Journals
Lumbar discectomy: should patient body mass index and abdominal girth be considered when selecting cases suitable for training opportunities?
A B S T R A C T
Study Design:
Prospective observational study.
Objectives:
To determine whether body mass index (BMI) and abdominal girth are reliable predictors of wound depth and operative duration at lumbar discectomy, to compare the duration of trainee- and consultant-performed cases, and to assess the role of patient body habitus when selecting cases for training opportunities.
Methods:
Pre-operative height and weight, abdominal girth in knee-chest position, and intra-operative wound measurements were taken. Operative duration was recorded using theatre management software. Patients undergoing single-level lumbar discectomy were selected, n=29, M:F ratio 18:11. Mean age was 47.2 years (range 18-83). Discectomy level: L2/3 (1); L3/4 (1), L4/5 (18); L5/S1 (9).
Results:
Mean BMI was 30.4kg/m2 (19.7-47.2), abdominal girth 106cm (48-154), wound length 5.4cm (4.5-6.5), subcutaneous fat depth 1.9cm (0.5-5.2), muscle depth 3.2cm (2.0-4.2), total wound depth 5.0cm (3.5-9.0), operation duration 47 minutes (24-82). Fifteen patients were clinically obese (BMI >30 kg/m2). Fifteen cases were trainee-performed and fourteen consultant-performed. Mean trainee operative duration was 50 minutes (24-77). Mean consultant operative duration was 45 minutes (24-82). Of the cases with BMI >30kg/m2, eight were trainee-performed and seven consultant-performed. Subcutaneous fat depth, muscle depth and total wound depth were associated with increased operative duration. BMI, abdominal girth, discectomy level and trainee-performed cases were not significantly associated with increased operative duration.
Conclusions:
Over half of the study patients were clinically obese. BMI and abdominal girth are not reliable predictors of operative difficulty as measured by operative duration. Lumbar discectomy in obese individuals is an appropriate training case.
K E Y W O R D S
Lumbar discectomy, surgical training, obesity, body mass index, abdominal girth, learning curve
Acronyms and abbreviations
BMI - body mass index, kg/m2 - kilograms per metre squared, SE - standard error, cm - centimetres
I N T R O D U C T I O N
An increasing proportion of the world’s population are projected to suffer obesity and related diseases in coming decades. The majority of prolapsed lumbar discs can be managed non-operatively with success. For those requiring surgery, the next generation of spine surgeons must possess the surgical skills to treat high BMI individuals. Regarding the prolapsed intervertebral disc with associated sciatic nerve symptoms, surgery remains an established option for failed conservative treatment.
Body mass often requires adaptations of patient positioning and anaesthetic technique [1]. Higher complication rates after lumbar spine fusion in obese individuals have been observed [2]. In one single-surgeon study of lumbar microdiscectomy in 75 patients, eight recurrences of herniated nucleus pulposus occurred. Among the 25 individuals with BMI >30kg/m2, the odds of recurrence were 12 times greater than their non-obese counterparts [3]. Some surgeons may conclude that lumbar discectomy is more technically demanding in high BMI individuals.
Duration of surgery has been used as a marker for technical difficulty, or unfamiliarity with the procedure. In the learning curve for lumbar micro endoscopic discectomy, the average operation duration reduces until approximately 20 cases [4]. Minimising operative duration remains crucial to managing theatre resources and lowering infection rates. Consequently, trainees may be directed towards non-obese patients as training cases. However, modern surgical instruments allow access to the lumbar disc at various wound depths while minimising soft tissue disruption. With regards to body mass index and body habitus, neither duration of surgery in lumbar discectomy, nor patient selection for training cases, have been examined.
Methods
A prospective observational study of elective primary lumbar discectomies was performed at two institutions by a single Consultant Orthopaedic Spine Surgeon (NWAE) and Specialty Registrar (CKJO). Pre-operative height and weight, abdominal girth in knee-chest position, and intra-operative wound measurements were taken. Operative duration was recorded using theatre management software.
