New Horizons for Observation of Patients with the Bladder Cancer Associated with Schistosoma haematobium Invasion
A B S T R A C T
Background and Purpose: The aim of the study was to improve the diagnostic and treatment approach for the medical care for patients with Schistosoma-associated bladder cancer (SA-BC).
Material and Methods: The survey results the study of 56 patients with gross hematuria in medical institutions of the Province Benguela (Angola) since 2007 to 2012. Group A (n=35) included patients before applying the standardized diagnostic algorithm. Group B (n=21) included patients using the new organizational format, in hospital outpatient’s.
Results: The progression to locally advanced stage of SA-BC was verified at significantly higher rate (80%). In patients from group A, while verified locally advanced SA-BC stays at low level (66,7%) in group B.
Conclusion: The combined usage of urine cytology test, ultrasonography and cystoscopy at the increased proliferative process caused by Schistosoma haematobium (SH) allows to reveal diagnose SA-BC in early stages, subject to on condition of patient’s admission in hospital outpatient care structures of specialized medical institutions.
Keywords
Schistosoma haematobium, schistosoma-associated bladder cancer, radical cystectomy, hospital outpatient’s, short-term hospital
Introduction
The urogenital schistosomiasis (UGS) is extremely widespread around the world, taking the second position after malaria [1]. Out of 243 million people with the proved UGS, more than a half of the cases are caused by infection of Schistosoma haematobium (SH), the parasite,that lives in water sources on the territory of Africa and the Middle East countries: he gets into bodies of an urogenital system of the person with infection, that leads to development of a disease [2]. The SH eggs which have been kept in a human body cause the appearance of specific granulomas and cankers on a mucous membrane of a bladder that promotes obstruction of ureters, the ascending infection of the upper urinary tract, a hydronephrosis and a renal failure [3]. The chronical effect of SH eggs on tissue of an urothelium causes the development of the specific schistosoma-associated bladder cancer (SA-BC), that is considered as "squamous cell carcinoma of the bladder" by pathologists in most cases.
The data of world scientific literature demonstrate that SA-BC is often diagnosed in the neglected disease stages, with a low stage of a differentiation of a tumor. Metastasis frequency of SA-BC does not exceed 18% that it is much less, than in patients with transitional cell bladder cancer [4].
The treatment conditions of the population living in the provinces with SA-bladder cancer are significantly different from those of urban residents. At the same time, residents of small towns and rural areas make up 55.18% of the total population of Angola. The results of medical care in bladder cancer are determined not only by the causes of the ecological, geographical, social and domestic plan, but to a considerable degree by medical and organizational factors. Unfortunately, specialized medical algorithm and postoperative care for many patients with SA-BC are not available. Study of the opportunities of improvement the quality of diagnostics and medical care in UGS patients, which are a risk factor for evolution of SA-BC, remains a relevant cross-disciplinary task.
Background and Purpose
The aim of the study was to improve the diagnostic and treatment approach for the medical care for patients with Schistosoma-associated bladder cancer (SA-BC).
Material and Methods
The survey results of 56 patients with gross hematuria attended in medical institutions of the province Benguela (Republic Angola) since 2007 to 2012. Most of the patients were from rural areas - 49 (87.5%), the number of citizens was 7 (12.5%). All patients participating in the study reported episodes of the use of crude fresh water in everyday life (drinking, cooking, washing, etc.). Patients are distributed in 2 groups A and B. Group A included 35 patients before applying the standardized diagnostic algorithm, (observation period from 2007 to 2009): 5 (14,3%) patients with tumor pathology not related to UGS and 30 (85,7%) SA-BC patients. Group B included 21 patients using the new organizational format (follow-up from 2009 to 2012): UGS and SA-BC was detected in 4 (19,1%) and in 14 (66,7%) cases respectively, 3 (14,3%) cases gross hematuria was not associated with UGS. All our diagnostic and therapeutic actions, including new ones, were approved by the members of the local ethics committee.
