Neurosurgical Presentations of Neurofibromatosis Type 1: Our Experience in a Regional Neurosurgical Centre, Sokoto, Nigeria
A B S T R A C T
Objective: The objective of this paper was to highlight various neurosurgical presentations of patients with neurofibromatosis type 1 seen in our center.
Design: This is retrospective analysis of all cases of neurofibromatosis type 1 seen in our neurosurgical center over five- year period. Data was extracted from case files retrieved from medical records department of the hospital. Biodemographic characteristics, clinical presentations, neuroimaging findings and treatment offered were noted.
Setting: A single center report conducted at department of neurosurgery, regional neurosurgical center, Usmanu Danfodiyo university teaching Hospital Sokoto.
Participants: All patients presenting to neurosurgery department with a diagnosis of neurofibromatosis type 1 over five-year period.
Interventions: Among the patients seen, three had surgical intervention for disfiguring plexiform neurofibroma. While the remaining two patients refused any form of surgery. Cosmesis was main study outcome which was satisfactory to both the surgeons and the patients.
Results: We found a total of five cases managed over the study period. Three males and two females, the youngest was 2 weeks old while the oldest was a 22-year-old man. Three patients had major cranial lesions while two presented with spinal/paraspinal lesions. Also, only three patients met NIH criteria for the diagnosis of NF-1, two presented with only plexiform neurofibromatosis. Two patients declined any form of surgical intervention. Cosmesis was the only reason for presenting to the hospital. Postoperative outcome was good for the three patients that accepted surgery.
Conclusion: Neurofibromatosis type 1 occurs at a rate of one case per year in our setting. Various cranial and spinal/paraspinal manifestations were observed.
Keywords
Neurofibromatosis type 1, neurosurgical presentations, plexiform neurofibroma
Introduction
Neurofibromatosis type 1 is a genetic and neurocutaneous disorder affecting multiple systems in the body [1-3]. This autosomal dominant condition is seen in one in 2000-4500 individuals, half of all cases result from new mutation and half has familial tendency [3, 4]. The incidence of neurofibromatosis type 1 was reported to be on the rise in Nigeria [5]. Development of NF 1 has been linked to a defective gene on chromosome band 17q11.2, when expressed, produces protein neurofibromin which has been demonstrated to serve as tumor suppressor [4, 6, 7]. Neurofibromin functions as Ras-negative regulator by increasing the hydrolysis of Ras-bound GTP [8]. When there is absence or dysfunction of neurofibromin, Ras is constantly bound to GTP and the pathway is hyper-activated, thereby causing deregulated cellular proliferation and survival [8]. Up-regulation of Ras triggers downstream signalling pathways, including the mitogen-activated protein kinase (MAPK) RAF/MEK/ERK pathway, which is associated with tumorigenesis [8]. The diagnosis of neurofibromatosis had been based on clinical criteria established in 1987 by the American National institute of Health (NIH) [8, 9]. A diagnosis is made when there are at least two major criteria listed below [9, 10]:
i. More than 6 café au lait spots >5 mm in greatest
ii. diameter (>15 mm in post-pubertal patients)
iii. Two or more neurofibromas of any type or one
iv. plexiform neurofibroma (PNF)
v. Axillary or inguinal area freckling
vi. Optic glioma
vii. Two or more lisch nodules of the iris
viii. Distinctive osseous lesions, for example, sphenoid
ix. dysplasia and pseudoarthrosis
x. First-degree relative with NF-1 as diagnosed by above
xi. criteria.
Also, presence of minor criteria would support the diagnosis: small stature, macrocephaly, scoliosis, pectus excavatum, hamartomas and neuropsychological abnormalities (Table 1) [10]. Neurofibromatosis type 1 has no predilection for race, but several studies reported different findings in terms of gender preference, some found male preponderance while others revealed no difference in occurrence across gender. neurofibromatosis can be seen in both children and adults [4, 11, 12]. Neurofibromatosis is a multisystemic disease, therefore requires multidisciplinary approach in the management.
Rare diseases like neurofibromatosis are somewhat considered orphans of medicine and receive little or no attention. There is dearth of information on neurosurgical presentations of neurofibromatosis in literature especially in Africa, it is believed that this paper shall provide more information on this condition in Nigeria and Africa at large.
Aim
This paper aims to illustrate a number of unusual cranial and spinal neurofibromatosis seen in our neurosurgical center.
Materials/Subjects and Methods
We retrospectively reviewed all cases of neurofibromatosis presenting to our regional neurosurgical center over five-year period (July 2015 to June 2020). Relevant data like age, gender, clinical features and treatment outcome were extracted from patients ‘case files retrieved from hospital’s medical records department.
Results
We had a total of five cases over the study period. Three males and two females, the youngest was 2 weeks old while the oldest was a 22-year-old man Table 1).