All cases were performed during one six-month training rotation in orthopaedic spine surgery. Twenty-nine patients undergoing single-level lumbar discectomy were selected were selected, n=29, M:F ratio 18:11. Mean age was 47.2 years (range 18-83). The discectomy level was L4/5 in 18 cases, L5/S1 in 9 cases, with one case each at L2/3 and L3/4. BMI was calculated using pre-operative height and weight measurements. Patient positioning was standard knee-chest: prone with hips and knees flexed, and a vertical support against the buttocks and ischial tuberosities. The maximum abdominal girth was measured after induction of general anaesthesia, with the patient in the knee-chest position.
All cases underwent pre-operative image intensifier identification of spinal level, and pre-operative surgical incision skin marking. A standard minidiscectomy was performed in all cases. McCulloch or Caspar wound retractors were utilised. Wound depth, subcutaneous fat depth, and muscle depth were measured intra-operatively using a flexible sterile disposable ruler placed vertically in the wound. The deepest portion of the vertebral lamina was used as the base of the wound. Operative duration was recorded as the time from knife-to-skin until application of wound dressing. Patient positioning and level identification were not included in the operation time. Final wound length was measured. Whether wound extension was necessary during surgery to facilitate access was not recorded. The primary surgeon for each case was recorded prospectively in the patient clinical record.
A correlation was sought between the variables via Pearson’s matrix. Correlation coefficient can be interpreted as follows: correlation coefficients (in absolute value) which are ≤0.35 are generally considered to represent low or weak correlations, 0.36 to 0.67 modest or moderate correlations, and 0.68 to 1.0 strong or high correlations with r coefficients ≥0.90 very high correlations [5]. Simple linear regression and stepwise linear regression with probability of rejection 0.05 was used to determine significant predictors of duration of the surgery. Analysis was carried out using Excel 2010 (Microsoft Corporation, Redmond, Washington) and Stata/IC 12.0 (StataCorp LP, College Station, Texas) and statistical significance was set at p≤0.05.
Results
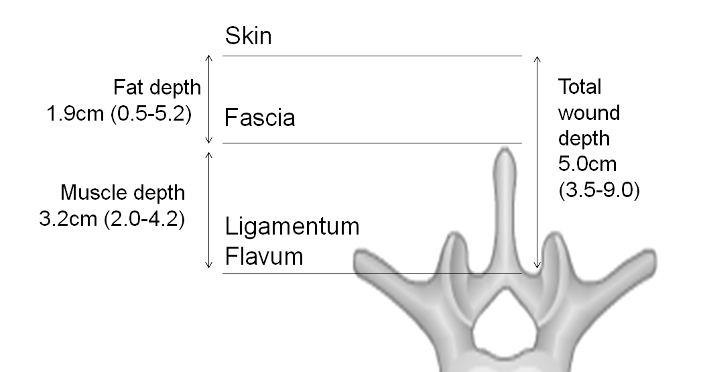
Of twenty-nine patients, the mean BMI was 30.4kg/m2 (19.7-47.2), abdominal girth 106cm (48-154), and operation duration 47 minutes (24-82). Mean wound length was 5.4cm (4.5-6.5), subcutaneous fat depth (Figure 1) was 1.9cm (0.5-5.2), muscle depth 3.2cm (2.0-4.2), and total wound depth 5.0cm (3.5-9.0). Fifteen patients were clinically obese, with a BMI >30 kg/m2 (Table 1). Mean operation duration among 15 obese individuals was 47.5 min (24-82) versus 14 non-obese was 45.5 min (24-77). Male patients experienced a longer operation duration by an average of 3 minutes (SE=6.2) than females.

Fifteen cases were trainee-performed and fourteen consultant-performed. Cases performed by the registrar were on average 8.2 minutes longer than the consultant, 50.4 minutes (24-77) versus 42.2 minutes (24-82) respectively (SE=5.8). This was not statistically significant in this sample. Of the cases with BMI >30kg/m2, eight were trainee-performed and seven consultant-performed.