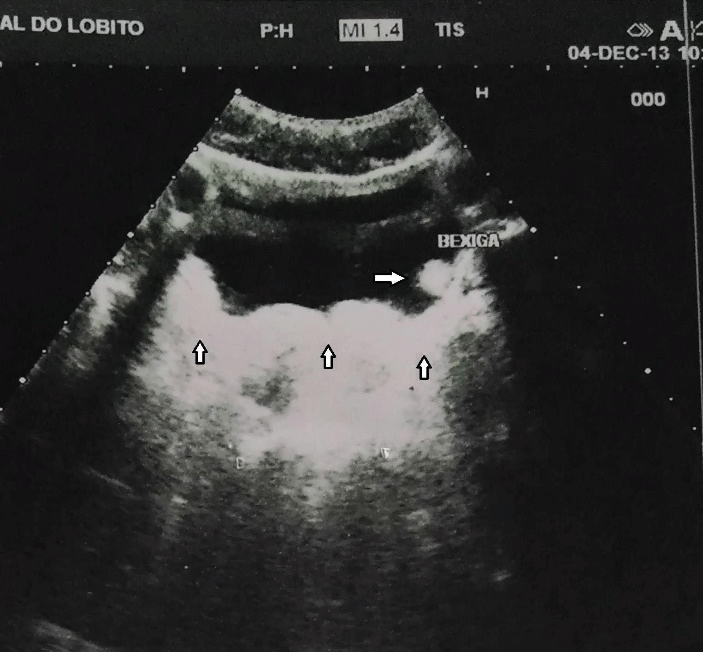
Figure 1: Ultrasound picture of the patient Z., 35 y.o. with gross hematuria and thickness of the bladder wall (marked) with schistosoma’s granulomas.
Results
Observation results of A group patients (n=35; 19 women and 16 men, middle age 35.4±4.2 years) estimated retrospectively. The duration of hematuria in patients of this group ranged from 3 weeks to 12 months. The unified algorithm of diagnostics and treatment of patients with UGS and SA-BC has not been implemented yet in that time. Patients with blood in the urine appealed to medical institutions at various levels. A standard approach UGS treatment in the region was a urine test followed by treatment with Praziquantel 40 mg/kg (according to WHO international recommendations). Patients have gone home after stopping of a gross hematuria. In case of continued hematuria additional examination has been conducted in a hospital of the regional level, where they were examined and received treatment by MD therapist. When stopping bleeding, of the patient allowed to go home. At inefficiency of therapy the patient directed to the urologist.
The urologist has appointed standard observation with the urine cytology, ultrasound examination of abdominal organs (Figure 1) and a lower pelvis, cystoscopy with a "random" biopsy (in the presence of changes of a wall of a bladder according to ultrasonography). The excretory urography and the computer tomography of abdominal organs, lower pelvis and urinary tract have been carried out according to indications. When a bladder tumor was detected, the patient was sent to the hospital for performing the surgical treatment.
Prostate tumor or malignant neoplasms of female’s genitalia were revealed at 5 (14.3%) patients in group A. We verified SA-BC after surgical treatment: a case (2.9%) of non-muscle-invasive SA-BC in stage pT1N0M0 (an open resection of the bladder), 28 (80%) cases of locally-spread SA-BC in stages рТ3-4N0-3M0-1 (radical cystectomy with various types of urine derivation in 23 cases or an ureterocutaneostomy). One (2.9%) patient came to a hospital from a maternity home, at 37 weeks of pregnancy. Squamous-cell bladder cancer (BC) confirmed histologically in all cases, Schistosoma eggs were revealed.
