Mediastinal Lipoblastoma Causing Diaphragm Eventration - A Challenging Entity
Mediastinal Lipoblastoma Causing Diaphragm Eventration - A Challenging Entity
A B S T R A C T
Lipoblastoma is a rare benign neoplasm and its mediastinal location is even rarer. We report a boy with anterior upper mediastinal fat density mass extended to neck root with ipsilateral diaphragm eventration. Preoperative diagnosis was a lipomatous neoplasm. The exact diagnosis was established after complete excision via a cervical approach with complete recovery.
Keywords
Mediastinal mass, lipoblastoma, diaphragm eventration
Introduction
Lipoblastoma and lipoblastomatosis are rare benign tumors, originate from embryonal fat tissue (lipoblasts), both exhibit the same histology but two different morphologic types; 1) lipoblastoma is the most common type (66%), a localized well-circumscribed, encapsulated and tends to occur in more superficial locations, 2) lipoblastomatosis is a non-capsulated, diffuse, multicentric and deeply embedded with the tendency to infiltrate into adjacent strictures [1]. Mediastinum localization constitute only 1% to 3% of all cases and lipoblastoma is more common (94%) than lipoblastomatosis in this location [2]. The exact diagnosis for this entity usually not possible before surgery and histological study.
Case Report
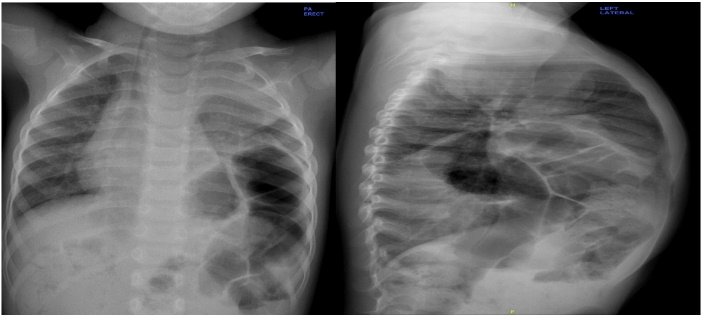
A 2-year-old boy, full-term with normal vaginal delivery, presented with shortness of breath and cough for one month, with past medical history of mild bronchial asthma, which was controlled by salbutamol nebulization only. On examination, apart from mild tachypnea, the rest of his vital signs were within normal limit, reduced air entry to left (LT) lung apex, a slight soft bulging could be noticed at neck root with the neck in extension position (Figure 1) and his weight was 10.4 Kg. Chest X-ray revealed eventration of LT diaphragm reaches up to 7th rib, the trachea is deviated to the right (RT) side and a mass shadow upper LT chest (Figures 2A & 2B).
Figure 1: Slight bulging over lower LT neck (arrow indicate level of the clavicle).
CT-scan showed a 5.1x7.2 cm fatty mass extending from the root of LT neck to the superior mediastinal (more on the LT side), displacement of the trachea towards the RT side with moderate narrowing of the tracheal lumen, the worst was noted at the level of the clavicle where the transverse diameter of the trachea was measured 3 mm. The mass also demonstrated anterior displacement of the common carotid artery and posterior displacement of the LT subclavian artery with immediate contact with the posterior part of the aortic arch (Figures 3A & 3B).
Figure 2: A) Posterior-anterior chest X-ray B) Lateral chest X-ray.
Figure 3: A) Coronal CT-scan image showing upper anterior mediastinal mass, trachea compression and deviation to RT side B) Axial CT-scan image showing the lower end of the mass extended down below the level of tracheal bifurcation.
MRI was done to obtain more information about the relation between the mass and the vessels. It revealed lobular high intense tumor on both T1 and T2-weighted images equivalent to subcutaneous fat, no solid enhancing component with complete encasement of the LT common carotid and subclavian arteries and it is abutting the posterior aspect of the aortic arch (Figure 4).
Figure 4: MRI.
