Left Facial Primary Leiomyosarcoma Misdiagnosed as Atypical Fibroxanthoma and Immunochemical Markers Relevant to Diagnosis: A Case Report
A B S T R A C T
Soft tissue sarcomas are relatively rare neoplasms of mesenchymal origin that generally make up less than 2% of all adult malignant neoplasms. Atypical fibroxanthoma is a benign soft tissue tumor often confused with malignant variants of similar tumors such as leiomyosarcoma due to similar staining markers and cell morphology. We report a case of a 70-year-old caucasian male who initially presented with a 2 cm exophytic left facial lesion that was misdiagnosed as atypical fibroxanthoma upon biopsy. The patient underwent a wide local excision of the growing 11 cm mass and immediate reconstruction with a cervicofacial flap and full thickness skin graft. Pathological analysis of the specimen revealed the final diagnosis as confirmed primary leiomyosarcoma. Both the patient’s biopsy report and the surgical pathology report revealed similar negative findings (desmin, cytokeratin AE1/AE3, p63, SOX10) as well as similar positive findings (smooth muscle actin and CD68). Critical distinctions that led to a change in diagnosis from atypical fibroxanthoma to leiomyosarcoma emerged during the final pathological analysis, which revealed more widespread positive staining for smooth muscle actin and muscle-specific actin throughout the surgical specimen along with detailed cell and nucleus morphology of atypical spindle cells in the dermis and subcutis. This valuable information was not available during the initial biopsy when the lesion was smaller. It is possible that earlier diagnosis of primary leiomyosarcoma could have resulted in advanced pre-operative treatment and excision of the facial lesion, preventing involvement of surrounding areas such as the patient’s left eye, ear, and facial nerve.
Keywords
Leiomyosarcoma, atypical fibroxanthoma, facial reconstruction, immunochemistry
Introduction
Soft tissue sarcomas (STS’s) are relatively rare neoplasms that arise for mesenchymal origin that generally make up less than 2% of all adult malignant neoplasms [1]. The diagnostic guidelines for soft tissue sarcomas are extremely wide reaching and variable; this quality is likely due to the ability of mesenchymal cells to differentiate into a number of different tissue types, like muscle, fat, connective tissue, and bone. This quality of STS’s is reflected in relative ambiguity in clinical practice of diagnosing between different types of STS’s, especially when differentiating between benign and malignant behavior of tumors. In specific, atypical fibroxanthoma is a form of a benign soft tissue tumor that is often confused with malignant forms of similar tumors such as pleomorphic dermal sarcomas and leiomyosarcomas, all of which share similar staining markers as well as the cell morphology of atypical spindle cells with mitotic figures. Immunohistochemical staining is crucial in guiding diagnosis to origin of the tumor, however, it is debatable to say whether staining itself is helpful in aiding the differentiation from benign and malignant potential [2].
Current literature suggests that observations on size, growth, and behavior of the tumor such as depth invasion can be used to assess malignant potential of STS’s, however, clear clinical guidelines in such qualities are still lacking in the ability to reach proper diagnosis as the biology of these tumors can vary widely. This leaves a large amount of room for misdiagnosis of STS’s, which is especially dangerous in tumors that are similar in embryonic origin but differ in malignant potential. Here, we report a case of a 70 year old caucasian male who presents with a left facial soft tissue tumor initially diagnosed as an atypical fibroxanthoma later revealed to be a primary leiomyosarcoma upon excision and pathological analysis.
Case Presentation
Our case report presents a 70-year-old caucasian male with past medical history of hypertension, atrial fibrillation on pradaxa, basal cell carcinoma, and significant refractive visual impairment who initially presented to our department with an ulcerating mass on the left side of the face. He first presented to a local skin care clinic for a pruritic, intermittently bleeding left superior malar cheek lesion that has been present for several months. He was then referred to a tertiary care center but due to a delay in care for unknown reasons, eventually referred to our Department of Surgical Oncology.
The patient had biopsies performed on the lesions roughly 3 months prior to the initial consultation visit with our Department of Surgical Oncology. Immunohistochemical stain with appropriate controls demonstrated tumor cells positive for vimentin, patchy for CD68, SMA, and lesional cells positive for factor XIIIa. Stains were negative for desmin, AE1- AE3 keratin, Melan-A, SOX10, CD10, and p63. At the time of this biopsy, the lesion measured 2 cm anterior to the ear on the left superior lateral malar cheek. The results of this biopsy led to the diagnosis of the atypical fibroxanthoma at this time.