There were 21 persons (13 women and 8 men at the age of 30±3.4 years) in group B, with gross hematuria have last from 1 week up to 2 months. The plan of observation has been corrected: patients with the first time revealed gross hematuria have been directed to the urologist of the short-term hospital (STH), the structural division of regional level hospital. From the moment of admission, the patient has been conducted specialized examination with use of tool of diagnostic methods in STH: the urine test with microscopic analysis of urine sediment, ultrasonography of abdominal organs and lower pelvis. The cystoscopy with a "random" biopsy of an urothelium or, according to indications after ultrasonography, diagnostic operation – transurethral resection of the bladder tumor (TURBT) has been included in the obligatory list of tests. The excretory urography and/or a computer tomography of abdominal organs, lower pelvis and urinary tract has been carried out additionally, at emergence of suspicion of pathology of the upper urinary tract and obstruction of ureters. The organization of specialized observation of the patient in STH of regional hospital, with participation of the qualified doctor-urologist is an advantage of this method.
The renal colic, complicated by a gross hematuria has been revealed at one patient (4.8%), the prostate cancer with germination in a bladder have been revealed at 2 patients (9.5%). An severe proliferative changes of a wall of a bladder caused by UGS have been verified at 4 patients (19.04%) and TURBT was executed. UGS confirmed by results of a histologic research – schistosoma eggs were found in the biopsy specimen, malignant cells were not found. The diagnosis established as "SA-BC pT1-2N0M0" at 14 patients (66.7%): TURBT has been carried out to 5 patients, an open segmented cystectomy has been executed to 9 patients (including three pregnant women in the third trimester of pregnancy). The existence of schistosoma eggs confirmed in 28.2% of cases during urine test. Specific changes for SA-BC and UGS, by results of ultrasonography and cystoscopy, revealed in all cases: it has been proliferative exophytic formations of a bladder (the size> of 1.5 cm). The combination of beam and endoscopic methods has allowed to diagnose a disease for patients of B group and define indications for endoscopic (TURBT) or open surgical interventions.
Indicators of the general status of SA-BC defeated (Karnowsky scale and ECOG Performance Status) has not differ significantly: all patients are at working-age, with a minimum list of associated diseases. Therefore, the general status of patients is not defining for choosing a method of treatment: Karnowsky index was 90 ± 8.5 and 80 ± 4.7, respectively, and the ECOG index – 0-1 and 1-3 (p> 0.05) at the patients transferred endoscopic treatment or cystectomies. Duration of hospital staying of patients, taking to account the choice of organ-preserving operation is in the (Table 1).
Table 1: Duration of stationary stay of patients with SA-BC.
|
Operation option |
Number of SA-BC cases |
Duration of hospital stay (days) |
|
TURBT Open operations |
5 10 |
4,3±1,5 18±2,1 |
|
Probability |
|
< 0,01 |
Indications of duration for hospitalization at SA-BC lesions have been significantly less after TURBT, comparing with indications after "open" operations, that corresponds to results of similar researches in this direction. The nature of an operative intervention has been lower after organ-preserving interventions (Table 2).
Table 2: Duration of hospital stay of patients, depending on the volume of the performed operation.
|
Operation option |
Number of SA-BC cases |
Duration of hospital stay (days) |
||
|
А |
В |
А |
В |
|
|
TURBT Partial resection of the bladder Radical cystectomy |
- 1
23 |
5 9
- |
- 17,5±2,1
31,6±2,3 |
4,3±1,5 10,1±1,5
- |
The duration of the bed stay has been lower at patients of B group after organ-preserving operations, comparing with similar measure for A group (Table 2). Probably, it is explained by usage of endoscopic surgery in STH, reduction of time expenditure by carrying out primary diagnostics and centralization of medical care in STH of a regional hospital. Average duration of bed stay at patients after performance of radical surgical treatment (radical cystectomy) has been lower (for 9.5 bed days) after usage of a Mainz Pouch II technique.
Discussion
Complaints to gross hematuria are nonspecific manifestations of UGS at inhabitants of regions with a quite low level of UGS incidence that can be the reason of underestimation of the prevalence of this disease. According to A.M. Bronstein et al., gross hematuria indicates on UGS infection, and also as one of early clinical manifestations of a malignant new growth [5]. Microscopic detection of SH eggs remains “the gold standard” for diagnostics of UGS in concentrated urine by centrifugal ultrafiltration method [6]. However, this method is not always applicable in routine practice due to the lack of equipment in municipal hospitals of Angola and insufficient qualification of laboratory specialists: the eggs can be missed at light microscopy or are taken for other, little significant object at insignificant infection [7]. Usage of PCR and molecular markers for SH verification is available only in laboratories of the large regional centers [3].
