Onplant Use for Orthodontic Anchorage Reinforcement
A B S T R A C T
Introduction: In 1995, Block and Hoffman reported the successful use of a subperiosteal disk (onplant) to reinforce orthodontic anchorage in an experimental study in dogs and monkeys. It was concluded that onplants provide sufficient anchorage to successfully move and anchor teeth.
Aims: The aim of this article is to discuss the development of onplant, key design features, clinical indications for use as well as any available supporting evidence.
Methods: Review of the literature was carried out using the following search methods: MEDLINE and EMBASE. The search was focused on various keywords including: "onplant", "bone anchorage device" and "subperiosteal disk", which were conducted on studies published until January 2020.
Results: Evidence from clinical studies is scarce, a total of 9 related papers were retrieved from the literature (2 animal studies, 3 RCTs, 2 case series and 2 case reports). All types of study designs were included in the summary to maximize potential information gain.
Conclusion: In this article, we reviewed the development of onplant and outlined the general design features as well as specific design features. The onplant is no longer available in the market given that it never gained acceptance among the orthodontic community and its use is almost obsolete.
Keywords
Bone anchorage devices, onplant, orthodontic anchorage, subperiosteal disk
Introduction
Orthodontic anchorage can be defined as the prevention of unwanted tooth movement. Traditionally this was provided by anchor sites within the mouth (intraoral anchorage) or from outside the mouth (extraoral anchorage) [1]. Intraoral anchor sites include teeth or other oral structures. Extraoral anchorage is achieved by using headgear, neck straps or facemasks. Another method of reinforcing anchorage is the use of bone anchorage devices. Gainsforth and Higley first suggested the use of metallic screws as anchors back in 1945 [2]. Following that, Creekmore and Eklund inserted a similar device below the nasal cavity in 1983 [3]. In the late 90’s, Kanomi first described a miniscrew specifically designed for orthodontic use [4]. In the following year, Costa and colleagues described a screw with a special bracket-like head that could be used for either direct or indirect anchorage [5]. Around the same time, in the mid-nineties, Block and Hoffman described the successful use of an onplant, a subperiosteal disk, as an orthodontic anchorage device in an experimental study in dogs and monkeys [6]. Unlike miniscrews, onplants (as well as palatal implants) offer maximum anchorage by virtue of osseointegration and they can be removed after orthodontic treatment [6]. Onplants can be connected by transpalatal arches to move segments of teeth or in patients whose dental anchorage is insufficient because of tooth loss, hypodontia, or periodontal disease. Claimed benefits of onplants compared to palatal implants include elimination of the risk of perforating the nasal floor where vertical bone height is insufficient, and no restriction of insertion timing in terms of patients’ dental eruption stage to avoid unerupted or erupted teeth as no bony drilling is required [6, 7].
Development of the Onplant
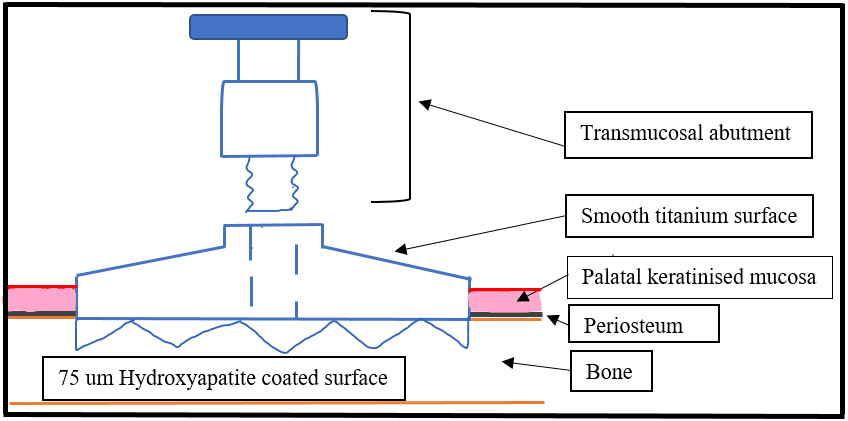
In 1989, Block and Hoffman designed a thin titanium alloy disk (onplant), textured and coated with hydroxyapatite (bioactive) on one surface and a threaded hole on the opposite side to be inserted subperiosteally with the hydroxyapatite-coated side against bone for biointegration (Figure 1). After approximately six years, the authors published their work after testing the onplant as absolute anchorage device for orthodontic movements in dogs and monkeys [6]. It was a relatively flat, disk-shaped fixture of 8-10 mm diameter and 3 mm thickness (Nobel Biocare, Gotenberg, Sweden) with a textured, hydroxyapatite-coated surface for integration with bone (Figure 1). Those authors showed that this new device could resist continuous forces up to 11 oz (3N) and concluded that onplants provide sufficient anchorage to successfully move and anchor teeth.