Accordingly, a percutaneous CT-guided biopsy using a 17/18-gauge needle was performed and pathology report revealed mature fatty tissues. There was a controversy about whether to go thoracotomy or try cervical approach. The design was to start with cervical exploration and proceed to thoracotomy if needed. Through transverse incision at the root of LT neck, transection of LT sternocleidomastoid muscle identified the mass bulging (Figure 5A), it was extending deep to the neck strap muscles, firmly attached to the anterior superior mediastinum, as the mass was bluntly retracted into the neck, meticulous dissection carried out till complete removal of the mass (Figures 5B & 5C). The phrenic nerve was not encountered during surgery.
Figure 5: A) Soft tissue mass bulging after complete transection of LT sternocleidomastoid muscle (star indicate head side) B) The mass (star indicate head side) C) A 11x4x5.5 cm, smooth, lobular, yellow-tan mass, weighed 90 grams (arrow indicate inferior end).
Figure 6: A) Well circumscribed lipoblastoma with surrounding thin fibrous capsule (H&E, 2X) B) Lipoblasts, mature adipocytes and myxoid stroma with plexiform vascular pattern (H&E, 20X) C) Lipoblastoma with entrapped skeletal muscle (H&E, 10X).
The microscopic study revealed thin pseudocapsule (Figure 6A), lobules of lipoblasts, mature adipocytes and myxoid stroma with plexiform vascular pattern (Figure 6B), entraped skeletal muscle (Figure 6C) and the lobules separated by cellular fibrous septae. The Post-operative course was uneventful. He was followed up for 2 years with no signs of recurrence with persistence LT diaphragm eventration.
Discussion
Jaffe, in 1926, first described lipoblastoma as a typical lipoma that consisted of immature fat cells (lipoblast) [3]. In 1958, Vellios et al., first described lipoblastomatosis in RT chest wall, axilla, and supraclavicular region in an 8-month-old girl [4]. Chug and Enzinger, in 1973, established the morphologic criteria of this tumor (lipoblastoma and lipoblastomatosis) [1]. It occurs almost exclusively in infants and early childhood, with 88% of cases in children being under 3-year-old [1]. It can arise almost anywhere within the soft tissue, and the commonest site is extremity, followed by trunk, head and neck [1, 5]. Other rarer locations include the omentum, scrotum, labia, inguinal, perineum, retroperitoneum, thoracic wall, heart, lungs and mediastinum [5].
Lipoblastoma is a benign tumor with good prognosis with no reported metastasis nor malignant transformation [3, 6]. Most of these tumors grew slowly but steadily with potential for local invasion and rapid growth and may attain large sizes [1, 5]. The severity of the symptoms depends on the size and location of the tumor [3]. Mediastinal lipoblastoma can be present with dyspnea, wheezing, cough, stridor, life-threatening asphyxia due to airway compression, vessel compression, superior vena cava syndrome, chest infection, neck swelling, chest wall protrusion and neurological symptoms resulting from spinal cord compression [2, 5-7].
In our case, the patient presented with recent onset of cough and tachypnea due to upper airway compression, but we thought he had symptoms longtime before, which were misinterpreted as mild asthma due to longstanding recurrent symptoms. To our knowledge, phrenic nerve involvement with mediastinal lipoblastoma has been reported in two cases in the literature and diaphragm eventration was presented only in one of them [2, 7]. In our case, we think the long-standing mass compression of LT phrenic nerve results in ipsilateral eventration. We were unable to visualize the LT phrenic nerve probably because we went through the cervical approach and maintained dissection close to the mass.
MRI and CT-scan show a fat composed tumor with anatomical detail of soft tissue masses but it is not specific enough to be used alone for differentiation among adipose tissue tumors like lipoma, lipoblastoma, fibrolipoma, teratoma, lipomatous hamartoma, spindle cell lipoma and liposarcoma [8]. It is imperative to differentiate especially those malignant lipomatous tumors because their prognosis and management are different. Complete local excision of the mass is the treatment of choice to establish the correct diagnosis and relieve patient symptoms [2, 3, 5]. In most reported cases of mediastinal lipoblastoma with neck, extension was operated via thoracotomy. In our case, we were able to remove the tumor completely through cervical approach, which we think it deserve to be considered.