Table 1: Demographics, discectomy level, operation duration, BMI, abdominal girth and wound measurements for twenty-nine individuals at lumbar discectomy
|
Patient study number |
Operator |
lumbar Oiscectomy |
Height |
Weight |
Abdom inal girth (cm) |
Sub. fat depthof wound (cm) |
Muscle Wound (cm) |
Total (cm) |
BMI |
Wound Length (cm) |
Operation duration (minutes) |
Sex |
Age |
|
|
1 |
Registrar |
L5/Sl |
164 |
97 |
122 |
2 |
3.2 |
5.2 |
36 |
6 |
46 |
M |
43 |
|
|
2 |
Registrar |
L5/Sl |
165 |
86 |
103 |
3 |
2 |
5 |
31.6 |
5 |
44 |
F |
25 |
|
|
3 |
Consultant |
L5/Sl |
180 |
76 |
105 |
1 |
3 |
4 |
23.5 |
5 |
24 |
M |
39 |
|
|
4 |
Consultant |
L5/Sl |
172 |
72 |
88 |
1.5 |
2.5 |
4 |
24.3 |
5 |
39 |
F |
43 |
|
|
5 |
Registrar |
L5/Sl |
174 |
70 |
88 |
1.8 |
2.7 |
4.5 |
23.1 |
4.5 |
37 |
F |
37 |
|
|
6 |
Consultant |
L5/Sl |
174 |
143 |
154 |
S.2 |
3.8 |
9 |
47.2 |
6.5 |
57 |
M |
38 |
|
|
7 |
Registrar |
L5/Sl |
173 |
77 |
104 |
2 |
2.5 |
4.5 |
25.7 |
5 |
56 |
M |
46 |
|
|
8 |
Registrar |
L5/Sl |
172 |
96 |
109 |
2.2 |
3.3 |
5.5 |
32.4 |
5.5 |
72 |
M |
44 |
|
|
9 |
Consultant |
L5/Sl |
180 |
93 |
109 |
2.7 |
2.3 |
5 |
28.7 |
5.5 |
36 |
M |
56 |
|
|
10 |
Consultant |
L4/5 |
165 |
108 |
135 |
3.5 |
3.5 |
7 |
39.7 |
6 |
50 |
F |
52 |
|
|
11 |
Consultant |
L4/5 |
167 |
91 |
118 |
1.5 |
3.5 |
5 |
32.6 |
5.5 |
50 |
F |
63 |
|
|
12 |
Consultant |
L4/5 |
162 |
93.7 |
104 |
1.8 |
3.2 |
5 |
35.7 |
4.5 |
26 |
M |
18 |
|
|
13 |
Registrar |
L4/5 |
179 |
97 |
120 |
0.8 |
3.5 |
4.3 |
30.3 |
4.5 |
36 |
M |
57 |
|
|
14 |
Consultant |
L4/5 |
173 |
88.9 |
48 |
2.2 |
4.2 |
6 |
29.7 |
6 |
40 |
M |
65 |
|
|
15 |
Registrar |
L4/5 |
175 |
94 |
118 |
2.7 |
3.3 |
6 |
30.7 |
6.2 |
24 |
M |
44 |
|
|
16 |
Registrar |
L4/5 |
176 |
81 |
96 |
1.7 |
2.4 |
4.1 |
26.1 |
6.5 |
77 |
M |
51 |
|
|
17 |
Registrar |
L4/5 |
166 |
87 |
112 |
1.4 |
2.8 |
4.2 |
31.6 |
5 |
62 |
F |
62 |
|
|
18 |
Consultant |
L2/3 |
167 |
70 |
92 |
0.5 |
3 |
3.5 |
25.1 |
4.5 |
40 |
F |
46 |
|
|
19 |
Registrar |
L4/5 |
150 |
84 |
103 |
2.1 |
3.9 |
6 |
37.3 |
6 |
47 |
M |
72 |
|
|
20 |
Consultant |
L4/5 |
164 |
53 |
79 |
0.6 |
3.5 |
4.1 |
19.7 |
5 |
25 |
F |
46 |
|
|
21 |
Registrar |
L3/4 |
184.5 |
101.9 |
123 |
1.2 |
2.9 |
4.1 |
29.9 |
6 |
75 |
M |
60 |
|
|
22 |
Registrar |
L4/5 |
179 |
69 |
84 |
1.4 |
3.5 |
4.9 |
21.5 |
4.5 |
41 |
M |
42 |
|
|
23 |
Registrar |
L4/5 |
177 |
85 |
110 |
3 |
3.5 |
6.5 |
27.1 |
5.5 |
60 |
F |
28 |
|
|
24 |
Consultant |
L4/5 |
180 |
104 |
107 |
1.4 |
3.9 |
5.3 |
32.1 |
5 |
30 |
M |
34 |
|
|
25 |
Consultant |
L4/5 |
190 |
115 |
110 |
2 |
3.5 |
5 |
31.9 |
6 |
82 |
M |
41 |
|
|
26 |
Registrar |
L4/5 |
152 |
89 |
118 |
2.5 |
2.5 |
5 |
38.5 |
5.5 |
44 |
F |
44 |
|
|
27 |
Consultant |
L4/5 |
176 |
83 |
100 |
1.7 |
3.7 |
5.4 |
26.8 |
5.5 |
51 |
M |
42 |
|
|
28 |
Consultant |
L4/5 |
184 |
115 |
109 |
1 |
3 |
4 |
34 |
6 |
42 |
M |
49 |
|
|
29 |
Registrar |
L4/5 |
159 |
70 |
97 |
1.5 |
2.8 |
4.3 |
27.7 |
5 |
36 |
F |
83 |
|