Figure 1: Schematic illustration of onplant. Superior smooth surface of onplant with internal thread for placement of transmucosal abutment and textured hydroxyapatite coated surface of onplant that is placed against bone for biointegration.
Method of Placement
Unlike implants, onplants require only simple surgical procedures to place and to remove, this makes them more versatile than implants as anchorage units in orthodontics. Furthermore, unlike implants, which are placed in freshly prepared bony sockets in alveolar bone, onplants are osseointegrated on relatively inactive bony surfaces. Onplants are surgically placed on the flat part of the palatal bone near the maxillary molar region. An incision is made in the palatal mucosa from the premolar area toward the midline. The tissue is tunnelled under, in full-thickness fashion, past the midline to the eventual implantation site (Figure 2).
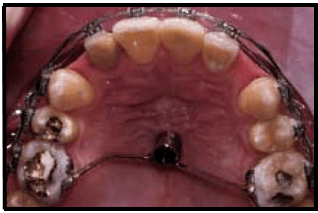
The onplant is then slipped under the soft tissue and brought into position, and the incision is sutured. A vacuum-formed stent is worn by the patient for approximately 10 days for the initial stabilisation and prevention of haematoma formation. After a healing period of up to 21 weeks, the cover screw on the onplant is exposed through a small incision (or tissue punch). The cover screw is removed, and the abutment is placed and fixed with an abutment screw. Once the onplant is exposed/uncovered, Transpalatal Arch (TPA) can be connected to gain anchorage reinforcement (Figure 3). To remove the onplant a second surgery is required to expose the bony surface and de-integrate the onplant.
Figure 2: A) Onplant incision and tissue elevation toward midline. B) Stage II of onplant procedure, with fixture exposed and impression coping screwed in and ready for open-tray impression. Reproduced with permission from Dr. Frank Celenza.
Figure 3: Transpalatal arch (TPA) connected to the onplant after a 12-week healing period. This system was utilised to reinforce anchorage in the anterioposterior plane during the retraction of the anterior labial segment. Reproduced with permission from Dr. Frank Celenza.
Supporting Evidence
A number of animal studies have reported successful use of onplant for provision of anchorage during orthodontic tooth movements. However, evidence from clinical studies is scarce, there are only few studies available in the literature that assessed the clinical effectiveness of this anchorage system (3 Randomized Controlled Trials [RCTs]). Table 1 shows a summary of the available evidence for onplant use, a total of 9 related papers were retrieved from the literature (2 animal studies, 3 RCTs, 2 case series and 2 case reports). All types of study designs were included in the summary to maximize potential information gain. Animal studies showed promising results initially [6, 10].
However, based on the clinical evidence available in the current literature, onplants did not provide adequate anchorage and were associated with high failure rates. The randomized controlled trial by Feldmann and Bondemark (2008) reported that onplant provides more reliable anchorage compared to conventional appliances such as headgear and TPA [8]. Feldmann et al. (2012) also studied patients’ perceptions of onplant in terms of pain and discomfort and concluded that this anchorage system is well accepted by patients in a long-time perspective [9]. Nevertheless, the evidence is quite limited.
Table 1: Supporting evidence regarding the use of onplant for orthodontic anchorage.