Complex diagnostics of early lesions of an urothelium at UGS with usage of beam and endoscopic methods allows to verify SA-BC promptly in at patients of young age that has important social value [7]. Cystoscopic picture of UGS is very specific. Inflammatory, polyp-like and erythematic bilharzial lesions most often are located in the field of a dome and on a bladder sidewall, and specific "sandy patches" of an urothelium – around a neck of a bladder and ureteral isthmus [8]. The "random" biopsy of chronic ulcers of a bladder conducts after light cystoscopy, which coagulate or resect during a transurethral resection [9]. Conducting the TURBT allows to reduce expressiveness of the irritable symptoms and to stop a gross hematuria. Malignant regeneration of an urothelium at UGS often appears in a late stage at which as method of the choice serves only operation – a radical cystectomy.
The frequency of verification of bladder malignant damages in a locally-spread stage in B group has been significantly higher, than in A group, that is reflection of opportunities of active medical and diagnostic tactics. It has allowed to execute only organ-preserving operations by all patients of B group, thereby having improved the forecast and the further prospects of treatment of these patients. The combined usage of urine cytology, ultrasonography and cystoscopy at the expressed proliferative process caused by UGS allows to reveal SA-BC in early stages, subject to patient’s admission in STH of specialized medical institutions.
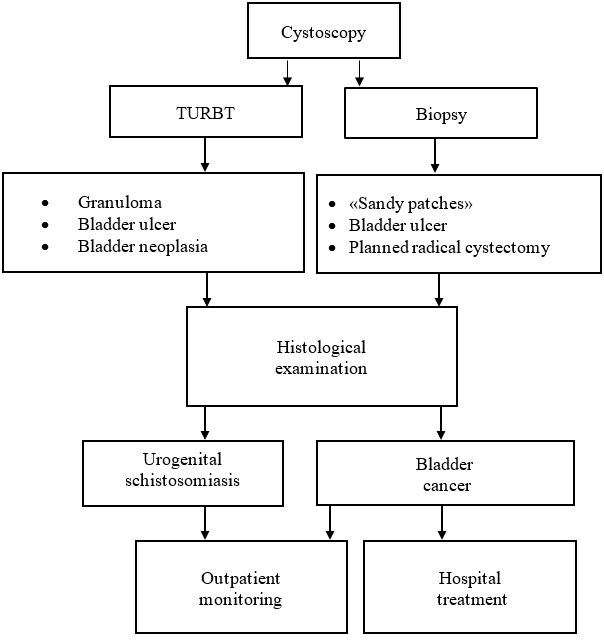
We have used the recommendations of the European association of urologists (EAU) for development of uniform indications to performance of TURBT, according to which operation is admissible in cases:
i. Endovesical proliferative inflammatory formations.
ii. Ulcerous lesions (performance of coagulation and a biopsy is allowed).
iii. Tumor new growth (without through perforation of a wall of a bladder, in cases of the planned radical cystectomy).
iv. "Sandy patches" can be subjected only to a biopsy [10].
The usage of endoscopic surgical interventions is applicable at identification of proliferative changes of an urothelium at UGS lesions, taking into account reliable decrease in number of complications and duration of patients staying in a hospital is expedient. The usage of endoscopic surgery at UGS defeated and at patients with early stages of SA-BC allows to verify most fully and low-invasive localization and volume of damage of a bladder that promotes the maintaining quality of patients’ life. Minimization of complications of the postoperative period after low-invasive interventions allows avoiding performance of "open" operative measures.
