Long-term Outcome of Surgical Reconstruction of the Interosseous Membrane after Chronic Essex-Lopresti Injury
A B S T R A C T
An Essex-Lopresti injury (ELI) is a rare lesion that describes an interosseous membrane (IOM) disruption associated with dislocation of the distal radio-ulnar joint (DRUJ) and radial head fracture. They are rare and have a tendency to be underdiagnosed in the ER, so it is not uncommon to see chronic cases. As part of the treatment options different IOM reconstructions have been proposed along with associated procedures to the radial head and DRUJ. One of the most effective treatment strategies has been the use of a bone-tendon-bone (BTB) patellar graft for IOM reconstruction with promising outcomes. We present a case of 46-year-old man who suffered an Essex-Lopresti injury with a radial head fracture and associated posterolateral elbow instability that was managed initially non-operatively. After failure for continued pain and instability if the elbow and forearm, we treated the patient with a radial head arthroplasty, ligament reconstruction of the posterolateral complex, and DRUJ ligament reconstruction with extensor hallucis tendon without a formal IOM. This operation was successful initially, but continued forearm instability contributed to failure of the RHA and DRUJ reconstruction. A second operation was performed resecting the loosened radial head arthroplasty, performing an ulnar shortening osteotomy, and an IOM reconstruction with BTB allograft. After eight years of follow-up the patient is very satisfied with the procedure and rates his elbow as almost normal. ELI are rare and represent a severe injury of the forearm with axial and transverse instability, leading to severe symptoms and instability of the forearm. Initial diagnosis is challenging, and acute treatment yields better results than chronic cases. IOM reconstruction seems to be necessary in the setting of chronic reconstructions, along with other procedures to balance the forearm. We review different IOM grafting options and associated procedures for the treatment of these challenging injuries.
Keywords
Essex-lopresti, longitudinal instability, forearm, IOM, graft, ulnar shortening osteotomy
Introduction
An Essex-Lopresti injury (ELI) is a rare lesion that describes an interosseous membrane (IOM) disruption associated with dislocation of the distal radio-ulnar joint (DRUJ) and radial head fracture. Reported case studies suggest an incidence of 1% of all radial head fractures, but only 25% of patients are correctly diagnosed acutely [1]. Timely diagnosis is critical as it has been shown to affect results adversely [2, 3]. Additionally, authors may report the diagnosis through different names, and not all cases with longitudinal instability of the forearm might be full-blown Essex-Lopresti injuries [4].
In a cadaver study using an axial load and ultrafast cameras, some authors have suggested that the Interosseous membrane (IOM) is the first structure to rupture followed by the radial head and the DRUJ. Still, it is unclear this is the sole way of reproducing this injury [5]. However, when presented with an isolated radial head fracture, the forearm and the DRUJ must be explored thoroughly. Pain at the forearm or at the wrist mandates comparative exploration of the DRUJ and the use of comparative x-ray evaluation. If acute longitudinal instability is suspected or pain during palpation of the DRUJ is found, specific projections can help diagnose the DRUJ associated instability. Advanced imaging modalities such as US or MRI are helpful to detect these injuries [6].
Chronic injuries show worse clinical results, and different IOM reconstructions have been proposed using different tissues (allograft, autograft, synthetic grafts), different fixation techniques (buttons, screws, or sutures) and the need for associated procedures [7]. One of the most effective treatment strategies has been the use of a bone–tendon-bone (BTB) patellar graft for IOM reconstruction with promising outcomes in the stabilization of the forearm, increasing function, and decreasing pain to the forearm and wrist in patients with chronic radioulnar dissociation [2].
Dr. Essex-Lopresti already made a clear case not to excise the radial head or reconstruct it with a radial head prosthesis in case of acute longitudinal instability, and this concept has been proved the test of time [8]. The need to perform an associated procedure to the wrist and radial head is subject to debate, but most chronic cases will benefit from an ulnar shortening osteotomy. Achieving the proper length of the forearm is intuitive and associating a radial head replacement to an ulnar shortening osteotomy and an interosseous membrane reconstruction are treatments directed towards that aim. Albeit, with the available evidence, there is not a clear consensus in which treatment option is superior [2, 9, 10].
