Necrotizing Soft-Tissue Infection and Necrotizing Fasciitis in Adults of a Single Center: Review, Current Concepts and Challenges
A B S T R A C T
Background: The aim of this work is to assess the clinical and therapeutic characteristics of patients treated for necrotizing soft-tissue infection/necrotizing fasciitis (NSTI/NF) and determine their outcomes.
Patients and Methods: During the period 1/2012-12/2019 24 adults (18 males, 6 females, aged 33-91 years/mean age 52.4 years) with NSTI/NF were treated. Comorbidities were encountered in 20 (83.3%). Eighteen patients (Group I) presented late, with gangrene and systemic inflammatory response syndrome (9) or septic shock/ organ dysfunction (9). Six patients (Group II) presented early, with local pain, fever, and erythema. Affected areas included perineum-scrotum- external genitalia- abdominal wall or thigh, extremities-trunk, and gluteofemoral area in Group I, and scrotum, extremities, and labium majus in Group II.
Results: Intensive resuscitation and antibiotics were started immediately. All patients had a CT scan and underwent surgery within 4 hours from admission. All necrotic soft tissues were aggressively excised. Additionally, patients underwent Hartmann’s colectomy (3) or colostomy (3), thoracostomy (1), opening of compartments of extremities (2), and extrapelvic drainage (1).Wounds were packed open; specimens were sent for Gram stain/cultures and histology. From Group I, 14 remained intubated for 2-10 days, and 15 required 1-5 further limited debridements or incisions (mean 2). Histologically, tissue necrosis was confirmed in all patients, NF in 18. Infection was polymicrobial in 20. Antibiotics were modulated based on culture results. Four Group I diabetics with extended perineal NF died due to uncontrolled sepsis (16.66%). Survivors received antibiosis for 10-18 days (mean, 15), were helped with nutritional support, and they had a planned wound closure or reconstruction. Their mean hospitalization was 28 days (range, 12-46).
Conclusion: Improving diagnosis of NSTI/NF requires awareness for early recognition and prompt initiation of aggressive treatment, particularly for lesions extended beside perineum. Unfavourable outcome is affected by the delayed or inadequate surgery and the degree of multiple organ dysfunction on admission.
Keywords
Necrotizing soft-tissue infection, necrotizing fasciitis, multidisciplinary treatment, debridement, necrectomy
Introduction
Necrotizing soft-tissue infection (NSTI) has been recognized for millennia, with reports dating back to notations by Hippocrates [1]. NSTI is an uncommon heterogeneous disease, which describes a group of fulminant infections, mostly virulent bacterial, that swiftly can spread through fascial planes causing necrosis of skin, soft tissues, and muscles, and that can rapidly lead to intoxication/systemic inflammatory response syndrome (SIRS), septic shock/multiple organ dysfunction syndrome (MODS) and death [2-8]. Necrotizing fasciitis (NF) is the most common type of NSTI and the most complicated and life-threatening NSTI [2]. It causes fulminant clinical deterioration in any patient, regardless of the patient's immune status.
The infection usually originates from the gastrointestinal tract, the genitourinary tract, or dermal-cutaneous injuries. A secondary host's colonization of their own indigenous aero-, anaerobic microflora usually leads to polymicrobial infection [2, 5, 9]. Bacteremia is accompanied by the production of particularly destructive toxins that are released into the systemic circulation; this is crucial as it is the starting link in the mechanism of development of fascial necrosis that initiates the cytokine cascade, which is leading to the endothelial damage [4]. Causative organisms proliferate in an environment of tissue hypoxia. The coagulation cascade of thromboplastin is activated resulting in inhibition of fibrinolysis and in the formation of disseminated microthrombosis of vessels feeding the fascia; in addition, the prolonged vasoconstriction in the dermal capillary network, the resultant extravasation of the liquid part of the blood, the tissue swelling and the leukocyte infiltration lead to the ischemic necrosis and liquefaction of the fascias and the surrounding tissues [2, 7, 9].
Even nowadays, NSTIs are associated with a high burden of surgical and critical care, as well as high morbidity and mortality for the patients [4]. Previous research has shown that morbidity and mortality rates increase when patients are not presented early in the course of their disease, they are transferred from other outside facilities, or when initiation of their treatment delays [4, 10-18]. The patients may be delayed in seeking medical help, mostly because of the rapid spread of the pathological process in deep tissues along the fascias, the lack of superficial changes of the skin over the infectious focus, and the absence of significant subjective sensations due to the destruction of the subcutaneous nerves, all leading to an underestimation of the severity of the disease [7, 17, 18]. On the other hand, in clinical practice, time to surgical intervention decreases and outcome improves, most likely due to increased awareness and more timely referral of the NSTI patients [3, 4, 13-15]. However, diagnosis in the early stages can be challenging, as local signs can be minimal and only become prominent as the disease progresses [3, 7, 11, 16, 17].
Patients and Methods
I Search Methods
This review included all adults with suspected NSTI/NF who were admitted to the General Hospital of Nea Ionia Constatopoulion-Patission “Aghia Olga”, Athens- Greece. An approval was granted by the Institutional Review Committee for retrospective patients' data collection from the Hospital medical records and medical files. The objective of this study was to determine the presentation of patients diagnosed with NSTI/NF and their in-hospital outcomes. In particular, we addressed the following issues: i) origin of soft-tissue infection, ii) progression of infection to NF, iii) microorganisms involved and antibiotics used, iv) clinical and histological staging of NF, v) type of surgical intervention, and vi) extend of holistic multidisciplinary treatment. This article contains the relative literature research, particularly the recent, using PubMed for the MEDLINE database.