|
Authors (Year) |
Type of evidence |
Methodology |
Results/Conclusion |
|
Block and Hoffman (1995) [6]
|
Animal study |
Studied the effects of stabilising molars during incisors retraction. -Canine study: Four mongrel dogs were used. In each dog onplants were placed onto the palate. -Monkey study: Five monkeys were used in the study. One monkey served as a control, and the remaining four had one onplant placed in the middle of the palate opposite the maxillary second molar. |
“The onplant is sufficiently anchored to the underlying bone to withstand 11 ounces of continuous force. It is sufficiently anchored by the HA-bone biointegrated interface to resist up to 160 pounds of shear force. The onplant can provide absolute anchorage to move a tooth toward it without moving the onplant”. |
|
Chen et al. (2007) [10]
|
Animal study |
Sixteen rabbits were used in the study, and 3 onplants were placed on the calvaria of each rabbit (n=48). The rabbits were divided into 4 healing-period groups with 12 onplants in each group: 2, 4, 8, and 12 weeks. Bone blocks, each containing an onplant, were prepared for either histologic examination or biomechanical characterisation |
“The notion of loading onplants for orthodontic tooth movement as early as possible needs further clinical study for verification”. |
|
Feldmann et al. (2007) [11]
|
RCT |
A total of 120 adolescent patients were recruited and randomised into three groups. Group A underwent installation of an onplant, group B installation of an Orthosystem implant, and group C premolar extraction. Pain intensity and discomfort, analgesic consumption, limitations in daily activities, and functional jaw impairment were evaluated the first evening and one week after the intervention. |
“The Orthosystem implant was better tolerated than the onplant in terms of pain intensity, discomfort, and analgesic consumption and was, therefore, the anchorage system of choice in a short-term perspective”. |
|
Feldmann & Bondemark (2008) [8]
|
RCT |
A total of 120 patients were recruited and randomised into 4 anchorage systems: Onplant, Orthosystem implant, headgear, and transpalatal bar. The main outcome measures were cephalometric analysis of maxillary first molar and incisor movement, sagittal growth changes of the maxilla, and treatment time. |
“The Onplant and the Orthosystem implant groups had significantly higher success rates for anchorage than did the headgear and transpalatal bar groups. Compared with the Orthosystem implant, there were more technical problems with the Onplant”. |
|
Feldmann et al. (2012) [9]
|
RCT |
A total of 120 adolescent patients in order to start orthodontic treatment were consecutively recruited and randomised into three groups with different anchorage. Group A underwent installation of a skeletal anchorage (Onplant or Orthosystem implant), group B received headgear, and group C a transpalatal bar. |
“Very few significant differences between different anchorage groups in terms of perceived pain intensity, discomfort and jaw function impairment”. |
|
Heuberer et al. (2016) [12]
|
Case series |
Two Onplants were placed subperiosteally in the anterior part of the hard palate in five adult patients presenting a highly atrophic edentulous maxilla, class V or VI, according to Cawood and Howell. After a healing period of 4 months the prosthetic procedures were started. |
“Unexpectedly, the present study had to be discontinued due to the early loss of all 10 Onplants at the time of prosthetic loading. In total, 16 patients were meant to participate, but the study was stopped after complete failures of the first five patients”. |
|
Heuberer et al. (2011) [13]
|
Case series |
A surgical/prosthodontic approach was chosen for six patients with subtotal edentulism despite their young age. To support removable dentures the maxilla was treated with onplants (OnPlants), whereas dental root form implants (NobelReplaces, Nobel Biocare) were placed in the mandible. |
“While none of the root form implants was lost, one Onplant was lost and replaced with a stable outcome”. |
|
Hong et al. (2005) [14]
|
Case report |
A hexagonal onplant of 7.7 mm diameter was placed on the palatal bone of the maxilla in an 11-year five-month-old female patient with a Class III malocclusion and midface deficiency. Elastic traction (400 g per side) was applied from a facemask to the onplant at 30° to the occlusal plane 12 hours per day for 12 months. |
“These results suggest that Onplants can be used as an extremely stable anchorage for maxillary orthopedic facemask treatment”. |
|
Janssens et al. (2002) [7]
|
Case report |
Report the use of an onplant for palatal anchorage to extrude the unerupted horizontal maxillary first molars in a 12-year-old white girl with tooth aplasia and secondary cleft palate |
“After a healing period of 5 months, the Onplant remained stable under indirect elastic tension of approximately 160 g applied for 17 weeks, and the maxillary first molars were successfully extruded”. |
Problems with Onplant Use
When first described in the late 90’s, the onplant was a rather promising concept. With no drilling and bony preparation required, it seemed like a relatively simple device/auxiliary to place. However, soon after the Onplant® was produced and marketed by Nobel Biocare™, clinicians started realising that there were multiple shortcomings associated with onplant use. For instance, the surgical procedure for placement was not as simple as it was first thought, with the need for raising a full thickness mucoperiosteal palatal flap. Furthermore, the need for second stage surgical procedure to uncover the onplant, complicated the overall procedure. The delayed healing period of 10-21 weeks meant that immediate loading and commencement of anchorage utilisation was not possible. The high failure rate (failure to biointegrate) reported in some studies reflected the uncertainty in terms of success.