Material and Method
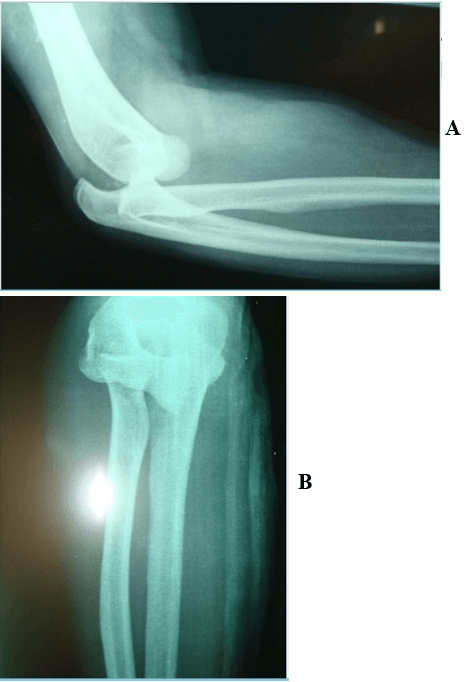
We present a 46-year-old patient that suffered a fall from its height and suffered a fracture-dislocation of the left elbow in 2007 that was treated with closed reduction and immobilization with a posterior slab for 12 days (Figure 1A & 1B). At follow-up, he was diagnosed with a radial head fracture and an epitrochlear fracture.
Figure 1: Radiographs of the initial injury after a fall on the outstretched hand showing an elbow dislocation with a radial head fracture.
After cast removal, the patient remained symptomatic, and elbow and wrist ultrasounds were performed a month later informing of partial avulsion of the common extensor tendon, triangular fibrocartilage (TFC) rupture, radial head fracture, and lateral condyle fracture. An MRI was made four months later (5 months postinjury), showing persistent elbow instability with a radial head fracture with intraarticular fragments. After this study, the patient came to our clinic, showing pain in the elbow and wrist associated with decreased ROM of the wrist, elbow, and forearm that precluded carrying a normal life.
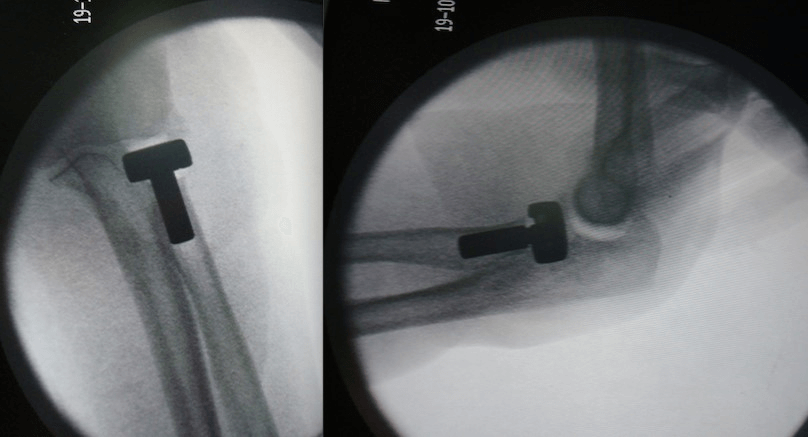
Clinically, the patient showed marked elbow stiffness and signs of forearm instability. The patient consented for radial head arthroplasty, ligament reconstruction of the posterolateral complex, and DRUJ ligament reconstruction with extensor hallucis tendon without a formal IOM reconstruction (Figure 2). During the operation, a radius pull test was performed, evidencing a longitudinal instability of the forearm (Figure 3) [11]. At that point, we considered it sufficient to regain the forearm's length with the radial head arthroplasty and stability by reconstructing the distal and proximal buttresses of the forearm. The patient was immobilized for three weeks in neutral rotation of the forearm, after which he began physical therapy.
Figure 2: Intraoperative images showing the radial head arthroplasty and a concentric elbow reduction.
Figure 3: Intraoperative images showing a positive radius pull test. The DRUJ was stabilized with a reconstruction using an extensor hallucis longus autograft.
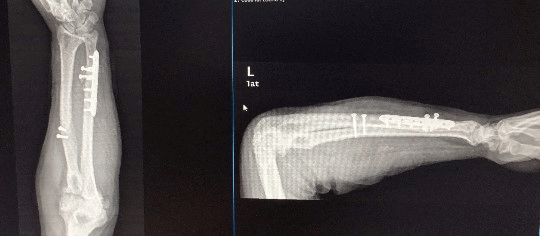
At three months postoperatively, the patient had persistent pain in the elbow and wrist, with mild ulnohumeral subluxation and early signs of loosening of the radial head arthroplasty on radiographs, suggesting a failure to stabilize the forearm. As the radial head loosened, the distal radius migrated proximally with progressive failure of the distal graft. A second operation was then performed resecting the shifted radial head arthroplasty, performing an ulnar shortening osteotomy with temporary pinning of the DRUJ, and a forearm reconstruction. The allograft was passed through the ulnar incision under the extensor muscles and fixed proximally with two small fragment screws through a separate dorsal incision on the proximal forearm (Figure 4).