Computed tomography (CT) of the chest, magnetic resonance imaging (MRI) of the face and neck, as well as positron emission tomography (PET) scan were performed roughly 1 month before the excisional operation. CT scan demonstrated a branching subsegmental endobronchial pulmonary nodule in the left upper lobe measuring 1.8 cm in craniocaudal dimension, which could be due to endobronchial impaction. MRI revealed a moderate sized soft tissue mass superficial to the left zygoma with mild superficial soft tissue edema and no obvious adjacent fractures. There is a thin fat plane between the zygoma and mass without soft tissue infiltration. PET CT scan showed the facial neoplasm to be hypermetabolic without distant metastasis or adenopathy at this time.
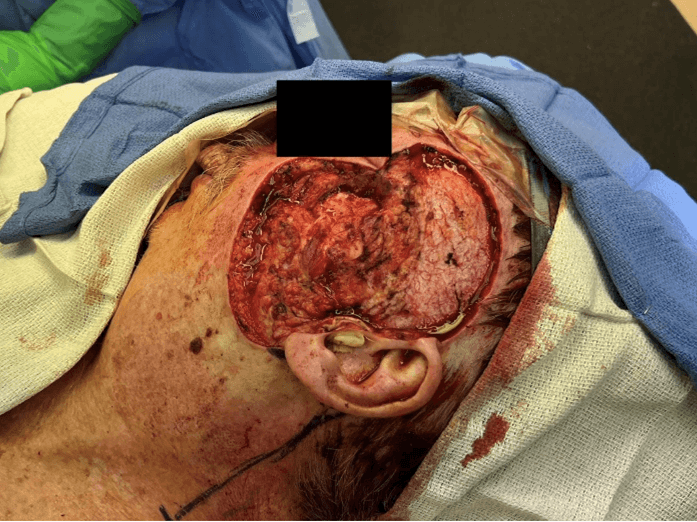
Final preoperative measurements revealed an 11 × 11 cm exophytic mass at the left malar cheek overlying the zygoma, just medial to the ear, with the superior aspect 1 cm lateral to the lateral canthus of the eye as shown in (Figure 1) below. Central necrosis of the lesion was noted along with relative immobility to underlying tissue of the lesion. The patient underwent a wide excision of the left face with 1 cm margin. Intraoperatively, excision of the mass was difficult due to firm adhesions of the neoplastic tissue to normal tissue and the inability to differentiate neoplastic tissue from fascia, muscle, and bone. Once the neoplasm was excised, it was promptly sent to pathology for further analysis.
Figure 1: Final Presentation of the left facial mass pre-operatively. 11 × 11 cm exophytic lesion at the left malar cheek overlying the zygoma, just medial to the ear, with the superior aspect 1 cm lateral to the lateral canthus of the eye.
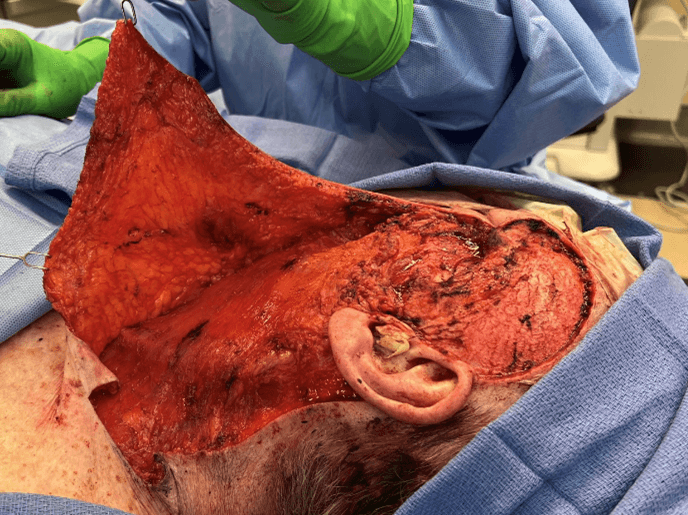
The defect size measured 16.5 × 9.5 × 1 cm involving the left lower eyelid, left cheek, left temporal, left tragus and periauricular area as well as depicted in (Figure 2). The patient subsequently underwent a cervical facial flap lift, full thickness skin graft of the left upper cheek, anterior temple, and lower eyelid area with donor site from the left arm as well as complex closure of the arm.
The closure of the defect involved a cervical skin flap dissection raised from the left cheek down inferiorly to the clavicular portion of the neck measuring 17 × 13 cm. Z-plasty technique was utilized in the lower neck measuring 4 × 4 cm. A full thickness skin graft was harvested from the left arm measuring 10.5 × 5.5 cm in dimension, which was grafted into the left temporal involving the left lower eyelid as shown in (Figures 3 & 4).