Availability of Onplants
The advent of other intraoral bone anchorage devices (miniscrews and palatal implants) caused a greater interest in utilising these devices instead, given the relative simplicity in placement and removal as compared to onplant. Since their introduction, orthodontic miniscrews have shifted the paradigm of anchorage in orthodontics and tooth movements that were once difficult have become easier [1]. Having searched the market and contacted the major orthodontic providers, it was concluded that the onplant is not available on the market anymore, to our knowledge. After temporarily producing and selling the Onplant®, Nobel Biocare™ have stopped providing/selling the product given that it never gained acceptance amongst the orthodontic community.
Conclusion
In this article, we reviewed the development of onplant and outlined the general design features as well as specific design features. Initially, the concept of utilising subperiosteal disks for orthodontic anchorage purposes was a promising one. However, few years after its introduction, the onplant is no longer available in the market given that it never gained acceptance among the orthodontic community and its use is almost obsolete.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Consent obtained for (Figures 2 & 3).
Availability of Data and Materials
Literature search available.
Competing Interests
None.
Author Contributions
Both authors prepared this manuscript.
Conflicts of Interest
None.
Acknowledgements
We would like to thank Dr. Frank Celenza for permitting the use of (Figures 2 & 3).
Article Info
Article Type
Review ArticlePublication history
Received: Sat 06, Jun 2020Accepted: Thu 18, Jun 2020
Published: Tue 23, Jun 2020
Copyright
© 2023 Aslam Alkadhimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDOA.2020.01.06
Author Info
Corresponding Author
Aslam AlkadhimiSpecialist Registrar, University College London, Eastman Dental Institute, London and Buckinghamshire Healthcare NHS Trust, London, UK
Figures & Tables
Table 1: Supporting evidence regarding the use of onplant for orthodontic anchorage.
|
Authors (Year) |
Type of evidence |
Methodology |
Results/Conclusion |
|
Block and Hoffman (1995) [6]
|
Animal study |
Studied the effects of stabilising molars during incisors retraction. -Canine study: Four mongrel dogs were used. In each dog onplants were placed onto the palate. -Monkey study: Five monkeys were used in the study. One monkey served as a control, and the remaining four had one onplant placed in the middle of the palate opposite the maxillary second molar. |
“The onplant is sufficiently anchored to the underlying bone to withstand 11 ounces of continuous force. It is sufficiently anchored by the HA-bone biointegrated interface to resist up to 160 pounds of shear force. The onplant can provide absolute anchorage to move a tooth toward it without moving the onplant”. |
|
Chen et al. (2007) [10]
|
Animal study |
Sixteen rabbits were used in the study, and 3 onplants were placed on the calvaria of each rabbit (n=48). The rabbits were divided into 4 healing-period groups with 12 onplants in each group: 2, 4, 8, and 12 weeks. Bone blocks, each containing an onplant, were prepared for either histologic examination or biomechanical characterisation |
“The notion of loading onplants for orthodontic tooth movement as early as possible needs further clinical study for verification”. |
|
Feldmann et al. (2007) [11]
|
RCT |
A total of 120 adolescent patients were recruited and randomised into three groups. Group A underwent installation of an onplant, group B installation of an Orthosystem implant, and group C premolar extraction. Pain intensity and discomfort, analgesic consumption, limitations in daily activities, and functional jaw impairment were evaluated the first evening and one week after the intervention. |
“The Orthosystem implant was better tolerated than the onplant in terms of pain intensity, discomfort, and analgesic consumption and was, therefore, the anchorage system of choice in a short-term perspective”. |
|
Feldmann & Bondemark (2008) [8]
|
RCT |
A total of 120 patients were recruited and randomised into 4 anchorage systems: Onplant, Orthosystem implant, headgear, and transpalatal bar. The main outcome measures were cephalometric analysis of maxillary first molar and incisor movement, sagittal growth changes of the maxilla, and treatment time. |
“The Onplant and the Orthosystem implant groups had significantly higher success rates for anchorage than did the headgear and transpalatal bar groups. Compared with the Orthosystem implant, there were more technical problems with the Onplant”. |
|
Feldmann et al. (2012) [9]