Table 2: Pearson product-moment correlation coefficient for variables listed
|
|
Operation duration (minutes) |
Total wound depth (cm) |
Abdominal girth (cm) |
Subcutaneous fat depth (cm) |
Muscle depth of wound (cm) |
BMI (kg/ m2) |
Wound length (cm) |
Age (years) |
|
Operation Duration (minutes) |
1.0000 |
|
|
|
|
|
|
|
|
Total wound depth (cm) |
0.1265 |
1.0000 |
|
|
|
|
|
|
|
Abdominal girth (cm) |
0.2681 |
0.4495 |
1.0000 |
|
|
|
|
|
|
Subcutaneous fat depth (cm) |
0.2154 |
0.8887 |
0.4966 |
1.0000 |
|
|
|
|
|
Muscle depth of wound (cm) |
-0.0575 |
0.5154 |
-0.0219 |
0.0774 |
1.0000 |
|
|
|
|
BMI (kg/m2) |
0.2026 |
0.6757 |
0.6930 |
0.6546 |
0.2440 |
1.0000 |
|
|
|
Wound length (cm |
0.4799 |
0.5159 |
0.3550 |
0.5140 |
0.2131 |
0.5258 |
1.0000 |
|
|
Age (years) |
0.1192 |
-0.1469 |
-0.1064 |
-0.2172 |
0.0996 |
0.0053 |
0.2229 |
1.0000 |
Pearson’s correlation matrix (Table 2) demonstrates that there was strong correlation between wound depth and subcutaneous fat depth (r=0.8887), confirming that a thick adipose tissue layer is the most common reason for deep wounds. There was a weak linear correlation between duration of operation and subcutaneous fat (r=0.2154), abdominal girth (r=0.2681) and BMI (r=0.2026). On average, the duration of the operation was increased by approximately 4 minutes per unit increase in subcutaneous fat (cm) (coefficient (SE) = 3.6 (3.1), p-value=0.26). A 10 unit increase in the abdominal girth (cm) caused an increase in duration of the operation by an average of 2 minutes (coefficient (SE) = 0.225 (0.156), p-value=0.16). However, this was not statistically significant in the current sample (Figure 2).
BMI (Figure 3), abdominal girth, discectomy level and trainee-performed cases demonstrated only a small effect size with regards to operative duration. BMI correlated with total wound depth, subcutaneous fat depth and abdominal girth. However, wound depth, fat depth, and BMI each have an effect on the wound length.

Simple linear regression showed that a unit increase in the wound length resulted an increase in operation time by 12 minutes (coefficient (SE) =12.2 (4.3), p-value= 0.008). Stepwise regression adjusting for age, gender, operator effect, abdominal girth confirmed that wound length significantly affected duration of the operation. The average operation duration for trainee performed cases reduced slightly over the course of fifteen cases (Figure 4), indicating that a learning curve may exist with

Discussion
Since Mixter and Barr’s first description of the lumbar discectomy in 1934, alteration to the technique have been described [6]. The ‘standard discectomy’ incision from L3 to sacrum was used by Caspar to compare with microdiscectomy in 1991 [7]. Modern open discectomy involves intervertebral level identification via intraoperative imaging, and specialised tissue retraction devices. As a result, wound length and paraspinal muscle disruption are reduced considerably.
