long-term follow-up and a histologic study of 23 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82: 122-131. [Crossref]
- Sahu S, Sahoo S, Banerjee R, Ghosh S (2019) An enigma of Gorlin-Goltz syndrome: Two cases reported in mother and daughter. J Oral Maxillofac Pathol 23: 115-121. [Crossref]
- Kaczmarzyk T, Mojsa I, Stypulkowska J (2012) A systematic review of the recurrence rate for keratocystic odontogenic tumor in relation to treatment modalities. Int J Oral Maxillofac Surg 41: 756-767. [Crossref]
- Kolokythas A, Fernandes RP, Pazoki A, Ord RA (2007) Odontogenic keratocyst: to decompress or not to decompress? A comparative study of decompression and Enucleation versus resection/peripheral ostectomy. J Oral Maxillofac Surg 65: 640-644. [Crossref]
- Johnson NR, Batstone MD, Savage NW (2013) Management and recurrence of keratocystic odontogenic tumor: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 116: e271-e276. [Crossref]