Table
1: Profile
of the cases.
|
Number |
Age |
Gender |
Main presenting feature(s) |
Other presenting features |
treatment |
outcome |
Follow up |
|
1 |
2 weeks |
Female |
Lumbosacral plexiform NF**. |
Multiple café au lait macules. |
Excision of PNF*. |
Good. |
Regular (now 3year old). |
|
2 |
4
year |
Male
|
Left
proptosis |
Ipsilateral
temporo-orbital swelling, Multiple
café au lait spots. |
Parents
declined any form of treatment |
- |
Lost
to follow up. |
|
3 |
12 year |
Female |
Right temporal scalp PNF* |
Kyphoscoliosis, multiple café au lait
spots |
Parents declined any form of treatment |
- |
Lost to follow up. |
|
4 |
16
year |
Male
|
Occipital
PNF* |
Nil
|
Total
excision |
Good |
Regular
on follow up |
|
5 |
22 year |
Male |
Paramedian lumbo-sacral PNF* |
Nil |
Total excision |
good |
Lost to follow up |
Key: * plexiform neurofibroma, **
neurofibromatosis.
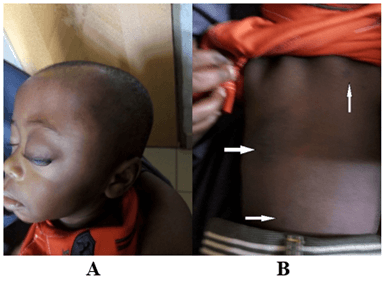
Figure 1: A neonate with lumbosacral PNF and hyperpigmented macule.
Figure 2: Excised PNF.
Figure 3: A) A child with left proptosis and temporo-orbital swelling. B) Multiple café au lait spots.
Figure 4: Superior arrow shows right temporal PNF, other arrows show hyperpigmented macules.
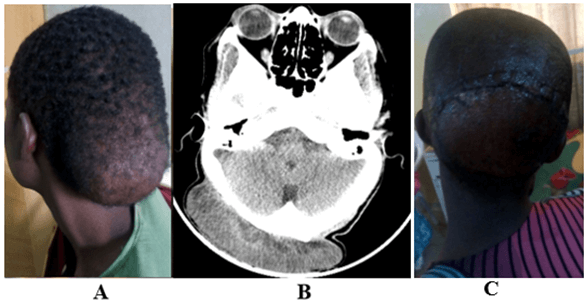
Figure 5: A) Occipital PNF. B) Axial slice CT scan showing occipital soft tissue swelling. C) post-operative photograph of patient with occipital PNF (Figure 5A).
Figure 6: A 22-year-old man with lumbosacral ulcerated PNF.
Discussion
Neurofibromatosis remains a multisystemic disease affecting all ages irrespective of ethnic or racial background [4, 8, 13]. We recorded five cases of neurofibromatosis with varied presentation over five-year period. Age ranges from 2 weeks to 22 years of life with slight male predominance. As reported in the literature most cases of neurofibromatosis appear from birth to adolescent age and males are commonly affected [4, 11, 14]. In contrast, some authors reported no sex predilection [9, 11]. The diagnosis of neurofibromatosis had been based on clinical criteria established by national institute of health (NIH) where two more of the features described by the NIH are present to make diagnosis of NF 1 [8]. The sensitivity and specificity of NIH criteria are high and adequate to diagnose half of the affected patients in the first one year and 95% by the age of eight years [8]. In the index paper, only three of the patients satisfied the NIH criteria (Figures 1-4), the other two presented with only plexiform neurofibromatosis (Figures 5 & 6). Questions may be raised on whether or not plexiform neurofibromatosis is pathognomonic of NF1. Some Authors believe that plexiform neurofibromatosis is indicative of NF 1, while others are insisting on following the NIH criteria and are of the opinion that plexiform neurofibromatosis is not pathognomonic of NF 1 but a feature of it [6]. For us, we would stay at the middle and follow up our patients as long as possible to see whether those with only plexiform neurofibroma would develop the full-blown disease or not.
Plexiform neurofibroma develops in about fifty percent of persons with neurofibromatosis 1 and accounted for the major disability and disfigurement seen in individuals with NF 1 [15, 16]. PNF could transform to malignant peripheral nerve sheath tumor and is one of the main causes of death among NF 1 patients [16, 17]. As seen in our first case, plexiform neurofibromatosis may appear at birth or diagnosed during the first year of life in 30% of individuals with NF1 [14]. Similar to other studies, the management of plexiform neurofibromatosis is mainly surgical excision as done in three patients in this series, two patients declined surgery [14]. The aim of the surgery was for cosmesis, none of the patients had any other symptoms.
Conclusion
Neurofibromatosis type 1 occurs at a rate of one case per year in our setting. Patients present in different forms, with a slight male preponderance. Three of the patients had major lesion on the head while two presented with spinal and paraspinal lesion. Only three in our series satisfied the NIH criteria, other two presented with only plexiform neurofibroma. The believe or not that plexiform neurofibroma is pathognomonic of neurofibromatosis type 1 awaits further clinical and genetic studies on this subject matter to settle the unending controversy.