II Case Presentation
During the period 01/2012-12/2019, 24 patients with NSTI/NF were treated at our Department of Surgery. There were 18 males and 6 females, with mean age 52.4 years (range, 33-91). All patients with suspected NSTI/NF, except 3 cases that were transferred from outside facilities, were initially admitted undiagnosed to the Emergency Department (ED); inpatients had the diagnosis of “worsened (necrotizing) infection” of perineum, scrotum, and labium majus following inadequate drainage before 24-48 hours. Comorbidities were encountered in 20 patients (83.3%) (Table 1).
Table 1: Risk factors for development of infection and initiating pathologic conditions in 24 patients with NSTI/NF.
|
Preexisting conditions |
No of patients |
|
|
Advanced age (>65 years) Diabetes mellitus Hypertension under medication Chronic pulmonary disease Peripheral vascular disease Congestive heart disease Obesity Malnutrition Chronic alcoholism Active IV drug use, steroid use/ immunocompromised status Malignancy |
8 12 6 4 7 2 6 3 2 3
1 |
|
|
Initiating pathologic conditions |
No of patients |
|
|
Perineal abscess or chronic anal fistula/fissure Periurethritis/epididymoorchitis after instrumentation(urethral rupture) Post-hemorrhoidectomy wound infection Anorectal carcinoma (anastomotic recurrence) Bartholin’s cyst abscess Tibial chronic vascular ulcers-sinuses(assoc. compartment syndrome in 2) Abscess after IM/IV injections (2 immunocompromised) |
8
6
1 1
1 |
Anorectal- genitourinary foci |
|
4
3 |
Dermal foci |
|
Figure 1: Fournier's gangrene extended to scrotum-penis-perineum-lower abdominal wall.
Prompt recognition and initial evaluation of cases suffering from a serious soft-tissue infection that was spreading rapidly and was accompanied by determinable systemic signs and symptoms, and of suspected cases for which such an infection could not be easily ruled out as well, was followed by immediate intensive resuscitation for the more severe cases, and by variable supporting for the remaining, coupled with a simultaneous laboratory work-up, which included blood chemistry analysis, aerometry and computed tomography (CT). Most antibiotics of an empirical broad-spectrum regime were initiated near the time of hospital admission and blood cultures were generally obtained before antibiotic administration (first-line treatment).
Table 2: Main local physical-clinical findings in 24 patients with NSTI/NF.
|
Late findings – Group I patients |
Early findings – Group II patients |
* LRINEC score ≥6 - 6 patients >8 - 12 patients |
* LRINEC score 5 - 3 patients 6 - 3 patients |
Table 3: Origin/type of infection and systemic manifestations in 24 patients with NSTI/NF.
|
Infectious origin: Affected area/ Depth |
Severe systemic manifestation: No of patients |
Type of infection: No of patients |
|
|
Anorectal, Urogenic:
|
Skin, fascia
|
|
Polymicrobial/Type I: 17 patients
|
|
Dermal wound (bite?):
|
Skin, fascia
|
|
Polymicrobial/Type I: 3 patients
|
|
Dermal wound-IM/IV drug abuse:
|
Skin, fascia, muscle
|
|
Monomicrobial/Type II: 2 patients
|
|
Dermal wound- IM/IV drug abuse:
|
Fascia, muscle |
|
Monomicrobial/Type III: 2 patients
|
Late physical findings were encountered in 18 patients, who were considered as having prolonged necrotic infection (Group I). Their extensive affected body areas involved: the perineum, scrotum-external genitalia and lower abdominal wall or upper thigh (14 patients; additionally, anorectal necrosis: 3, left pleural-pericardial collection: 1), the lower extremity (two patients with compartment syndrome: thigh 1, tibia 1), the right gluteofemoral area (one patient) and the upper extremity-trunk (one patient) (Figure 1). Disproportional local pain or local anaesthesia, skin necrosis or ischaemia, and erythema/edema (with crepitus in 12 patients), were the main physical findings. Systemic manifestations detecting sepsis were encountered: tachycardia/tachypnea, hypotension, oliguria-anuria, hyperglycemia or metabolic acidosis, leukocytosis, and high fever (except in one immunocompromised), and alterations of mental status (7 patients). All these patients had an immediate laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring system score≥6, which, however, was not timely used in cases with “hard” signs of NF and certain clinical diagnosis. Their condition was manifested with either SIRS (9 cases) or toxic septic shock and/or MODS (9 cases), with at least 2 organs – usually lungs and kidneys-dysfunctioning (Tables 2 & 3).