The quantity of complications at endoscopic operations at SA-BC lesions is defined by surgeon’s experience and, in a small number of cases, depends on a stage and the sizes of a new lesion. Endoscopic urological equipment of the day hospital base located in an endemic zone of schistosoma – is an important component of work of a urological hospital which employees provide medical care by the patient from the confirmed urinary system invasion of SH. According to the accepted indications, the medical and diagnostic algorithm used on the basis of STH (Figure 2) is created.
Figure 2: The algorithm used at delivery of health care by UGS lesions and SA-BC on the basis of short-term hospital.
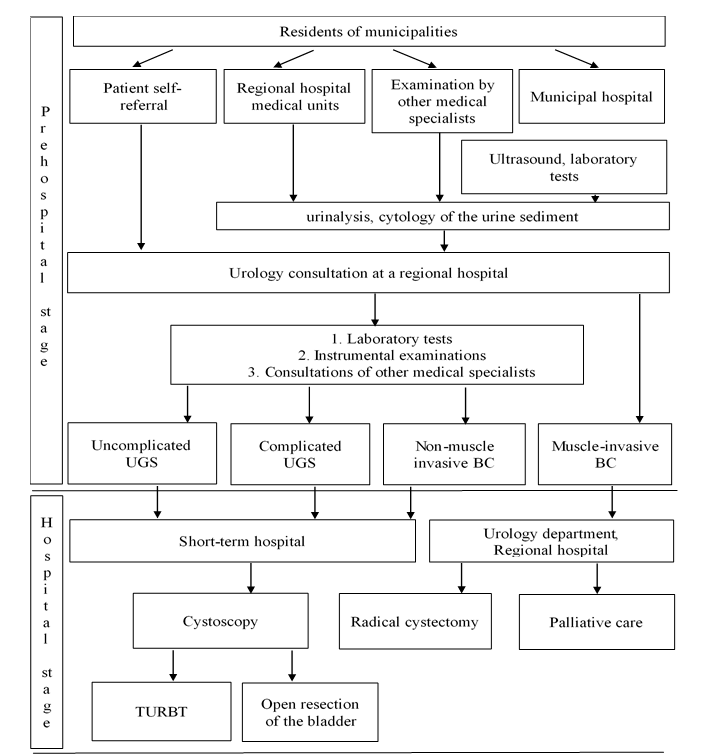
Figure 3: Algorithm of delivery of health care for UGS and SA-BC lesions.
In our opinion, the medical and diagnostic actions can be conditionally divided into three stages for optimization of identification of cases of SA-BC:
i. Pre-hospital inspection: Taking into account residence of most of patients in remote areas, the organization of laboratory and functional inspections and medical examination by specialists in the adopted standard is carried out in municipal hospitals. The patient is conducted the specialized examination in STH of regional hospital at the emergence of a gross hematuria;
ii. Hospital stage: Specialized medical care in urology departments of regional hospital;
iii. Rehabilitation stage: Dynamic observation and dispensary control of SA-BC lesions in medical institution at the place of residence. The algorithm of delivery of health care at pre-hospital and hospital stages is represented for UGS and SA-BC defeated in (Figure 3).
Conclusion
The absence of due consideration to a problem of UGS and uniform tactics of observation and treatment of UGS lesions at all stages may become the reason of late detection of a bladder malignant tumors. Preventive oral treatment by the Praziquantel does not solve a problem of treatment of SA-BC in an early stage.
The continuous sorting of the patients with a gross hematuria living in endemic regions, consisting in redistribution of patients in the medical institutions equipped with the necessary diagnostic equipment and the endoscopic operational equipment and also staffed with the qualified specialists urologists that will allow to diagnose and treat in due time proliferative changes of a urothelium is expedient.
The cytological analysis of urine sediment for detection of SH eggs is the most available diagnostic method, but it does not correspond to high diagnostic criteria. The medical and diagnostic algorithm at patients with UGS has to include carrying out cystoscopy and, according to indications, perform the TURB. The similar approach in treatment tactics of UGS allows us to verify SA-BC in early stages. It improves the forecast of a disease, keeps high quality of life for the young able-bodied citizen and solves a problem of prevention of the development of complications in malignant tumor cases.