Figure 4: Ulnar shortening fixed with a dedicated ulnar plate and a K-wire for temporary fixation.
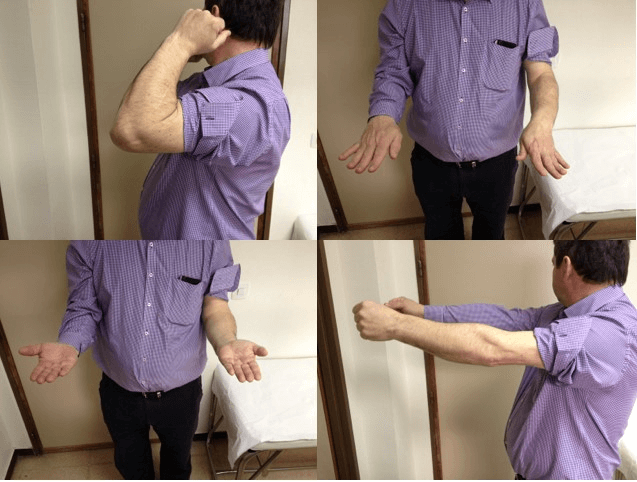
The patient improved dramatically after this operation, resolving any wrist and elbow pain. Over the years, the radius has shifted a few millimeters proximally without any clinical consequence. After eight years of follow-up, our patient continued to show good elbow, wrist, and forearm range of motion with no work limitations and considered his elbow to be almost normal (Figures 5 & 6).
Figure 5: Final radiographic result of surgery after 8 years. During the initial stages there was a mild increase in ulnar variance that stabilized over time.
Figure 6: Patients ROM after 8 years of surgery. The patient is very satisfied with the outcome of his elbow and wrist and rates his elbow as almost normal and performs heavy duties in his job with no restriction.
Conclusion
Essex-Lopresti injuries are rare and represent a severe injury of the forearm with axial and transverse instability [4, 12]. Sadly, they are often not recognized acutely in the emergency room, and there is evidence that these injuries are best treated early.
Pain extending to the forearm or wrist pain in the context of a radial head fracture should raise suspicion to the event of this injury, especially when there is radiographic evidence of slight proximal migration. It might be challenging to obtain stress views of the wrist in the acute setting due to pain. Comparative wrist x-rays can be helpful, but proximal migration of radius and disruption of the DRUJ might not be observed in the acute setting. When in doubt, there is a special projection defined by Epner to image the DRUJ. With the patient's shoulder abducted to 90° and the elbow flexed to 90° with the forearm in a neutral position a dorso-palmar x-ray projection must be made in pronation under full-grip to identify dynamic instability [13].
If there is a suspicion of an injury to the IOM, performing an US of the forearm is a fast, accessible test to diagnose acute ruptures [6, 14]. There are some instances where the US can be negative, and an MRI can be obtained. In the setting of trauma, MR of the forearm has shown a positive predictive value of 100%, a negative predictive value of 89%, a sensitivity of 87.5% and a specificity of 100%, in comparison to dissection findings [15]. Fester et al. studied in 19 cadavers the comparative values for diagnosis of the IOM and concluded that both MR and US were valid methods for the determination of IOM injuries. MRI showed a 96% accuracy rate, 93% sensitivity, 100% specificity, 100% positive predictive value, and 93% negative predictive value while US showed a 94% accuracy rate, 100% sensitivity, 89% specificity, 94% positive predictive value, and 100% negative predictive value [16].
Gaspar et al. reported a retrospective series of 33 patients, who, since 1992, have been treated with patellar BTB reconstruction (auto and allograft) with an ulnar shortening osteotomy for IOM chronic injuries after a failed initial management [2]. The study includes different presentations, but all cases included a fracture to the radial head or neck, except one case with a fracture of both forearm bones. Most of the patients underwent at least one previous operation (mean 1.7 operations, ranging from 1 to 7). Previous operations consisted mainly in radial head excision in 16 cases (1 partial), radial head replacement (13 cases, one of them with silastic and another with bony reconstruction), elbow debridement in 7 cases, radial head ORIF in 4 cases, lateral ligament reconstruction in 3 cases (1 revision procedure), TFCC repair in 2 cases, TFCC debridement in 2 cases, ulnar shortening osteotomy in 2 cases and HO excision and elbow capsulectomy in 1 case. At a mean follow up of 10 years, patients showed improved PROMS with a final QuickDASH of 29.8, a modified Mayor Wrist score (MMW) of 82.7, and a Broberg-Morrey score of 91.6. Radiographically, patients improved the ulnar variance but, over time, lost a mean of 1.1 mm of ulnar variance. Eleven patients suffered a complication (33%) mostly related to nonunion or hardware-related problems of the ulnar shortening osteotomy.