Immediate and intensive fluid resuscitation, correction of metabolic disturbances and hemodynamic support were started in the ED and were calculated according to the requirements and preexisting conditions of each patient. Three patients with severe cardiopulmonary instability were emergently intubated in the ED. Group I patients waited an average 3.5 days (range, 18 hours-6 days) after the onset of symptoms before seeking medical advice. The remaining 6 patients were timely presented with early local findings (Table 2), consisting of the Group II. They were presented with 1-2 days fever, the most annoying local pain out of proportion to the physical appearance, and tense edema beyond the area of erythema or skin bronzing. Affected areas in this group were: the scrotum (2 patients), the labium majus (inadequately opened Bartholin’s cyst abscess 1) and the extremities (forearm 1, tibia 2). Comorbidities were detected in 3 patients (diabetes mellitus, hypertension, peripheral vascular disease). Symptoms of systemic toxicity were lacking in Group II patients; their LRINEC scoring system score was 5 or 6. Since their other findings were highly suspicious for underlying NSTI or NF, variable supporting, particularly fluid hydration, was initiated at the ED. The initiating pathologic conditions of the inflammatory process were either distinct or considered probable and included perineal-anorectal-urogenic foci in 17 patients, and dermal foci on the trunk, gluteus, and extremities in 7 patients (Tables 1 & 3). Complete information about the type of microbial infection was obtained later (24-48 hours from admission) in the course of the disease. Differential diagnosis in the early stages of suspected disease included the non-necrotizing cellulitis and the ulcerative and gangrenous forms of inguinal lymphogranulomatosis.
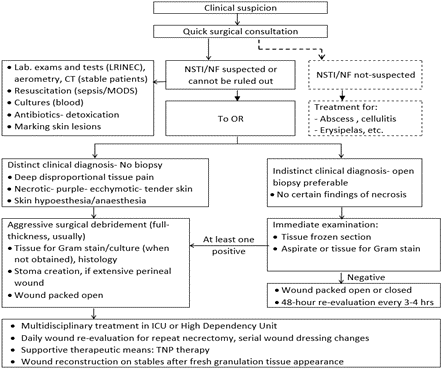
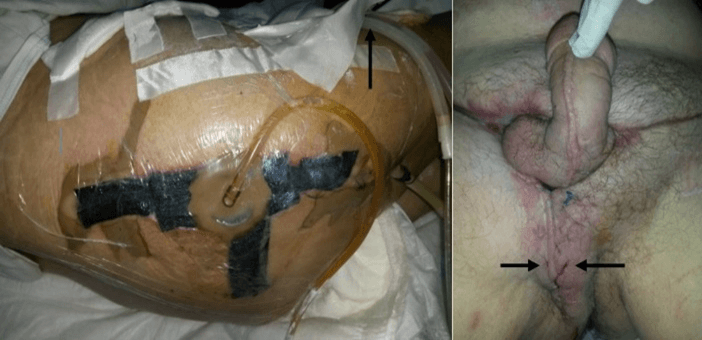
Laboratory results in Group I cases included: leukocytosis with white blood count 18-30x109/L (with high number of immature forms in most severe cases) or leukopenia in one immunocompromised patient, C-reactive protein >180mg/L, creatinine≥1.8 mg/dl, hyperglycemia with glucose >220 mg/dl in all diabetics, and metabolic acidosis; results in Group II patients showed milder increase in white blood count (normal count in one immunocompromised), C-reactive protein and glucose levels. Bacteremia upon admission was documented in only 4 cases (16.66%) with prolonged infection. Simultaneously to the required stabilization, all patients underwent a CT scan at the site of infection (using contrast media when creatinine value permitted it), which constantly detected the extent of tissue edema and the infectious infiltration, and in 16 patients the pathognomonic signs of fascia/fascia-muscular necrosis or deep tissue emphysema (Figure 2).
Figure 2: Pathognomonic imaging findings of fascia necrosis and deep tissue emphysema (arrows) in thigh (left) and rectosigmoid (right).
In three of the most severe cases, necrosis or emphysema were extending to the anorectum and the perirectal tissues; in one case the infectious infiltration reached as far as the left pleural and pericardial cavities. In addition, for cases with extremities involved, plain radiographs showed superficial tissue edema or emphysema, and Triplex confirmed the diagnosis of compartment syndrome in two patients who raised the suspicion for it.
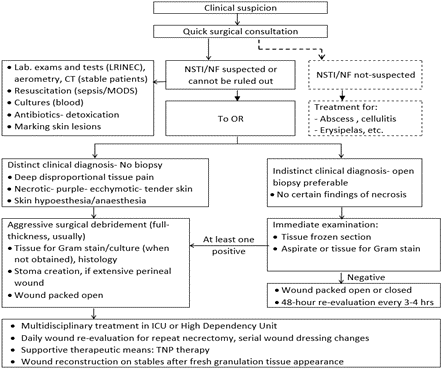
We followed a clinical diagnostic and treatment algorithm for the management of NF suspected patients and patients for whom NSTI could not be ruled out (Table 4). Perioperative reversal of the effect of traditional or novel anticoagulants and antiplatelet medications (3 patients for each of them) was achieved by fresh frozen plasma transfusions and prothrombin or vitamin K administration. Under continuous resuscitation, all patients were transferred to the operating room (OR) within 4 hours from admission, irrespective of the degree of their hemodynamic stability restoration. In Group II patients, an incisional biopsy via a longitudinal incision in the Langer’s lines over the most suspected affected area was primarily performed under regional or spinal anaesthesia; samples contained subcutaneous tissue, fascia, and muscle; at least one immediate result of rapid tissue frozen section or aspirate/tissue for Gram stain (Hematoxylin & eosin) was achieved within 35 min and it was found positive. Relative biopsy findings included: vessels’ thrombi or necrosis, fascial ischaemia, polymorphonuclear infiltration and isolated microorganisms. These patients, soon after biopsy results, and all of the Group I patients underwent aggressive surgical debridement under general (20 patients) or spinal (4 Group II patients) anaesthesia.