Figure 2: Intraoperative defect after wide excision of the patient’s lesion. 16.5 × 9.5 × 1 cm post-excisional defect prior to immediate facial reconstruction.
Figure 3: Cervical facial skin flap dissection from the left cheek down inferiorly to the clavicular portion of the neck measuring 17 × 13 cm with intention to reduce initial defect size through rhytidectomy of the dissected skin.
Figure 4: Patient after facial reconstruction operation following wide excision of facial mass. Full thickness skin graft measuring 10.5 × 5.5 cm transplanted into the left temporal area following rhytidectomy with the dissected cervical facial skin flap.
Expected Treatment Outcomes
It was expected that the patient would no longer have nerve connection to the sensation and motor control of the left side of the face in general, due to the proximity to the left mastoid process and facial nerve. Involvement of the left lower eye during excision posed risk of vision loss in the corresponding eye, however, as noted in the initial history and physical examination, this patient already has significant refractive visual impairment– this posed a nonsignificant impact to the patient’s visual function.
Facial skin reconstruction measures were expected to heal appropriately without significant strain restriction to the skin that was reconstructed and grafted on the left side of the face. Postoperative external beam radiation to the area and possible adjuvant chemotherapy were expected to be optimal treatment to restrict the growth of any cancerous tissue not excised, as well as shrink and destroy remaining neoplastic tissue. As PET scan was discussed earlier, no metastatic disease was demonstrated in this patient, thus, this post-operative treatment plan was expected to be sufficient for the patient’s continued recovery.
Actual Treatment Outcomes
Updated post-operative pathology reports of the excised mass were received with the new diagnosis of the patient’s mass as a primary leiomyosarcoma. The patient’s post-excisional pathology report of the facial mass demonstrated dense proliferation of atypical spindled cells occupying the dermis and extending into the subcutis. The lesional cells demonstrate many cigar-shaped nuclei with blunted ends. The nuclei were enlarged and nuclear pleomorphism was seen. Mitotic figures were readily observed in these sections. Smooth muscle actin and muscle specific actin stains performed are diffusely positive, while desmin and caldesmon stains are negative. CD10 stains and CD68 stains demonstrated focal areas of positivity. p63, cytokeratin AE1/AE3, SOX10, S100, and CD34 stains were negative. These findings were felt to be most consistent with those of a leiomyosarcoma.
At the patient’s one month follow up appointment, the patient’s full thickness skin grafts and surgical site was noted to be healing well without any major complications as depicted in (Figure 5) below. No further surgical intervention was needed. All clinical and pathological details and reports indicate a final diagnosis of facial leiomyosarcoma; mitotic count 8/mm2, grade 3; pathological stage IIIB (pT4aN0M0). The patient was subsequently scheduled for clearance in order to undergo a course of external beam radiation to the left malar and zygoma area. At this visit, the patient elected not to undergo adjuvant chemotherapy given his age and current comorbidities.
Figure 5: 11 weeks post-operative follow-up showing healing cervicofacial flap with full thickness skin-graft with external beam radiation therapy.
Discussion
This case demonstrated an interesting ambiguity between the clinical and pathological diagnosis of cutaneous and soft tissue tumors like primary leiomyosarcoma. This was a unique case of a smooth muscle tumor that primarily arises in the alimentary tract, uterus, and retroperitoneum occurring cutaneously on the head and neck area.
Less than 4% of all leiomyosarcoma cases occur in head and neck region [3]. This quality of the neoplasm is likely a factor that contributed to the low suspicion of the diagnosis upon initial presentation of the patient’s lesion. In addition, one of the most common presentations of a primary leiomyosarcoma is in the uterus; which further points to the unique quality of this neoplasm arising in our specific patient, a 70 year old caucasian male. As discussed in the case history, the patient’s initial biopsy of the lesion at its smaller size originally resulted in a diagnosis of atypical fibroxanthoma. Wide excision of the lesion at its final largest size resulted in a diagnosis of primary leiomyosarcoma.
Immunochemical staining is known to be crucial in diagnosing ambiguous neoplasms, such as an atypical fibroxanthoma. However, in this case, immunochemical staining was extraordinarily similar between the initial diagnosis of atypical fibroxanthoma and final diagnosis of primary leiomyosarcoma with the exception of more diffusely positive stainings in regards to leiomyosarcoma.
To elaborate, pathology report staining for both atypical fibroxanthoma and leiomyosarcoma both demonstrated similar negative findings discussed in the history (desmin, cytokeratin AE1/AE3, p63, SOX10); as well as similar positive findings for smooth muscle actin and CD68.