In the study, two patients underwent a radial head arthroplasty resection, one Silastic, and one metallic, like in our clinical case. None of these patients underwent subsequent complications or revisions. This information adds to the initial positive experience with this technique published initially by Marcotte and Osterman [10]. Regarding the need for radial head reconstruction, Trousdale et al. published significant rates of improvement in wrist and elbow with an improvement of ROM and clinical subjective scales using a radial head prosthesis and other authors have reported good results with the use of a radial head arthroplasty without formal reconstruction of the IOM [9, 17]. Szabo et al. also described a marked improvement of wrist pain, ROM, and forearm rotation after using radial head frozen allograft in 5 cases. However, forearm length was achieved previously on three cases with the use of an Ilizarov frame [18]. While we believe a radial head, replacement adds to the stability of the forearm, in our case damage to the proximal radius after loosening of the primary RH arthroplasty precluded the reliable use of a revision arthroplasty. The limited available evidence suggests that satisfactory results can be achieved by IOM reconstruction without the use of a RH arthroplasty [2, 19].
There are multiple graft options for reconstructing the IOM that include the semitendinosus, the pronator teres, the flexor digitorum superficialis tendon, a folded fascia lata graft, or a synthetic graft [3, 20-25]. The stiffer construct, however, is achieved with the use of a BTB patellar graft. Regarding the type of reconstruction, we favored the use of a BTB patellar allograft, reproducing the experience of other authors [2, 10]. These authors reported the initial use of autograft that they discontinued due to donor site morbidity during the study. While the allograft showed increased ulnar variance, the clinical results were not adversely affected. Likewise, our patient has shown a loss of initial ulnar variance, but the clinical result has not been affected. Other authors have used synthetic grafts with good initial outcomes, mostly for acute injuries, but long-term studies are warranted [26]. It seems that IOM reconstruction is critical, and it might become especially important in cases of RH resection or RH arthroplasty excision. We do not know, however, if the initial relief is obtained by the ulnar shortening osteotomy or the BTB allograft reconstruction, but we believe that proximal migration in the absence of a radial head arthroplasty would have progressed have the IOM reconstruction not been functional. Our findings are consistent with the results of Marcotte and Gaspar that rebalancing the forearm and containing the proximal migration seems to work effectively after long-term follow up [2, 10].
Article Info
Article Type
Research ArticlePublication history
Received: Mon 20, Jul 2020Accepted: Thu 06, Aug 2020
Published: Mon 31, Aug 2020
Copyright
© 2023 Raul Barco. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.02.03
Author Info
Minotta Quebradas MJ Antuña SA Raul Barco
Corresponding Author
Raul BarcoUpper Limb Unit, Department of Orthopedics, Hospital Universitario La Paz, Madrid, Spain
Figures & Tables


References
- Descamps J, Costil V, Apard T (2020) Ultrasound-guided transection of the interosseous membrane of the forearm. Hand Surg Rehabil 39: 167-170. [Crossref]
- Gaspar MP, Adams JE, Zohn RC, Jacoby SM, Culp RW et al. (2018) Late Reconstruction of the Interosseous Membrane with Bone-Patellar Tendon-Bone Graft for Chronic Essex-Lopresti Injuries: Outcomes with a Mean Follow-up of Over 10 Years. J Bone Joint Surg Am 100: 416-427. [Crossref]
- Bigazzi P, Marenghi L, Biondi M, Zucchini M, Ceruso M (2017) Surgical Treatment of Chronic Essex-Lopresti Lesion: Interosseous Membrane Reconstruction and Radial Head Prosthesis. Tech Hand Up Extrem Surg 21: 2-7. [Crossref]
- Wegmann K, Dargel J, Burkhart KJ, Brüggemann GP, Müller LP (2012) The Essex-Lopresti lesion. Strategies Trauma Limb Reconstr 7: 131-139. [Crossref]