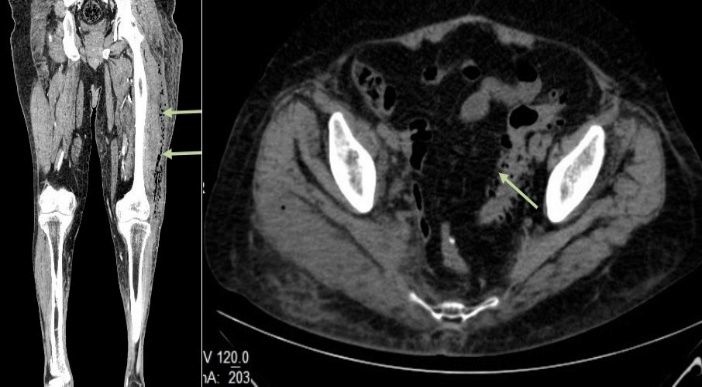
Figure 3: Index surgery: Large wounds involving perineum, scrotum, penis, and lower abdominal wall in a 91-year-old man (left), an 87-year-old man (medium) and a 75-year-old man (right). Denuded testicles are shown (white arrows), as well as a loop sigmoid stoma (left: arrowhead) and an urethral rupture (medium: black arrows).
All necrotic, ischemic tissues, and even tissues of doubtful viability, both in extent and depth, were radically excised until healthy tissues were reached, and all contaminated tissue planes were opened, debrided, cleansed, and drained (Figure 3). Intraoperatively, macroscopic findings that we considered as pathognomonic for NF were dull grey (necrotic) fascia-tissue, small vessel thrombosis/ lack of bleeding, tissue easily elevated off of the fascia/positive “finger test”, non-constructing muscle and “dishwater” pus. Tissue specimens and fluid aspirates were obtained for immediate Gram strain, as well as for aerobic and anaerobic cultures with sensitivities and histology. All residual tissue defects were packed open.
For patients with necrosis from anorectal/urogenital origin, the result of the wide tissue excision was a single defect but more extensive and composite, which involved the perineum, external genitalia, and/or lower abdominal wall and upper thigh(s). Six septic patients required additionally either an atypical low Hartmann’s resection for rectosigmoid infectious involvement (3 patients, including one with recently recognized anastomotic recurrence after excision for rectosigmoid carcinoma before 8 months in another hospital: they underwent anoscopy in the OR) or a diverting loop sigmoidostomy for large perineal wound (3); a 91-year-old man underwent also a tube thoracostomy for left pleural empyema. When needed, the testicles were simply denuded but spared. Two other patients with compartment syndrome underwent wide opening of one (tibia) or two (thigh) compartments. A 76-year-old woman with gluteofemoral NSTI/NF underwent gluteal debridement and deep intramuscular dissection for tube drainage and cleansing of the ipsilateral extrapelvic space for related infectious collection at the internal surface of the pelvic acetabulum (CT finding), accessed via a separate groin incision and deep dissection; a set of two plastic tubes was placed into the extrapelvic space for continuous “washing”. One drug addict with upper extremity- trunk NSTI/NF required the greatest number (9) of incisions for debridement and drainage.
Later histological examination of infected soft tissues revealed ischaemia or necrosis of superficial tissues (skin included in most cases), superficial and deep fascia and, in 6 cases of muscle fibers, thrombosis of feeding vessels or fibrinoid coagulation in the lumen of vessels, and polymorphic cell infiltration. True NF was confirmed in 18 cases, with 9 of them affected by Group A Streptococci (GAS), either alone or, mostly, in combination with other microbes. Wall thickness ischemic or necrotic changes were documented in all three colectomy specimens, in one case with a malignant anastomotic lesion (recurrence).
Fourteen Group I patients remained intubated and they were treated either in the Intensive Care Unit (ICU) (8 patients, with 2 intubated in ED included: 2 patients died within 72 hours, survivors stayed for 6-10 days/ mean 7.8) or into the High Dependency Unit (HDU) (6 patients: intubated for 2-3 days) for at least the initial postoperative period. Sepsis was never controlled in other 2 patients with extended perineal necrosis, which required colectomy or colostomy (one remained intubated). All others had a dramatic improvement of their clinical course soon after the primary necrectomy/debridement. Extubated patients were mostly treated in the general ward unless HDU was available. We continued intensive resuscitation and support to restore intravascular volume, maintain adequate end-organ perfusion and tissue oxygenation, and limit the adverse effect of end-organ dysfunction. The magnitude of resuscitation was dependent on the individual patient’s requirements and physiologic status. Blood transfusion was given to 12 survivors (2-6 units). Five patients underwent session of hemodialysis. Insulation in separate rooms for variable periods of time had been compulsory for 8 contagious patients after positive cultures during the course of their disease.
We initially used an empirical combination of IV antibiotics that cover a broad spectrum of aerobes, anaerobes, gram positive and gram negative bacteria. Our therapeutic regime usually consisted of Penicillin G or Ampicillin or 2nd/3rd generation Cephalosporin, Clindamycin, and Gentamycin or 3rd/4th generation Cephalosporin or Carbapenem. We monitored renal function with creatinine excretion when Aminoglycoside was used. Alternatively, to Penicillin, we sometimes replaced the whole regime by Piperacillin/Tazobactam/Aminoglycoside. We used Linezolid against possible Methicillin-resistant Staphylococcus aureus (MRSA) in 4 diabetics who were re-admitted for NSTI after a recent hospitalization for cardiorespiratory disease; administration was stopped in one after such infection had been excluded. Modulation of antibiotics and de-escalation to a more targeted therapy was later feasible, after Gram-staining result and microbiological identification of the pathogens. In all, 20 patients had polymicrobial infections, with those with perineal/anorectal origin of the infection having the greater number of bacteria (up to 5). Commonest isolated microbes were: GAS, Staphylococci (MRSA or community-associated MRSA, included), Enterococci, Klebsiella sp., Bacteroides sp., Escherichia coli, Pseudomonas aeruginosa and Proteus mirabilis (Table 3).