Because of the benign nature of the tumor, sacrificing major structures during surgery should be avoided. Local recurrence has been reported in 14% to 24% of cases, usually due to incomplete excision or diffuse type [1, 2]. So, a follow-up period of at least 3 years is recommended and re-excision is the treatment of choice in case of recurrence [3]. The histology, according to the World Health Organization, lipoblastoma is characterized by the proliferation of mature and immature fat cells with mesenchymal precursors and lipoblasts at varying stages of differentiation. Small lobules of mature and immature fat cells are separated by fibrous trabeculae with or without a myxoid stroma, which contains blood vessels. The diffuse variant shows a less pronounced lobular pattern [3]. Sometimes the histological diagnosis is difficult because of the close resemblance with myxoid, round cell, and well-differentiated liposarcoma. In our case, the patient’s age, absence of mitosis and atypical nuclei and molecular cytogenetic analysis helped in making the correct diagnosis [3, 9].
Conclusion
We present a rare case of anterior superior mediastinal lipoblastoma that results in ipsilateral diaphragm eventration and upper airway compression. The exact diagnosis was established after complete resection of the mass via a cervical approach. Mediastinum lipoblastoma is a clinical and surgical challenge because, despite its benign nature, it has the potential of rapid growth and local invasion, which required complete but conservative excision. Hence, the familiarization of these tumors is necessary.
Competing Interests
None.
Consent
The consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgements
We appreciate all the efforts of Dr. Salman T. AL Malki, Consultant Pathologist Dermatopathology and Soft tissue/Bone Pathology, who provided us with the full pathology report about our patients.
Article Info
Article Type
Case ReportPublication history
Received: Mon 10, Aug 2020Accepted: Mon 24, Aug 2020
Published: Tue 01, Sep 2020
Copyright
© 2023 Alam Ara Shafi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.09.01
Author Info
Majd A. Hadad Abdulwahab S. Aljubab Alam Ara Shafi
Corresponding Author
Alam Ara ShafiGeneral Surgery Department, King Fahad Medical City, Riyadh, Saudi Arabia
Figures & Tables





References
- E B Chung, F M Enzinger (1973) Benign lipoblastomatosis. An analysis of 35 cases. Cancer 32: 482-492. [Crossref]
- Mehmet Mutlu, Nilgün Yarş, Mustafa Imamoğlu, Polat Koşucu, Havva Turgutalp (2009) Mediastinal Lipoblastoma Causing Diaphragmatic Eventration: A Case Report and Review of the Literature. J Pediatr Hematol Oncol 31: 346-348. [Crossref]
- Claudio Spinelli, Sara Costanzo, Elisa Severi, Giulia Giannotti, Francesco Massart (2006) A Thoracic Wall Lipoblastoma in a 3-Month-Old Infant: A Case Report and Review of the Literature. J Pediatr Hematol Oncol 28: 594-600. [Crossref]
- F Vellios, J Baez, H B Shumacker (1958) Lipoblastomatosis: a tumor of fetal fat different from hibernoma; report of a case, with observations on the embryogenesis of human adipose tissue. Am J Pathol 34: 1149-1159. [Crossref]
- Hudsona SA, Lacsona GA, Dicken JB (2019) Benign giant mediastinal lipoblastoma. J Pediatr Surg Case Rep 40: 38-42.
- Mohammad Hanafiah, Mohammad Noryati, Talib Arni (2013) Mediastinal lipoblastoma: unexpected finding of a chest infection. BMJ Case Rep 2013: bcr2013009879. [Crossref]
- I Irgau, K W McNicholas (1998) Mediastinal Lipoblastoma Involving the Left Innominate Vein and the Left Phrenic Nerve. J Pediatr Surg 33: 1540-1542. [Crossref]
- Kazuhiro Kaneyama, Atsuyuki Yamataka, Tadaharu Okazaki, Geoffrey J Lane, Takeshi Miyano (2006) Magnetic Resonance Imaging in Lipoblastoma: Can it be a Diagnostic Modality? Asian J Surg 29: 198-201. [Crossref]
- Parul Ghosh, Ram Narayan Das, Ranajoy Ghosh, Uttara Chatterjee, Chhanda Datta et al. (2015) Lipoblastoma and lipoblastomatosis: A clinicopathological study of six cases. J Cancer Res Ther 11: 1040. [Crossref]