- Liu Y, Zhang Y (2014) Sequence of the Essex-Lopresti lesion--a high-speed video documentation and kinematic analysis. Acta Orthop 85: 545. [Crossref]
- Rodriguez Martin J, Pretell Mazzini J (2011) The role of ultrasound and magnetic resonance imaging in the evaluation of the forearm interosseous membrane. A review. Skeletal Radiol 40: 1515-1522. [Crossref]
- Artiaco S, Fusini F, Colzani G, Massè A, Battiston B (2019) Chronic Essex-Lopresti injury: a systematic review of current treatment options. Int Orthop 43: 1413-1420. [Crossref]
- Loeffler BJ, Green JB, Zelouf DS (2014) Forearm instability. J Hand Surg Am 39: 156-167. [Crossref]
- Venouziou AI, Papatheodorou LK, Weiser RW, Sotereanos DG (2014) Chronic Essex-Lopresti injuries: an alternative treatment method. J Shoulder Elbow Surg 23: 861-866. [Crossref]
- Marcotte AL, Osterman AL (2007) Longitudinal radioulnar dissociation: identification and treatment of acute and chronic injuries. Hand Clin 23: 195-208. [Crossref]
- Smith AM, Urbanosky LR, Castle JA, Rushing JT, Ruch DS (2002) Radius pull test: predictor of longitudinal forearm instability. J Bone Joint Surg Am 84: 1970-1976. [Crossref]
- Orbay JL, Mijares MR, Berriz CG (2016) The transverse force experienced by the radial head during axial loading of the forearm: A cadaveric study. Clin Biomech (Bristol, Avon) 31: 117-122. [Crossref]
- Epner RA, Bowers WH, Guilford WB (1982) Ulnar Variance--The Effect of Wrist Positioning and Roentgen Filming Technique. J Hand Surg Am 7: 298-305. [Crossref]
- Failla JM, Jacobson J, van Holsbeeck M (1999) Ultrasound diagnosis and surgical pathology of the torn interosseous membrane in forearm fractures/dislocations. J Hand Surg Am 24: 257-266. [Crossref]
- McGinley JC, Gold G, Cheung E, Yao J (2014) MRI detection of forearm soft tissue injuries with radial head fractures. Hand (N Y) 9: 87-92. [Crossref]
- Fester EW, Murray PM, Sanders TG, Ingari JV, Leyendecker J et al. (2002) The efficacy of magnetic resonance imaging and ultrasound in detecting disruptions of the forearm interosseous membrane: a cadaver study. J Hand Surg Am 27: 418-424. [Crossref]
- Trousdale RJ, Amadio PC, Cooney WP, Morrey BF (1992) Radio-ulnar dissociation. A review of twenty cases. J Bone Joint Surg Am 74: 1486-1497. [Crossref]
- Szabo RM, Hotchkiss RN, Slater RR Jr (1997) The use of frozen-allograft radial head replacement for treatment of established symptomatic proximal translation of the radius: preliminary experience in five cases. J Hand Surg Am 22: 269-278. [Crossref]
- Verhiel S, Özkan S, Langhammer CG, Chen NC (2020) The Serially-Operated Essex-Lopresti Injury: Long-Term Outcomes in a Retrospective Cohort. J Hand Microsurg 12: 47-55. [Crossref]
- Oberlin C, Belkheyar Z, Soubeyrand M, Welby F, Degeorges R (2006) Semitendinosus ligamentoplasty of the forearm interosseous membrane in a case of Essex-Lopresti syndrome. Eur J Orthop Surg Traumatol 16: 164-168. [Crossref]
- Soubeyrand M, Oberlin C, Dumontier C, Belkheyar Z, Lafont C et al. (2006) Ligamentoplasty of the forearm interosseous membrane using the semitendinosus tendon: anatomical study and surgical procedure. Surg Radiol Anat 28: 300-307. [Crossref]
- Chloros GD, Wiesler ER, Stabile KJ, Papadonikolakis A, Ruch DS et al. (2008) Reconstruction of essex-lopresti injury of the forearm: technical note. J Hand Surg Am 33: 124-130. [Crossref]
- Nunez FA Jr, Evans PJ (2018) Chronic Longitudinal Instability of the Forearm Treated With a Combination of Ulnar Shortening Osteotomy, Pronator Teres Transfer, and Tightrope Technique. Tech Hand Up Extrem Surg 22: 99-103. [Crossref]
- Smith NC, Sivakumar BS, Tremblay DM, Bellity JP, Lawson RD (2019) Interosseous Membrane Reconstruction Utilizing Flexor Digitorum Superficialis Autograft. Tech Hand Up Extrem Surg 23: 122-127. [Crossref]
- Sabo MT, Watts AC (2012) Reconstructing the interosseous membrane: a technique using synthetic graft and endobuttons. Tech Hand Up Extrem Surg 16: 187-193. [Crossref]
- Gaspar MP, Kearns KA, Culp RW, Osterman AL, Kane PM (2018) Single- versus double-bundle suture button reconstruction of the forearm interosseous membrane for the chronic Essex-Lopresti lesion. Eur J Orthop Surg Traumatol 28: 409-413. [Crossref]