Article Info
Article Type
Research ArticlePublication history
Received: Thu 24, Nov 2022Accepted: Mon 12, Dec 2022
Published: Sat 31, Dec 2022
Copyright
© 2023 Aliyu Muhammad Koko. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.NNB.2022.04.04
Author Info
Aliyu Muhammad Koko Ali Lasseini
Corresponding Author
Aliyu Muhammad KokoDepartment of neurosurgery, regional centre for neurosurgery Usmanu Danfodiyo University Teaching Hospital Sokoto, Nigeria
Figures & Tables
Table
1: Profile
of the cases.
|
Number |
Age |
Gender |
Main presenting feature(s) |
Other presenting features |
treatment |
outcome |
Follow up |
|
1 |
2 weeks |
Female |
Lumbosacral plexiform NF**. |
Multiple café au lait macules. |
Excision of PNF*. |
Good. |
Regular (now 3year old). |
|
2 |
4
year |
Male
|
Left
proptosis |
Ipsilateral
temporo-orbital swelling, Multiple
café au lait spots. |
Parents
declined any form of treatment |
- |
Lost
to follow up. |
|
3 |
12 year |
Female |
Right temporal scalp PNF* |
Kyphoscoliosis, multiple café au lait
spots |
Parents declined any form of treatment |
- |
Lost to follow up. |
|
4 |
16
year |
Male
|
Occipital
PNF* |
Nil
|
Total
excision |
Good |
Regular
on follow up |
|
5 |
22 year |
Male |
Paramedian lumbo-sacral PNF* |
Nil |
Total excision |
good |
Lost to follow up |
Key: * plexiform neurofibroma, **
neurofibromatosis.




References
1.
North K (1993)
Neurofibromatosis type 1: review of the first 200 patients in an Australian
clinic. J Child Neurol 8: 395-402. [Crossref]
2.
Karnes PS (1998)
Neurofibromatosis: a common neurocutaneous disorder. Mayo Clin Proc 73:
1071-1076. [Crossref]
3.
DeBella K, Szudek
J, Friedman JM (2000) Use of the national institutes of health criteria for
diagnosis of neurofibromatosis 1 in children. Pediatrics 105: 608-614. [Crossref]
4.
Odebode TO, Afolayan
EAO, Adigun IA, Daramola OOM (2005) Clinicopathological study of
neurofibromatosis type 1: an experience in Nigeria. Int J Dermatol 44:
116-120. [Crossref]
5.
Anyabolu EN (2019)
Lumbar plexiform neurofibroma, short stature, and kyphoscoliosis in
neurofibromatosis-1: A rare entity. Sahel Med J 22: 153-156.
6.
Lin V, Daniel S,
Forte V (2004) Is a plexiform neurofibroma pathognomonic of neurofibromatosis
type I? Laryngoscope 114: 1410-1414. [Crossref]
7.
Onunu AN, Lawal NA
(2002) Neurofibromatosis 1: A Clinical Study In The Nigerian African. Ann
Biomed Sci 1: 118-123.
8.
Shofty B,
Constantini S, Shachar SB (2015) Advances in Molecular Diagnosis of Neurofibromatosis
Type 1. Semin Pediatr Neurol 22: 234-239. [Crossref]
9.
Nyandati YW, Tahir
C, Nggada HA, Ndahi AA (2009) Clinico-Pathologic Presentation and Management of
neurofibromatosis type 1(Von Recklinghausen's) Disease among North-Eastern
Nigerians: A six year review. Niger Med J 50: 80-83.
10.
Ehigiamusoe FO,
Ogbeide E (2017) Neurofibromatosis with pulsating exophthalmos. Port
Harcourt Med J 11: 99-102.
11.
Obringer AC,
Meadows AT, Zackai EH (1989) The diagnosis of neurofibromatosis-1 in the child
under the age of 6 years. Am J Dis Child 143: 717-719. [Crossref]
12.
Otibi MA, Rutka JT
(2006) Neurosurgical implications of neurofibromatosis Type I in children. Neurosurg
Focus 20: E2. [Crossref]
13.
Alhadef HT, Mautner
VF, Gugel I, Zipfel J, Lude KH et al. (2020) Role, function and challenges of
multidisciplinary centres for rare diseases exemplified for neurofibromatosis
type 1 syndrome. Childs Nerv Syst 36: 2279-2284. [Crossref]
14.
Mersal AY, Hassan
AA, Alardati HA, Harthi AA, Avand G (2012) Congenital Neurofibromatosis in a
Saudi Neonate who Presented with Neck Mass, Esophageal and Airway Obstruction. J
Clin Neonatol 1: 214-216. [Crossref]
15.
Joshi A, Lancelot
M, Bhattacharjee NR, Polavarapu S, Beltaos E et al. (2015) Extensive plexiform
neurofibroma in a premature neonate. Clin Med Res 13: 36-40. [Crossref]
16. Korf BR (1999) Plexiform neurofibromas. Am J Med Genet 89: 31-37. [Crossref]
17. Gutmann DH, Aylsworth A, Carey JC, Korf B, Marks J et al. (1997) The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. JAMA 278: 51-57. [Crossref]