The management in immunocompromised patients differed in that it comprised an anti-fungal agent. In 4 patients, monomicrobial infection was documented and causative organisms were: GAS, MRSA and Clostridium perfringens. We continued the administration of the targeted therapy for 3-5 days after the systemic signs and symptoms and the most local signs of soft-tissue infection had been resolved. In survivors, targeted antibiotic therapy was administered for 10-18 days (mean, 15 days). Beyond that time, antibiotics were variably given for wound superinfection, nosocomial pulmonary or urinary infection, and as coverage in some wound reconstructions.
After index surgery, the resultant wounds were re-explored during the next 24 hours in the OR, under general anaesthesia in intubated patients and those with no clear improvement of their condition. Fifteen patients, all with perineal/urethral foci and one with lower extremity NF from Group I, underwent further 1-5 limited debridements or new incisions (mean, 2), under IV analgesia if non-intubated, during the first 8 days (mean, 4 days). Serial wound dressing changes -twice daily during the first 72 hours- were performed; open wounds were irrigated with hydrogen peroxide and saline and were covered with antibiotic dressing (povidone-iodine 1%). After stabilization of the wounds, we occasionally used agents such as silver nitrate or silver sulfadiazine; we applicated topical negative pressure (TNP) in non-perineal wounds.
Enteral feeding was preferred over parenteral nutrition, and it was provided after calculating caloric and protein requirements for patients with extensive open wounds and in hypermetabolic state. Vitamins A and C, and minerals were also given. Food orally was taken soon when the patient could tolerate it. Rehabilitation was started as soon as the patient was stable and able to participate. We stopped the postoperative anticoagulant/ antithrombotic treatment near the time of patients' mobilization and prescribed their medication on discharge from hospital.
In all, four chronic diabetics with prolonged sepsis and MODS at admission, who had the more extensive wounds that involved the perineum and who had undergone additional Hartmann’s colectomy (two patients, one with anorectal carcinoma recurrence) or loop sigmoidostomy (two patients, one with left thoracostomy) at index surgery died at 2nd, 3rd, 5th, and 16th day due to uncontrolled sepsis (overall mortality: 16.66%, mortality of cases with late findings: 22.22%). Complications were encountered in 11 survivors (55%): thrombophlebitis (8), atelectasis (5), urinary infection (4), residual wound superinfection (3), delayed MODS-corrected (2), partial autograft necrosis needing intervention (1), and chronic renal insufficiency (1).
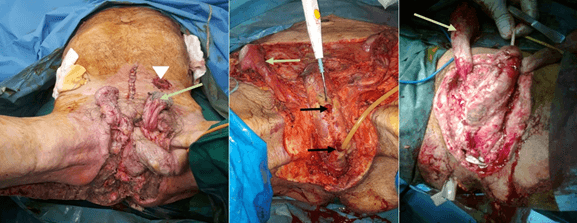
Figure 4: Reconstruction: Use of TNP in a woman with gluteofemoral NSTI/NF at 8th postoperative day (left: arrow shows extrapelvic drain tubes), and final result at 40th postoperative day in a patient with perineal- lower abdominal/ groin wound and denuded testicles (right: arrows show flap healing and covered testicles).
In survivors, closure of the residual tissue defects and “covering” of denuded organs (i.e., testicles) was a scheduled procedure during the initial admission (10 patients) or at planned re-admissions (10 patients). Applied simple to complex reconstructive methods included either repeat limited mobilization of wound edges and sectional suturing at week intervals (9 patients) or true plastic procedures after the formation of new granulation tissue (11 patients): creation of advancement pudendal-thigh (anterolateral) flaps (usually, bilateral), or local split-thickness skin grafts, component separation technique with restoration of abdominal wall function, and use of bioprosthetic mesh (Figure 4).
After initial admission, the mean hospitalization of survivors was 28 days (range, 12-46), with those with perineal/urogenic foci having the longer durations: 18-46 days vs 12-26 days for patients with infections on extremities, gluteus or trunk. After discharge, 12 patients were re-admitted for some days, either for planned residual wound reconstruction (10) and requested ostomy closure (1) or for surgical skin infection-disruption requiring intervention (1). All survivors were followed-up for at least one year after index surgery. No recurrence of NSTI/NF was encountered.
Discussion
Necrotizing infections are polymicrobial/synergistic in ~80% of cases (mostly, type I) and monomicrobial in ~20% [2, 5, 11]. NF, the worst of all NSTIs, has a reported incidence of 0.4 cases per 100.000 adults per year [2]. The present series comprises mostly septic patients with perineal and/or urogenic focus of inflammatory origin. Patients of this group had greater number of bacteria and they had larger and more composite tissue defects after the index surgery; survivors (all 4 deaths belonged to this group) required more operative procedures and longer hospitalization than patients with dermal foci. Actually, a subgroup of diabetic patients with extended affected areas involving the perineum, external genitalia, lower abdominal wall, and upper thigh(s), originating from non-clearly identified inflammatory focus, either perineal/anorectal or genitourinary, had the worse prognosis. It has been postulated that infecting bacteria in these difficult cases are probably passing through the Buck’s fascia of penis and spreading along the Darto’s fascia of penis and scrotum, the Colle’s fascia of perineum, and the Scarpa’s fascia of the lower abdominal wall [2, 6, 7, 9, 11, 19].