Considering the probability of development of SA-BC during 10-15 from the moment of SH infection, stages of further observation and medical examination of this group of patients have to be standardized. The improvement of diagnostic methods of a tumor, in combination with modern medical approach at SA-BC lesions, plus introduction of observation system of patients at a stage of rehabilitation – will allow to make manageable of the oncological growth, caused by the development of an urinogenital schistosomiasis. Conducting the TURBT allows to reduce expressiveness of the irritable symptoms and to stop a gross hematuria schistosomiasis.
Consent
Informed consent was obtained from all participants. Additionally, the consent of the Local Ethics Committee was obtained.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 19, May 2020Accepted: Tue 02, Jun 2020
Published: Mon 08, Jun 2020
Copyright
© 2023 Vladimir Startsev. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2020.03.10
Author Info
Anton Yu. Kolmakov Faik R. Asfandiyarov Vasiliy I. Oriol Vladimir Startsev Vladimir S. Luchkevich
Corresponding Author
Vladimir StartsevSt. Petersburg State Pediatric Medical University, Russia
Figures & Tables
Table 1: Duration of stationary stay of patients with SA-BC.
|
Operation option |
Number of SA-BC cases |
Duration of hospital stay (days) |
|
TURBT Open operations |
5 10 |
4,3±1,5 18±2,1 |
|
Probability |
|
< 0,01 |
Table 2: Duration of hospital stay of patients, depending on the volume of the performed operation.
|
Operation option |
Number of SA-BC cases |
Duration of hospital stay (days) |
||
|
А |
В |
А |
В |
|
|
TURBT Partial resection of the bladder Radical cystectomy |
- 1
23 |
5 9
- |
- 17,5±2,1
31,6±2,3 |
4,3±1,5 10,1±1,5
- |
References
- IARC Monographs on the evaluation of carcinogenic risks to humans (2012) Biological Agents. IARC Monogr Eval Carcinog Risks Hum 100B: 35-44.
- WHO World Health Assembly Resolution WHA 54.19 Elimination of Schistosomiasis.
- Rashad S Barsoum (2013) Urinary Schistosomiasis: Review. J Adv Res 4: 453-459. [Crossref]
- Ramy Youssef, Payal Kapur, Wareef Kabbani, Shahrokh F Shariat, Ahmed Mosbah et al. (2011) Bilharzial vs non-bilharzial related bladder cancer: pathological characteristics and value of cyclooxygenase-2 expression. BJU Int 108: 31-37. [Crossref]
- Bronstein AM, Malyshev NA, Zharov SN (2012) Acute urogenital schistosomiasis in a tourist visiting Uganda and Kenya: a description of the case and a review of the literature [in Russian]. Epidemiology and infectious diseases : 47-50.
- Olumide Ajibola, Bashar Haruna Gulumbe, Anthonius Anayochukwu Eze, Emmanuel Obishakin (2018) Tools for Detection of Schistosomiasis in Resource Limited Settings. Med Sci (Basel) 6: 39. [Crossref]
- Stefanie Knopp, Sören L Becker, Katrin J Ingram, Jennifer Keiser, Jürg Utzinger (2013) Diagnosis and treatment of schistosomiasis in children in the era of intensified control. Expert Rev Anti-Infect Ther 11: 1237-1258. [Crossref]
- Kolmakov A, Startsev V (2014) Diagnosis and treatment of urinary schistosomiasis as pre-condition of bladder cancer. Eur Urol Suppl 13: e1164.
- Zaghloul MS (2012) Bladder cancer and schistosomiasis. Journal of the Egyptian National Cancer Institute 24: 151-159.
- Karl-Horst Bichler, Ilya Savatovsky, Kurt G Naber, Michael C Bischop, Truls E Bjerklund-Johansen et al. (2006) EAU Guidelines for the Management of Urogenital Schistosomiasis. Eur Urol 49: 998-1003. [Crossref]