One series compares open ‘macro discectomy’ using a 5cm incision to microdiscectomy via a 2.5cm incision, with an operative time of 40 and 45 min respectively. Blood loss, and visual analogue scores for sciatica pre- and post- operatively were similar [8]. Operative duration for microdiscectomy, either using open technique or minimally invasive (paraspinal muscle dilatation without separation from spinous processes), have been compared, with duration of approximately 122 minutes [9]. A randomised controlled trial of open versus micro endoscopic discectomy, found longer incisions, longer hospital stays but shorter operative duration in the open group [10].
Regarding grade of surgeon, a retrospective audit of 971 primary elective lumbar microdiscectomies showed no association with outcomes [11]. Incidence of perioperative complications in thoracolumbar spine surgery was not shown to be significantly different among obese individuals, in a cohort of 87 patients, 40.8% of whom were obese [2]. Lumbar fusion in obese individuals with BMI >30kg/m2 is associated with complication rates of over 40%, set-up times of one hour, and post-operative weight gain of 1.5kg versus 1.4kg weight loss in the morbidly obese (BMI >40kg/m2) [12]. The perceived challenge of lumbar discectomy in obese patients may relate that of lumbar fusion, and to perioperative factors such as positioning of patients, and management of comorbidities rather than depth of wound. We observed that in patents with an elevated BMI or abdominal girth, a large proportion of the body fat was located within the anterior abdominal wall rather than posteriorly at the operative site. Therefore, we propose that trainees should not be denied opportunities in lumbar discectomy based on the patient’s BMI or abdominal girth. Long-term follow-up for complications and validated outcome scoring is necessary to make detailed recommendations regarding patient selection for surgical training.
Conclusion
BMI, wound depth, and abdominal girth demonstrate weak correlations with operative duration. Total wound length has a significant association with operative duration in lumbar discectomy. A strong correlation exists between wound depth and subcutaneous fat depth. Cases performed by a consultant were shorter than those by a trainee in this study. The average duration of trainee-performed cases reduces over the course of fifteen cases. Elevated BMI and abdominal girth should not preclude surgical training in lumbar discectomy on the basis of anticipated prolongation of surgery.
Acknowledgements
The authors would like the theatre nurses in our institution for their assistance with the performing the operations and measurements.
Funding
No financial support was received for this study.
Conflict of Interest
No conflict of interest exists
Article Info
Article History
Research ArticlePublication history
Received 29 November, 2018Accepted 20 December, 2018
Published 28 December, 2018
Copyright