NSTI/NF remains associated with a heavy mortality, despite the improvement in critical care, usage of broad spectrum and targeted antibiotics, and the aggressive surgical debridement. However, over the last fifteen years, mortality has decreased to 13%-43% in reported series [2-5, 8, 20-23]. The mortality rate in our cohort (16.66%) compares favourably with the combined published mortality rate. Unfavourable outcome is affected by the delayed or inadequate index surgery, the degree of MODS on admission (delay in presentation), the high virulence of certain bacteria and the presence of severe concomitant illness[ 2, 6, 7, 16, 19, 22-27]. The relative risk of death was 7.5 times greater with improper primary necrectomy in the study of Mock et al. [24], and it was 9 times greater when index surgery was delayed more than 24 hours in the study of Wong et al. [23]. The multivariate analysis in the series of Jerraya et al. [19] retained the extension of gangrene beyond the perineum as an independent predictive factor of mortality (p=0.004). This was a clear observation in our present cohort, as it was the delayed presentation in our previous relative research [28, 29]. We also maintain that diabetics, representing half of our patients, mostly presented with delay, associated with all cases of unfavourable outcome, appear to be particularly at greater risk. Amputations (“guillotine” type) are sometimes inevitable for patients when the affected limb is not viable or not expected to be functional after the debridement [4, 8, 22]. Fortunately, in this series, we haven't been confronted with such a necessity. Awareness is advocated in patients with sudden onset and rapid progression of a suspected soft-tissue infectious disease [3, 5, 16, 22]. A meticulous physical examination and a clear understanding of the clinical picture have paramount importance in establishing an early diagnosis of NSTI or NF [2, 3, 11, 16-18, 22]. Early clinical findings generally emphasized are the swelling-erythema with tenderness and disproportional pain [5]. Only 6 (25%) of our patients were presented early in the course of their disease. However, in the early phase, the spread and extent of infection do not correspond with the overlying skin changes, the clinical diagnosis may be ambivalent, and the unskilled surgeon might not clearly determine the seriousness of a progressed disease that takes place under the skin and into the subcutis. On the other hand, the hallmark symptoms of prolonged NF, especially on the perineum and extremities, include intense pain and tenderness over the involved skin and underlying muscles [2]. With either the presence of obvious skin necrosis or not, the presence of tissue crepitus (encountered in more than half of all NF cases) or skin anaesthesia (due to destruction of cutaneous nerves) are late findings of more severe disease [22]. Concluding, the diagnosis of NSTI/NF relies on clinical findings which, however, can further be supplemented by clinical and laboratory scores such as the Fournier's Gangrene Severity Index and the LRINEC score [2, 3, 5, 7, 9, 17, 22]. Imaging is important for diagnosis in equivocal cases and for assessment of infection extent and severity [2, 5, 6, 17, 22].
The suggested approach is that sepsis is treated immediately according to the Surviving Sepsis Campaign Guidelines [30]. Intentionally, Infectious Diseases Society of America (IDSA) guidelines support prompt and aggressive wide surgical excision of infected tissue, accompanied by appropriate antibiotic therapy [31]. Many investigators postulated that encouraging recovery, especially of the more severe cases with NF affecting large body areas, and favourable final outcome are positive only after a multidisciplinary approach [2, 5, 11, 15, 22, 26]. Contemporary dilemmas about how long to use antibiotics also exist [2, 4, 8, 22]. TNP therapy for large wounds has been reported to securely remove exudates, reduce bacterial contamination, and promote better healing, and we support its use [2]. Finally, although well-conducted trials evaluating the efficacy of IV immunoglobulins (i.e., for GAS infection) and hyperbaric oxygen (i.e., for Clostridia) are lacking, scattered case reports and observational studies show no obvious survival benefit to therapy [2, 5, 22].
In our study, the polymicrobial infection identified by wound cultures was the dominant cause of either the NSTI or NF. Our therapeutic regime covered a broad spectrum of anaerobes and Gram-positive and Gram-negative organisms; repeat culture results with sensitivities to antibiotics guided further appropriate adjustment to more targeted treatments. Importantly, we never delayed the index surgical necrectomy/debridement in the fraudulent hope of correcting firstly hemodynamic instability, because septic state reversal will not occur until all of the infected and necrotic tissues have been timely removed. Time to wait for the first surgery ranges from 3 hours to 36 hours in the existing literature [2, 5, 18, 22, 32]. In this series, rapid improvement after the earliest (within 4 hours) and the as widest as possible index necrectomy was observed in all but four of our patients, besides that survivors required some repeat further limited excisions or new incisions. The clinical course of the infection was never improved in four patients with much delay in presentation and the worst necrosis beyond the perineum, who had a colectomy or colostomy at index surgery, had undergone additional serial debridements, but finally died due to uncontrolled sepsis. Practice guidelines for best management of NSTI/NF after initial necrectomy/debridement and administration of antibiotics do not exist [2, 4, 5, 9].