|
RCT |
A total of 120 adolescent patients in order to start orthodontic treatment were consecutively recruited and randomised into three groups with different anchorage. Group A underwent installation of a skeletal anchorage (Onplant or Orthosystem implant), group B received headgear, and group C a transpalatal bar. |
“Very few significant differences between different anchorage groups in terms of perceived pain intensity, discomfort and jaw function impairment”. |
|
Heuberer et al. (2016) [12]
|
Case series |
Two Onplants were placed subperiosteally in the anterior part of the hard palate in five adult patients presenting a highly atrophic edentulous maxilla, class V or VI, according to Cawood and Howell. After a healing period of 4 months the prosthetic procedures were started. |
“Unexpectedly, the present study had to be discontinued due to the early loss of all 10 Onplants at the time of prosthetic loading. In total, 16 patients were meant to participate, but the study was stopped after complete failures of the first five patients”. |
|
Heuberer et al. (2011) [13]
|
Case series |
A surgical/prosthodontic approach was chosen for six patients with subtotal edentulism despite their young age. To support removable dentures the maxilla was treated with onplants (OnPlants), whereas dental root form implants (NobelReplaces, Nobel Biocare) were placed in the mandible. |
“While none of the root form implants was lost, one Onplant was lost and replaced with a stable outcome”. |
|
Hong et al. (2005) [14]
|
Case report |
A hexagonal onplant of 7.7 mm diameter was placed on the palatal bone of the maxilla in an 11-year five-month-old female patient with a Class III malocclusion and midface deficiency. Elastic traction (400 g per side) was applied from a facemask to the onplant at 30° to the occlusal plane 12 hours per day for 12 months. |
“These results suggest that Onplants can be used as an extremely stable anchorage for maxillary orthopedic facemask treatment”. |
|
Janssens et al. (2002) [7]
|
Case report |
Report the use of an onplant for palatal anchorage to extrude the unerupted horizontal maxillary first molars in a 12-year-old white girl with tooth aplasia and secondary cleft palate |
“After a healing period of 5 months, the Onplant remained stable under indirect elastic tension of approximately 160 g applied for 17 weeks, and the maxillary first molars were successfully extruded”. |

References
- Alkadhimi A, Al Awadhi EA (2018) Miniscrews for orthodontic anchorage: a review of available systems. J Orthod 45: 102-114. [Crossref]
- Gainsforth BL, Higley LB (1945) A study of orthodontic anchorage possibilities in basal bone. Am J Orthod Oral Surg 31: 406-417.
- Creekmore TD, Eklund MK (1983) The possibility of skeletal anchorage. J Clin Orthod 17: 266-269. [Crossref]
- Kanomi R (1997) Mini-implant for orthodontic anchorage. J Clin Orthod 31: 763-767. [Crossref]
- Costa A, Raffainl M, Melsen B (1998) Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg 13: 201-209. [Crossref]
- Block MS, Hoffman DR (1995) A new device for absolute anchorage for orthodontics. Am J Orthod Dentofacial Orthop 107: 251-258. [Crossref]
- Janssens F, Swennen G, Dujardin T, Glineur R, Malevez C (2002) Use of an onplant as orthodontic anchorage. Am J Orthod Dentofacial Orthop 122: 566-570. [Crossref]
- Feldmann I, Bondemark L (2008) Anchorage capacity of osseointegrated and conventional anchorage systems: a randomized controlled trial. Am J Orthod Dentofacial Orthop 133: 339.e19-339.e28. [Crossref]
- Feldmann I, List T, Bondemark L (2012) Orthodontic anchoring techniques and its influence on pain, discomfort, and jaw function--a randomized controlled trial. Eur J Orthod 34: 102-108. [Crossref]
- Chen X, Chen G, He H, Peng C, Zhang T et al. (2007) Osseointegration and biomechanical properties of the onplant system. Am J Orthod Dentofacial Orthop 132: 278.e1-278.e6. [Crossref]
- Feldmann I (2007) Orthodontic anchorage--Evidence-based evaluation of anchorage capacity and patients' perceptions. Swed Dent J Suppl 10-86. [Crossref]
- Heuberer S, Ulm C, Zauza K, Zechner W, Watzek G et al. (2016) Effectiveness of subperiosteal bone anchor (Onplant) placement in the anterior highly atrophic maxilla for cross-arch prosthetic rehabilitation: Results from a pilot study. Eur J Oral Implantol 9: 291-297. [Crossref]
- Heuberer S, Dvorak G, Zauza K, Watzek G (2012) The use of onplants and implants in children with severe oligodontia: a retrospective evaluation. Clin Oral Implants Res 23: 827-831. [Crossref]
- Hong H, Ngan P, Han G, Qi LG, Wei SH (2005) Use of onplants as stable anchorage for facemask treatment: a case report. Angle Orthod 75: 453-460. [Crossref]