© 2018 Dallan P Dargan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository. All rights reserved.DOI: 10.31487/j.SSG.2018.01.001
Author Info
Corresponding author
Dallan P DarganDepartment of Orthopaedic Surgery, Musgrave Park Hospital, Stockman’s Lane, Belfast, Northern Ireland.
Figures & Tables
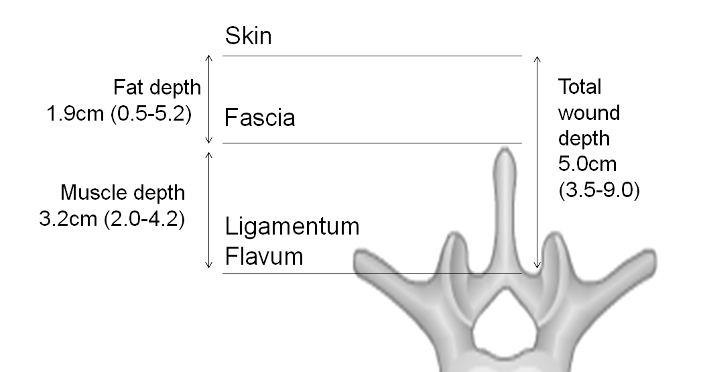



Table 1: Demographics, discectomy level, operation duration, BMI, abdominal girth and wound measurements for twenty-nine individuals at lumbar discectomy
|
Patient study number |
Operator |
lumbar Oiscectomy |
Height |
Weight |
Abdom inal girth (cm) |
Sub. fat depthof wound (cm) |
Muscle Wound (cm) |
Total (cm) |
BMI |
Wound Length (cm) |
Operation duration (minutes) |
Sex |
Age |
|
|
1 |
Registrar |
L5/Sl |
164 |
97 |
122 |
2 |
3.2 |
5.2 |
36 |
6 |
46 |
M |
43 |
|
|
2 |
Registrar |
L5/Sl |
165 |
86 |
103 |
3 |
2 |
5 |
31.6 |
5 |
44 |
F |
25 |
|
|
3 |
Consultant |
L5/Sl |
180 |
76 |
105 |
1 |
3 |
4 |
23.5 |
5 |
24 |
M |
39 |
|
|
4 |
Consultant |
L5/Sl |
172 |
72 |
88 |
1.5 |
2.5 |
4 |
24.3 |
5 |
39 |
F |
43 |
|
|
5 |
Registrar |
L5/Sl |
174 |
70 |
88 |
1.8 |
2.7 |
4.5 |
23.1 |
4.5 |
37 |
F |
37 |
|
|
6 |
Consultant |
L5/Sl |
174 |
143 |
154 |
S.2 |
3.8 |
9 |
47.2 |
6.5 |
57 |
M |
38 |
|
|
7 |
Registrar |
L5/Sl |
173 |
77 |
104 |
2 |
2.5 |
4.5 |
25.7 |
5 |
56 |
M |
46 |
|
|
8 |
Registrar |
L5/Sl |
172 |
96 |
109 |
2.2 |
3.3 |
5.5 |
32.4 |
5.5 |
72 |
M |
44 |
|
|
9 |
Consultant |
L5/Sl |
180 |
93 |
109 |
2.7 |
2.3 |
5 |
28.7 |
5.5 |
36 |
M |
56 |
|
|
10 |
Consultant |
L4/5 |
165 |
108 |
135 |
3.5 |
3.5 |
7 |
39.7 |
6 |
50 |
F |
52 |
|
|
11 |
Consultant |
L4/5 |
167 |
91 |
118 |
1.5 |
3.5 |
5 |
32.6 |
5.5 |
50 |
F |
63 |
|
|
12 |
Consultant |
L4/5 |
162 |
93.7 |
104 |
1.8 |
3.2 |
5 |
35.7 |
4.5 |
26 |
M |
18 |
|
|
13 |
Registrar |
L4/5 |
179 |
97 |
120 |
0.8 |
3.5 |
4.3 |
30.3 |
4.5 |
36 |
M |
57 |
|
|
14 |
Consultant |
L4/5 |
173 |
88.9 |
48 |
2.2 |
4.2 |
6 |
29.7 |
6 |
40 |
M |
65 |
|
|
15 |
Registrar |
L4/5 |
175 |
94 |
118 |
2.7 |
3.3 |
6 |
30.7 |
6.2 |
24 |
M |
44 |
|
|
16 |
Registrar |
L4/5 |
176 |
81 |
96 |
1.7 |
2.4 |
4.1 |
26.1 |
6.5 |
77 |
M |
51 |
|
|
17 |
Registrar |
L4/5 |
166 |
87 |
112 |
1.4 |
2.8 |
4.2 |
31.6 |
5 |
62 |
F |
62 |
|
|
18 |
Consultant |
L2/3 |
167 |
70 |
92 |
0.5 |
3 |
3.5 |
25.1 |
4.5 |
40 |
F |
46 |
|
|
19 |
Registrar |
L4/5 |
150 |
84 |
103 |
2.1 |
3.9 |
6 |
37.3 |
6 |
47 |
M |
72 |
|
|
20 |
Consultant |
L4/5 |
164 |
53 |
79 |
0.6 |
3.5 |
4.1 |
19.7 |
5 |
25 |
F |
46 |
|
|
21 |
Registrar |
L3/4 |
184.5 |
101.9 |
123 |
1.2 |
2.9 |
4.1 |
29.9 |
6 |
75 |
M |
60 |
|
|
22 |
Registrar |
L4/5 |
179 |
69 |
84 |
1.4 |
3.5 |
4.9 |
21.5 |
4.5 |
41 |
M |
42 |
|
|
23 |
Registrar |
L4/5 |
177 |
85 |
110 |
3 |
3.5 |
6.5 |
27.1 |
5.5 |
60 |
F |
28 |
|
|
24 |
Consultant |
L4/5 |
180 |
104 |
107 |
1.4 |
3.9 |
5.3 |
32.1 |
5 |
30 |
M |
34 |
|
|
25 |
Consultant |
L4/5 |
190 |
115 |
110 |
2 |
3.5 |
5 |
31.9 |
6 |
82 |
M |
41 |
|
|
26 |
Registrar |
L4/5 |
152 |
89 |
118 |