Conclusion
High index of suspicion is the prerequisite for an early clinical diagnosis of NSTI/NF, which is especially challenging in ambivalent cases with minimal local signs. Awareness is advocated in patients with sudden onset and rapid progression of a suspected soft-tissue infectious disease. Clinical physical examination, coupled with cultures, imaging and surgical exploration may confirm the initial suspicion. The treatment of NSTI/NF is multidisciplinary. It is initiated promptly, including intensive resuscitation, and supporting of the patient in shock, and simultaneous surgical radical excision of affected tissues and administration of wide-spectrum antibiotics. The mainstay of treatment entails an aggressive approach with extensive and, if required, repeated necrectomy/debridement to completely control the progressing sepsis in the soft tissues. Contributors for final favourable outcome are the close wound care, the de-escalation to targeted antibiotic therapy after culture results, the nutritional support, the appropriate rehabilitation, and the timely plastic reconstruction to cover denuded organs and reconstruct residual tissue defects. Unfavourable outcome is affected by the delayed or inadequate index surgery, the degree of MODS on admission, and the severe concomitant illness.
Ethical Approval
The authors declare that the study has been approved by the Institutional Ethics Committee of the General Hospital of Nea Ionia “Constantopoulion-Patission”, Athens- Greece, and it is in accordance with the ethical standards.
Consent
A written informed consent was obtained from individual participants included in the study; a close relative or legal guardian has signed in case of intubated patients who died.
Availability of Data and Materials
Further information is available from the corresponding author on reasonable request.
Competing Interests
None.
Author Contributions
CA was responsible for the emergent operations and perioperative management, he conceptualized the study, and he is the corresponding author; VK, PC and MS contributed to the treatment of patients and have taken part in designing the study, analyzing data, and interpreting the study results; ChA contributed to analysis of culture results and antibiotics used, as well as supported in documenting the article, drawing the conclusion, and preparing the manuscript.
Article Info
Article Type
Case SeriesPublication history
Received: Mon 18, Jan 2021Accepted: Mon 01, Feb 2021
Published: Mon 15, Feb 2021
Copyright
© 2023 Constantinos Avgoustou. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.02.13
Author Info
Constantinos Avgoustou Periklis Constantinou Christina Avgoustou Karampas Vasilios Maria Sioula
Corresponding Author
Constantinos AvgoustouDepartment of Surgery, General Hospital of Nea Ionia Constantopoulion-Patission “Aghia Olga”, Athens, Greece
Figures & Tables
Table 1: Risk factors for development of infection and initiating pathologic conditions in 24 patients with NSTI/NF.
|
Preexisting conditions |
No of patients |
|
|
Advanced age (>65 years) Diabetes mellitus Hypertension under medication Chronic pulmonary disease Peripheral vascular disease Congestive heart disease Obesity Malnutrition Chronic alcoholism Active IV drug use, steroid use/ immunocompromised status Malignancy |
8 12 6 4 7 2 6 3 2 3
1 |
|
|
Initiating pathologic conditions |
No of patients |
|
|
Perineal abscess or chronic anal fistula/fissure Periurethritis/epididymoorchitis after instrumentation(urethral rupture) Post-hemorrhoidectomy wound infection Anorectal carcinoma (anastomotic recurrence) Bartholin’s cyst abscess Tibial chronic vascular ulcers-sinuses(assoc. compartment syndrome in 2) Abscess after IM/IV injections (2 immunocompromised) |
8
6
1 1
1 |
Anorectal- genitourinary foci |
|
4
3 |
Dermal foci |
|
Table 2: Main local physical-clinical findings in 24 patients with NSTI/NF.
|
Late findings – Group I patients |
Early findings – Group II patients |
* LRINEC score ≥6 - 6 patients >8 - 12 patients |
* LRINEC score 5 - 3 patients 6 - 3 patients |
Table 3: Origin/type of infection and systemic manifestations in 24 patients with NSTI/NF.
|
Infectious origin: Affected area/ Depth |
Severe systemic manifestation: No of patients |
Type of infection: No of patients |
|
|
Anorectal, Urogenic:
|
Skin, fascia
|
|
Polymicrobial/Type I: 17 patients
|
|
Dermal wound (bite?):
|
Skin, fascia
|
|
Polymicrobial/Type I: 3 patients
|
|
Dermal wound-IM/IV drug abuse:
|
Skin, fascia, muscle
|
|
Monomicrobial/Type II: 2 patients
|
|
Dermal wound- IM/IV drug abuse:
|
Fascia, muscle |
|
Monomicrobial/Type III: 2 patients
|

References
- Descamps V, Aitken J, Lee MG (1994) Hippocrates on necrotising fasciitis. Lancet 344: 556. [Crossref]
- Roje Z, Roje Z, Matić D, Librenjak D, Dokuzović S et al. (2011) Necrotizing fasciitis:literature review of contemporary strategies for diagnosing and management with three case reports: torso, abdominal wall, upper and lower limbs. World J Emerg Surg 6: 46. [Crossref]
- Hietbrink F, Bode LG, Riddez L, Leenen LP, Dijk MRV (2016) Triple diagnostics for early detection of ambivalent necrotizing fasciitis. World J Emerg Surg 11: 51. [Crossref]
