Modifying ICU Rooms to Protect Health Care Workers During the COVID 19 Crisis: Brief Report
A B S T R A C T
Background: With the growing crisis of the pandemic COVID-19, healthcare providers have been put under tremendous emotional stress and physical strain attempting to protect themselves from contracting the infection while caring for critically ill patients. This task is further challenged by the global shortage of the protective equipment recommended for their safety.
Methods: In two different ICUs in different hospitals in Hawaii, we were able to modify our rooms, both those equipped and not equipped with negative pressure capabilities. We were able to remove the intravenous pumps, feeding tubes, and even the ventilator monitors out of the patient room without affecting the negative pressure inside the room. The purposes of such measures were to reduce the exposure risk for nurses, respiratory therapists, radiology technicians, and physicians from entering the room for routine medication changes, blood draws, or ventilator checks. Those measures are by no means to neglect the patients from physical examination, communicating with the patient if alert enough, or emergency situations.
Conclusion: The modifications implied are feasible, practical and conceptually safe to implement. We hypothesize that those measures will reduce the number of times entering the rooms for routine measures, thus reducing personnel exposure, infection rate, and reducing the growing need for the now precious PPE. Additionally, it will enhance response time to medications needs or ventilator adjustments.
Keywords
C0VID-19, PPE, ICU rooms
Introduction
SARS-COV 2 was emerged from China in December 2019, and has since emerged as a worldwide pandemic, with infection and mortality rates rising exponentially worldwide and changing daily per the John Hopkins data center [1]. Health care workers in hospitals, clinics are in the front line fighting this crisis and they are at highest risk for exposure and contracting the infection. There are multiple guidelines from CDC and other societies regarding protective measures for healthcare workers, personal protective equipment (PPE) including eye protection, gowns, face masks, N-95 respirators [2]. Despite these measures many still fall sick or even die from contracting the virus on duty.
The data on actual infection rate or mortality among healthcare workers are very scarce and inconsistent. A report from Italy estimated an infection rate of about 20% though does not report mortality [3]. Another report from China in mid-February reported more than 1,700 healthcare workers with 6 dead [4]. Spain reported more than 12,000 healthcare workers infected accounting for 14.4% of total infection rate in the country [5]. In the USA, the data involving the healthcare population is very scarce and remains unknown. The CDC recently reported in April a tally of health care workers infected of about 9,200 with 27 deaths and suggests that health care workers account for about 11% of the total COVID-19 infections [6]. One case report described 41 healthcare workers exposed to aerosolized procedure of a COVID-19 patient, none of them tested positive or developed symptoms, 85% of them were wearing regular surgical masks and 15% wore N-95 respirator [7]. This observation suggests that in additional to PPE, other measures can be taken to significantly reduce the risk of acquiring the virus while taking care of the ill. Unfortunately, with the growing numbers of infection worldwide, there has been equally problematic crisis in the marked shortage and lack of those equipment available for health care workers.
Case Presentation
First case, a 70-year-old Caucasian man with type II diabetes mellitus and hypertension who was admitted to the ICU of the first hospital with acute hypoxic respiratory failure on mechanical ventilation secondary to COVID-19 infection confirmed by SARS-COV 2 Polymerase Chain Reaction assay (PCR). Second case, an 82-year-old male, with history of congestive heart failure and coronary artery disease admitted to the ICU of the second hospital with acute hypoxic respiratory failure requiring high flow nasal cannula (HFNC) secondary to COVID-19 infection confirmed by PCR.
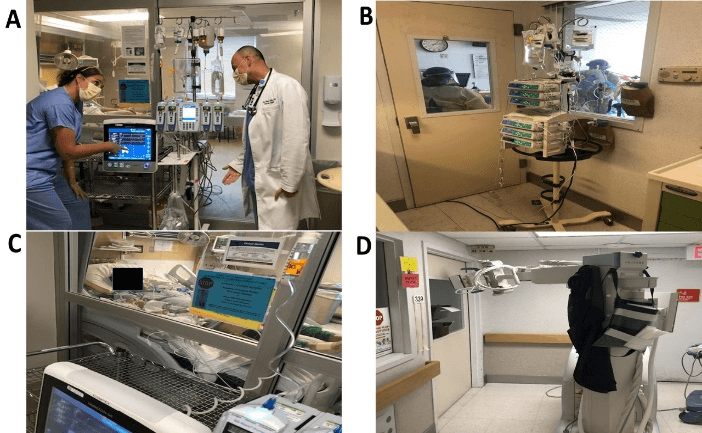
With collaboration between all healthcare personnel in both ICUs, the patients were transferred to a negative pressure room with modifications to minimize frequency of room entrance. Lines and transducers were extended and modified so that intravenous pumps, feeding tubes, and the ventilator graphic user interface (GUI), can be placed outside the patient’s room (Figures 1A-1C). Concerns regarding air leaks and loss of negative pressure inside the room were addressed by having clinical engineers assess the room to ensure the pressure inside the room remains unaffected. Routine tasks such as administering IV medications, blood draws, and ventilator checks and adjustments were done outside the patient’s room.