2.5 |
2.5 |
5 |
38.5 |
5.5 |
44 |
F |
44 |
|
|
27 |
Consultant |
L4/5 |
176 |
83 |
100 |
1.7 |
3.7 |
5.4 |
26.8 |
5.5 |
51 |
M |
42 |
|
|
28 |
Consultant |
L4/5 |
184 |
115 |
109 |
1 |
3 |
4 |
34 |
6 |
42 |
M |
49 |
|
|
29 |
Registrar |
L4/5 |
159 |
70 |
97 |
1.5 |
2.8 |
4.3 |
27.7 |
5 |
36 |
F |
83 |
|
Table 2: Pearson product-moment correlation coefficient for variables listed
|
|
Operation duration (minutes) |
Total wound depth (cm) |
Abdominal girth (cm) |
Subcutaneous fat depth (cm) |
Muscle depth of wound (cm) |
BMI (kg/ m2) |
Wound length (cm) |
Age (years) |
|
Operation Duration (minutes) |
1.0000 |
|
|
|
|
|
|
|
|
Total wound depth (cm) |
0.1265 |
1.0000 |
|
|
|
|
|
|
|
Abdominal girth (cm) |
0.2681 |
0.4495 |
1.0000 |
|
|
|
|
|
|
Subcutaneous fat depth (cm) |
0.2154 |
0.8887 |
0.4966 |
1.0000 |
|
|
|
|
|
Muscle depth of wound (cm) |
-0.0575 |
0.5154 |
-0.0219 |
0.0774 |
1.0000 |
|
|
|
|
BMI (kg/m2) |
0.2026 |
0.6757 |
0.6930 |
0.6546 |
0.2440 |
1.0000 |
|
|
|
Wound length (cm |
0.4799 |
0.5159 |
0.3550 |
0.5140 |
0.2131 |
0.5258 |
1.0000 |
|
|
Age (years) |
0.1192 |
-0.1469 |
-0.1064 |
-0.2172 |
0.0996 |
0.0053 |
0.2229 |
1.0000 |
References
1. Guss D, Bhattacharyya T (2006) Perioperative management of the obese orthopaedic patient. J Am Acad Orthop Surg 14: 425-432. [Crossref]
2. Yadla S, Malone J, Campbell PG, Maltenfort MG, Harrop JS, et al. (2010) Obesity and spine surgery: reassessment based on a prospective evaluation of perioperative complications in elective degenerative thoracolumbar procedures. Spine J 10: 581-587. [Crossref]
3. Meredith DS, Huang RC, Nguyen J, Lyman S (2010) Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J 10: 575-580. [Crossref]
4. Nowitzke AM (2005) Assessment of the learning curve for lumbar microendoscopic discectomy. Neurosurgery 56: 755-762. [Crossref]
5. Taylor R (1990) Interpretation of the correlation coefficient: a basic review. J Diagn Med Sonog 6: 35-39.
6. Mixter WJ, Barr JS (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211: 210-215.
7. Caspar W, Campbell B, Barbier DD, Kretschmmer R, Gotfried Y (1991) The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery 28: 78-87. [Crossref]
8. Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, et al. (2006) Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech 19: 344-347. [Crossref]
9. Lau D, Han SJ, Lee JG, Lu DC, Chou D (2011) Minimally invasive compared to open microdiscectomy for lumbar disc herniation. J Clin Neurosci 18: 81-84. [Crossref]
10. Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61: 545-549. [Crossref]
11. Ellenbogen JR, Marlow W, Fischer BE, Tsegaye M, Wilby MJ (2014) Is the rate of re-operation after primary lumbar microdiscectomy affected by surgeon grade or intra-operative lavage of the disc space? Br J Neurosurg 28: 247-251. [Crossref]
12. Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, et al. (2009) Lumbar spine fusion in obese and morbidly obese patients. Spine 34: 495-500.