- Faraklas I, Yang D, Eggerstedt M, Zhai Y, Liebel P et al. (2016) A Multi-Center Review of Care Patterns and Outcomes in Necrotizing Soft Tissue Infections. Surg Infect 17: 773-778. [Crossref]
- Cocanour CS, Chang P, Huston JM, Adams CA Jr, Diaz JJ et al. (2017) Management and Novel Adjuncts of Necrotizing Soft Tissue Infections. Surg Infect 18: 250-272. [Crossref]
- Weimer SB, Matthews MR, Caruso DM, Foster KN (2017) Retroperitoneal Necrotizing Fasciitis from Fournier's Gangrene in an Immunocompromised Patient. Case Rep Surg 2017: 5290793. [Crossref]
- Chernyadyev SA, Ufimtseva MA, Vishnevskaya IF, Bochkarev YM, Ushakov AA et al. (2018) Fournier's Gangrene: Literature Review and Clinical Cases. Urol Int 101: 91-97. [Crossref]
- Hua C, Bosc R, Sbidian E, De Prost N, Hughes C et al. (2018) Interventions for necrotizing soft tissue infections in adults. Cochrane Database Syst Rev 5: CD011680. [Crossref]
- Izadi D, Coelho J, Gurjal S, Salim F (2016) Fournier's Gangrene and the Reconstructive Challenges for the Plastic Surgeon. Eplasty 16: ic38. [Crossref]
- Mills MK, Faraklas I, Davis C, Stoddard GJ, Saffle J (2010) Outcomes from treatment of necrotizing soft-tissue infections: results from the National Surgical Quality Improvement Program database. Am J Surg 200: 790-796. [Crossref]
- Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJC et al. (2014) Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis 59: 147-159. [Crossref]
- Kincius M, Telksnys T, Trumbeckas D, Jievaltas M, Milonas D (2016) Evaluation of LRINEC Scale Feasibility for Predicting Outcomes of Fournier Gangrene. Surg Infect 17: 448-453. [Crossref]
- Stamenkovic I, Lew PD (1984) Early recognition of potentially fatal necrotizing fasciitis. The use of frozen-section biopsy. N Engl J Med 310: 1689-1693. [Crossref]
- Sarani B, Strong M, Pascual J, Schwab CW (2009) Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg 208: 279-288. [Crossref]
- Hakkarainen TW, Kopari NM, Pham TN, Evans HL (2014) Necrotizing soft tissue infections: review and current concepts in treatment, systems of care, and outcomes. Curr Probl Surg 51: 344-362. [Crossref]
- Goh T, Goh LG, Ang CH, Wong CH (2014) Early diagnosis of necrotizing fasciitis. Br J Surg 101: e119-e125. [Crossref]
- Fernando SM, Tran A, Cheng W, Rochwerg B, Kyeremanteng K et al. (2019) Necrotizing Soft Tissue Infection: Diagnostic Accuracy of Physical Examination, Imaging, and LRINEC Score: A Systematic Review and Meta-Analysis. Ann Surg 269: 58-65. [Crossref]
- Chen KJC, Klingel M, McLeod S, Mindra S, Ng VK (2017) Presentation and outcomes of necrotizing soft tissue infections. Int J Gen Med 10: 215-220. [Crossref]
- Jerraya H, Fehri H, Khalfallah M, Abdesselem MM, Dziri C (2015) Predictive factors of mortality in Fournier's gangrene. Tunis Med 93: 800-803. [Crossref]
- Swain RA, Hatcher JC, Azadian BS, Soni N, Souza BD (2013) A five-year review of necrotising fasciitis in a tertiary referral unit. Ann R Coll Surg Engl 95: 57-60. [Crossref]
- Stigt SFLV, Vries JD, Bijker JB, Mollen RMHG, Hekma EJ et al. (2016) Review of 58 patients with necrotizing fasciitis in the Netherlands. World J Emerg Surg 11: 21. [Crossref]
- Garcia NM, Cai J (2018) Aggressive Soft Tissue Infections. Surg Clin North Am 98: 1097-1108. [Crossref]
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL et al. (2003) Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 85: 1454-1460. [Crossref]
- Mock MY, Wong SY, Chan TM, Tang WM, Wong WS et al. (2006) Necrotizing fasciitis in rheumatic diseases. Lupus 15: 380-383. [Crossref]
- Sartelli M, Malangoni MA, May AK, Viale P, Kao LS et al. (2014) World Society of Emergency Surgery (WSES) guidelines for management of skin and soft tissue infections. World J Emerg Surg 9: 57. [Crossref]
- Park SJ, Kim DH, Choi CI, Yun SP, Kim JH et al. (2016) Necrotizing soft tissue infection: analysis of the factors related to mortality in 30 cases of a single institution for 5 years. Ann Surg Treat Res 91: 45-50. [Crossref]
- Fais P, Viero A, Viel G, Giordano R, Raniero D et al. (2018) Necrotizing fasciitis: case series and review of the literature on clinical and medico-legal diagnostic challenges. Int J Legal Med 132: 1357-1366. [Crossref]
- Avgoustou C, Foroulis C, Constantinou M, Zormbas J (1997) Surgical management of acute suppurative mediastinitis. Br J Surg 84 Suppl 2: 147.
- Avgoustou C, Coniaris H, Skevis C, Penlidis P, Triantopoulou Ch et al. (2003) Fournier’s gangrene and soft-tissue necrotizing infections of perineum and external genitalia. In: Papaevangelou E, Karaliotas C, editors. Evolutions in Surgery 2002. Innovating diagnostic and therapeutic approaches. Athens Greece: Synedron; 112-115].
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H et al. (2013) Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41: 580-637. [Crossref]
- Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P et al. (2005) Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis 41: 1373-1406. [Crossref]
- Gelbard RB, Ferrada P, Yeh DD, Williams BH, Loor M et al. (2018) Optimal timing of initial debridement for necrotizing soft tissue infection: A Practice Management Guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 85: 208-214. [Crossref]