The main distinctions that made the diagnosis from atypical fibroxanthoma and leiomyosarcoma lies in the later excision of the mass being more diffusely positive for smooth muscle actin and muscle specific actin stains throughout the sample. In addition, the larger, surgical excision of the mass offered the ability to observe cell and nucleus morphology of atypical spindle cells in the dermis and subcutis; a quality that was not available for the initial biopsy of the lesion at its earlier size in regards to initial diagnosis. It is indicated in this case that the growth in size from initial presentation to final excision offered a means of proper diagnosis of the neoplasm; however growth of the mass comes at the cost of mortality and survival rate of the patient. Staining markers can be useful in ruling in and out malignant origins, however, improvements for more specific and strict clinical and immunochemical guidelines must be made as malignant neoplasms can have similar staining characteristics [4].
In addition, this case demonstrates the need for close follow up and high suspicion for malignancy in initial lesions as well. Atypical fibroxanthoma diagnoses are also largely based on clinically benign behavior, especially under 4 cm in dimension; a dangerous assumption for a neoplasm that truly is malignant in origin as in our patient’s case due to risk of metastases and invasion if untreated [5].
The treatment of atypical fibroxanthoma in its generally benign behavior involves Moh’s surgery (wide local excision) with adjuvant radiation to treat recurrence and any nonexcised neoplasm. Treatment for leiomyosarcoma, with its more malignant nature, often requires strict pretreatment evaluation along with possible initiation of neoadjuvant chemotherapy along with surgical excision, and subsequent strict treatment response monitoring with continued chemotherapy and radiation as needed. It is possible that earlier diagnosis of primary leiomyosarcoma made sooner could have resulted in earlier and more aggressive excision of the facial lesion, preventing involvement and tissue invasion of surrounding areas such as the patient’s left eye, ear, and facial nerve involvement.
In regards to the final diagnosis of the patient’s mass as a primary leiomyosarcoma, general data shows that the 5 year survival rate for primary localized leiomyosarcoma is roughly 50%, with individuals aged under 60 years showing a better outlook on survival.
More specifically, general data showed a 40% survival rate for patients with primary leiomyosarcoma of the trunk/axial portion of the body [6]. Being that our specific patient is 70 years old with the mass on the face of the body, survival rate was interpreted to be more towards the 40% group of individuals. It is important to add that there is not consistent general data that discusses the survival rate of leiomyosarcomas on the facial area of the body specifically. Although our specific patient did not experience evident metastatic disease on diagnostic studies, metastases soft tissue tumors such as leiomyosarcoma may drop five year survival rate down to 15 to 25% [6].
In summary, current literature suggests that high clinical uncertainty exists in differentiating diagnosis of soft tissue tumors. In regards to pathological analysis to reach a diagnosis, immunohistochemical staining is not enough to provide evidence between benign and malignant causes. Improvements in clinical suspicion, tissue analysis, and pre-treatment evaluation is necessary in order to provide necessary treatment modes aggressive enough to prevent complications of misdiagnosed tumors of malignant origins.
Article Info
Article Type
Case ReportPublication history
Received: Fri 22, Dec 2023Accepted: Tue 23, Jan 2024
Published: Tue 06, Feb 2024
Copyright
© 2023 Emily Tran. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2023.04.03
Author Info
Emily Tran Jasmine J. Park Nandini N. Kulkarni Vinay S. Gundlapalli
Corresponding Author
Emily TranRowan-Virtua School of Osteopathic Medicine, Stratford, New Jersey, USA
Figures & Tables



References
1. Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. CA Cancer J Clin 73: 17-48. [Crossref]
2. Čierna Z, Trška
R (2019) Atypical fibroxanthoma, rare and often unrecognized cutaneous soft
tissue tumor - a case report and review of the literature. Cesk Patol
55: 182-186. [Crossref]
3. Jafarian M, Azizi S
(2022) Leiomyosarcoma of the Maxilla: A Case Report and Literature Review. J Dent (Shiraz)
23: 244-250. [Crossref]
4. Deneve JL, Messina
JL, Bui MM, Marzban SS, Letson GD et al. (2013) Cutaneous leiomyosarcoma:
treatment and outcomes with a standardized margin of resection. Cancer
Control 20: 307-312. [Crossref]
5. Alvegard TA, Berg NO, Baldetorp B, Ferno M, Killander et al. (1990) Cellular DNA content and prognosis of high-grade soft tissue sarcoma: the Scandinavian Sarcoma Group experience. J Clin Oncol 8: 538-547. [Crossref]
6. Gaillard S, Secord AA (2023) Staging, treatment, and prognosis of endometrial stromal sarcoma and related tumors and uterine adenosarcoma. In: Chakrabarti A and Vora SR, eds. UpToDate.