The numbers of times healthcare personnel are required to enter the room were observed over a period of 7 days. Nurses are observed to enter the room approximately once every 4 hours and respiratory therapist only needs to enter the room when managing endotracheal tubes. We were also able to reduce the number of PPE used while providing care for this patient more efficiently.
Discussion
During this global pandemic, hospitals are doing their best in protecting healthcare workers who are in the frontline of this fight. With new challenges and information that come to light every day, hospitals and health organizations are required to adapt quickly by constantly implementing and adjusting policies and procedures. Providing PPEs, limiting visitations, and screening patients and staff members are vital and have been implemented in most healthcare settings. We believe that additional measures can be taken to minimize risk of exposure and thus prevent more morbidity and mortality from COVID-19 among our colleagues. With the modified room, routine tasks and monitoring can be carried out safely outside the patient’s room. Not only do these measures minimize unnecessary exposure of our healthcare providers, but it also helps to preserve PPE that is in short supply. Although our cases were done in a negative pressure room, we believe these measures can also be used in a regular ICU room.
We need to emphasize that these modifications are not intended to negatively affect necessary patient communication, physical examination, and routine turning, or attending to emergent needs of the patient. We recognize that many factors can limit modifications made to these rooms. Some examples include room designs, door configurations, visibility of monitors, and presence of surveillance camera that allows close monitoring from the nursing station. Additionally, in our case, we were able to use a ventilator with a detachable GUI that can be mounted at a distance from the ventilator itself (Figures 1A & 1C), which is not available in all ventilator machines. Recently there has been some work on trying to control the ventilators remotely. Other considerations include obtaining imaging such as chest x-rays for these patients. We were able to get high-quality imaging even with the x-ray machine from outside the room (Figure 1D).
Figure 1: A) Room configuration in first hospital showing intravenous pumps and ventilator GUI outside the room. B) Room configuration in second hospital showing intravenous pumps outside the room with lines passing under the door. C) Intravenous lines and ventilator GUI cable passing between sliding doors in first hospital. D) Obtaining portable chest x-ray from outside the closed ICU room.
Conclusion
Adjusting the ICU rooms to minimize exposure from performing routine tasks on patients with COVID-19 is feasible and conceptually reduces the risk of contracting the infection, and thus death, of our health providers. In addition, it may preserve PPE and reduce time to attend to patients’ hemodynamics and ventilator needs.
Funding
None.
Key Points
i. COVID-19: Novel SARS-COV 2 virus declared as worldwide pandemic starting in China in December 2019, declaring life of thousands and infecting health care providers fighting this infection.
ii. Measures to protect health care workers including personal protective are challenging and lacking.
iii. Any additional measures to protect our health care workers in their fight against the viral infection should be welcomed and implemented.
Article Info
Article Type
Case ReportPublication history
Received: Mon 18, May 2020Accepted: Mon 01, Jun 2020
Published: Fri 26, Jun 2020
Copyright
© 2023 Ehab Daoud. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CEI.2020.02.04
Author Info
Ehab Daoud Marissa Su Mia Shokry
Corresponding Author
Ehab DaoudAssistant Professor of Medicine, John A. Burns School of Medicine, University of Hawaii, USA
Figures & Tables
References
- Watson C, Cicero A, Blumenstock J, Fraser M (2020) A National Plan to Enable Comprehensive COVID-19 Case Finding and Contact Tracing in the US. John Hopkins Univ Med.
- Center of Disease Control and Prevention (2020) Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19). Healthcare Sett.
- Remuzzi A, Remuzzi G (2020) COVID-19 and Italy: What Next? Lancet 395: 1225-1228. [Crossref]
- Bellisle M (2020) How Many Medical Workers Have Contracted COVID-19? States Lack Key Data. Oregon public broadcasting.
- Schnirring L (2020) COVID-19 sickens over 1,700 health workers in China, killing 6. Univ Minnesota Center Infectious Disease Res Policy.
- Kaiser Health News 2020.
- Ng K, Poon BH, Kiat Puar TH, Shan Quah JL, Loh WJ et al. (2020) COVID-19 and the Risk to Health Care Workers: A Case Report. Ann Intern Med L20-0175. [Crossref]
